High-density lipoprotein
High-density lipoprotein (HDL) is one of the five major groups of lipoproteins which, in order of sizes, largest to smallest, are chylomicrons, VLDL, IDL, LDL and HDL, which enable lipids like cholesterol and triglycerides to be transported within the water-based bloodstream. In healthy individuals, about thirty percent of blood cholesterol is carried by HDL.[1]
HDL particles containing cholesterol are termed HDL-C. It is often contrasted with low density or LDL cholesterol. HDL appears to be able to remove cholesterol from atheroma within arteries and transport it back to the liver for excretion or re-utilization, which is the main reason why HDL-C is sometimes called "good cholesterol". A high level of HDL-C does seem to protect against cardiovascular diseases, while low HDL cholesterol levels (less than 40 mg/dL or about 1 mmol/L) increase the risk for heart disease.[1]
Contents |
Structure and function
HDL is the smallest of the lipoprotein particles. They are the densest because they contain the highest proportion of protein. Their most abundant apolipoproteins are apo A-I and apo A-II.[2] The liver synthesizes these lipoproteins as complexes of apolipoproteins and phospholipid, which resemble cholesterol-free flattened spherical lipoprotein particles. They are capable of picking up cholesterol, carried internally, from cells by interaction with the ATP-binding cassette transporter A1 (ABCA1). A plasma enzyme called lecithin-cholesterol acyltransferase (LCAT) converts the free cholesterol into cholesteryl ester (a more hydrophobic form of cholesterol), which is then sequestered into the core of the lipoprotein particle, eventually making the newly synthesized HDL spherical. They increase in size as they circulate through the bloodstream and incorporate more cholesterol and phospholipid molecules from cells and other lipoproteins, for example by the interaction with the ABCG1 transporter and the phospholipid transport protein (PLTP).
HDL transports cholesterol mostly to the liver or steroidogenic organs such as adrenals, ovary, and testes by direct and indirect pathways. HDL is removed by HDL receptors such as scavenger receptor BI (SR-BI), which mediate the selective uptake of cholesterol from HDL. In humans, probably the most relevant pathway is the indirect one, which is mediated by cholesteryl ester transfer protein (CETP). This protein exchanges triglycerides of VLDL against cholesteryl esters of HDL. As the result, VLDLs are processed to LDL, which are removed from the circulation by the LDL receptor pathway. The triglycerides are not stable in HDL, but degraded by hepatic lipase so that finally small HDL particles are left, which restart the uptake of cholesterol from cells.
The cholesterol delivered to the liver is excreted into the bile and, hence, intestine either directly or indirectly after conversion into bile acids. Delivery of HDL cholesterol to adrenals, ovaries, and testes is important for the synthesis of steroid hormones.
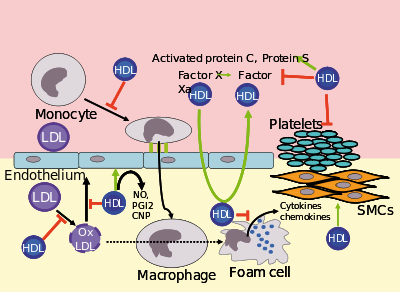
Several steps in the metabolism of HDL can contribute to the transport of cholesterol from lipid-laden macrophages of atherosclerotic arteries, termed foam cells, to the liver for secretion into the bile. This pathway has been termed reverse cholesterol transport and is considered as the classical protective function of HDL toward atherosclerosis.
However, HDL carries many lipid and protein species, several of which have very low concentrations but are biologically very active. For example, HDL and their protein and lipid constituents help to inhibit oxidation, inflammation, activation of the endothelium, coagulation, and platelet aggregation. All these properties may contribute to the ability of HDL to protect from atherosclerosis, and it is not yet known what are the most important.
In the stress response, serum amyloid A, which is one of the acute-phase proteins and an apolipoprotein, is under the stimulation of cytokines (IL-1, IL-6), and cortisol produced in the adrenal cortex and carried to the damaged tissue incorporated into HDL particles. At the inflammation site, it attracts and activates leukocytes. In chronic inflammations, its deposition in the tissues manifests itself as amyloidosis.
It has been postulated that the concentration of large HDL particles more accurately reflects protective action, as opposed to the concentration of total HDL particles.[3] This ratio of large HDL to total HDL particles varies widely and is measured only by more sophisticated lipoprotein assays using either electrophoresis (the original method developed in the 1970s) or newer NMR spectroscopy methods (See also: NMR and spectroscopy), developed in the 1990s.
Epidemiology
Men tend to have noticeably lower HDL levels, with smaller size and lower cholesterol content, than women. Men also have an increased incidence of atherosclerotic heart disease.
Epidemiological studies have shown that high concentrations of HDL (over 60 mg/dL) have protective value against cardiovascular diseases such as ischemic stroke and myocardial infarction. Low concentrations of HDL (below 40 mg/dL for men, below 50 mg/dL for women) increase the risk for atherosclerotic diseases.
Data from the landmark Framingham Heart Study showed that, for a given level of LDL, the risk of heart disease increases 10-fold as the HDL varies from high to low. On the converse, however, for a fixed level of HDL, the risk increases 3-fold as LDL varies from low to high.
Even people with very low LDL levels are exposed to increased risk if their HDL levels are not high enough.[4]
Estimating HDL associated cholesterol
Many laboratories used a two-step method: Chemical precipitation of lipoproteins containing apoprotein B, then calculating HDL associated cholesterol as the cholesterol remaining in the supernate,[5] but there are also direct methods.[6] Labs use the routine dextran sulfate-Mg2+ precipitation method with ultracentrifugation/dextran sulfate-Mg2+ precipitation as reference method.[7] HPLC can be used.[8]
Subfractions (HDL-2C, HDL-3C) can be measured [9] and have clinical significance.
Recommended ranges
The American Heart Association, NIH and NCEP provides a set of guidelines for fasting HDL levels and risk for heart disease.[10][11][12]
| Level mg/dL | Level mmol/L | Interpretation |
| <40 for men, <50 for women | <1.03 | Low HDL cholesterol, heightened risk for heart disease |
| 40–59 | 1.03–1.55 | Medium HDL level |
| >60 | >1.55 | High HDL level, optimal condition considered protective against heart disease |
Measuring HDL concentration and sizes
As technology has reduced costs and clinical trial have continued to demonstrate the importance of HDL, methods for directly measuring HDL concentrations, and size (which indicates function) at lower costs have become increasingly available and regarded as more important for assessing individual risk for progressive arterial disease and improve treatment methods.
Chemical measurements
HDL, as discussed above, forms from two large proteins, predominantly apo A-I and apo A-II, positioned, back to back. Charged amino acids on the outer surface attract water, making the particles both water soluble (so as to carry fats within the blood) and able to associate with HDL receptors on in the surface of cells, e.g. the macrophages of which plaque is predominantly composed, at least in the early stages. Cholesterol is carried within and between the two particles. If the particles pick up more cholesterol, then the particles enlarge and a third or fourth Apo A protein joins the grouping, termed large HDL. Since the predominant protein is Apo A-I, then chemical measurements can be used to estimate HDL concentrations present in a blood sample, though such measurements may not indicate how well the HDL particles are functioning to reverse transport cholesterol from tissues.
Electrophoresis measurements
Since the HDL particles have a net negative charge and vary by size, electrophoresis measurements have been utilized since the 1960s to both indicate the number of HDL particles and additionally sort them by size, thus presumably function. Small HDL particles are not carrying much, larger HDL particles are carrying more cholesterol.
NMR measurements
The newest methodology for measuring HDL particles, available clinically since the late 1990s[1] uses Nuclear Magnetic Resonance fingerprinting of the particles to measure both concentration and sizes. This methodology has significantly reduced costs and made such determinations more widely available clinically.
Optimal Total and Large HDL concentrations
The HDL particle concentrations are typically categorized by event rate percentiles based on the people participating and being tracked in the MESA[2] trial, a medical research study sponsored by the United States National Heart, Lung, and Blood Institute.
| MESA Percentile | Total HDL particles μmol/L | Interpretation |
|---|---|---|
| >75% | >34.9 | Those with highest (Optimal) total HDL particle concentrations & lowest rates of cardiovascular disease events |
| 50–75% | 30.5–34.5 | Those with moderately high total HDL particle concentrations & moderate rates of cardiovascular disease events |
| 25–50% | 26.7–30.5 | Those with lower total HDL particle concentrations & Borderline-High rates of cardiovascular disease |
| 0–25% | <26.7 | Those with lowest total HDL particle concentrations & Highest rates of cardiovascular disease events |
| MESA Percentile | Large HDL particles μmol/L | Interpretation |
|---|---|---|
| >75% | >7.3 | Those with highest (Optimal) Large HDL particle concentrations & lowest rates of cardiovascular disease events |
| 50–75% | 4.8–7.3 | Those with moderately high Large HDL particle concentrations & moderate rates of cardiovascular disease events |
| 25–50% | 3.1–4.8 | Those with lower Large HDL particle concentrations & Borderline-High rates of cardiovascular disease |
| 0–25% | <3.1 | Those with lowest Large HDL particle concentrations & Highest rates of cardiovascular disease events |
The lowest incidence of atherosclerotic events over time occurs within those with both the highest concentrations of total HDL particles, the top quarter (>75%), and the highest concentrations of large HDL particle concentrations. Multiple other measures, including LDL particle concentrations, small LDL particle concentrations, along with VLDL concentrations, estimations of Insulin resistance pattern and standard cholesterol lipid measurements (for comparison of the plasma data with the estimation methods discussed above) are also routinely provided.
Memory
A link has been shown between level of HDL and onset of dementia. Those with high HDL were less likely to have dementia.[13] Low HDL-C in late-middle age has also been associated with memory loss.[14]
Raising HDL
Diet and lifestyle
Certain changes in lifestyle can have a positive impact on raising HDL levels:[15]
- Aerobic exercise[16]
- Weight loss[17]
- Smoking cessation[17]
- Removing trans fatty acids from the diet[18]
- Mild to moderate alcohol intake[17] HDL transports cholesterol to the liver and cholesterol is known to have a protective effect on the cell membrane. It is likely that this reflects the liver's need for more cholesterol to protect itself from the alcohol.[19]
- Adding soluble fiber to diet
- Using supplements such as omega 3 fish oil[20] or flax oil
- Increasing intake of cis-unsaturated fats[21] and cholesterol, decreasing intake of trans-fats.
- Avoiding supplements that contain omega 6 (Omega 6 reduces cholesterol but does not discriminate between good and bad cholesterol) as well as limiting foods high in omega 6 (tilapia, most vegetable oils, nuts)
A very-low-carbohydrate diet involving ketogenesis may have similar response to taking niacin as described above (lowered LDL and increased HDL) through beta-hydroxybutyrate coupling the Niacin receptor 1.[22]
Drugs
Pharmacological therapy to increase the level of HDL cholesterol includes use of fibrates and niacin. Fibrates, however, have shown that they have no effect on overall deaths from all causes, despite their effects on lipids.[23]
Niacin (B3), increases HDL by selectively inhibiting hepatic Diacylglycerol acyltransferase 2, reducing triglyceride synthesis and VLDL secretion through a receptor HM74[24] otherwise known as Niacin receptor 2 and HM74A / GPR109A,[22] Niacin receptor 1.
Pharmacologic (1- to 3-gram) doses increase HDL levels by 10–30%,[25] making it the most powerful agent to increase HDL-cholesterol.[26][27] A randomized clinical trial demonstrated that treatment with niacin can significantly reduce atherosclerosis progression and cardiovascular events.[28] However, niacin products sold as "no-flush", i.e. not having side-effects such as "niacin flush", do not contain free nicotinic acid and are therefore ineffective at raising HDL, while products sold as "sustained-release" may contain free nicotinic acid, but "some brands are hepatotoxic"; therefore the recommended form of niacin for raising HDL is the cheapest, immediate-release preparation.[29] Both fibrates and niacin increase artery toxic homocysteine, an effect that can be counteracted by also consuming a multivitamin with relatively high amounts of the B-vitamins.
In contrast, while the use of statins is effective against high levels of LDL cholesterol, it has little or no effect in raising HDL cholesterol.[26]
Torcetrapib, a drug developed by Pfizer to raise HDL by inhibition of cholesteryl ester transfer protein (CETP), was terminated after a greater percentage of patients treated with torcetrapib-Lipitor combination died compared with patients treated with Lipitor alone. Merck is currently researching a similar molecule called anacetrapib.
See also
- Asymmetric dimethylarginine
- Cardiovascular disease
- Endothelium
- Low-density lipoprotein
Footnotes
- ↑ 1.0 1.1 "LDL and HDL Cholesterol: What's Bad and What's Good?". American Heart Association. July 2, 2009. http://www.americanheart.org/presenter.jhtml?identifier=180. Retrieved October 8, 2009.
- ↑ Després, Jean-Pierre. "The Atherogenic Triad of New Metabolic Risk Factors: Importance of Waist and Fasting Triglycerides as Screening Tools". Visceral Adipose Tissue and Cardiometabolic Risk: Does It Really Matter? Part 2. http://www.lipidsonline.org/slides/slide01.cfm?q=apolipoprotein&dpg=59. Retrieved October 8, 2009.
- ↑ PMID 11374859 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Barter, Philip; Gotto, Antonio M.; LaRosa, John C.; Maroni, Jaman; Szarek, Michael; Grundy, Scott M.; Kastelein, John J. P.; Bittner, Vera et al. (2007). "HDL Cholesterol, Very Low Levels of LDL Cholesterol, and Cardiovascular Events". New England Journal of Medicine 357 (13): 1301. doi:10.1056/NEJMoa064278. PMID 17898099.
- ↑ Lin, Maun-Jan; Hoke, Carolyn; Ettinger, Bruce (1998). "Evaluation of Homogeneous High-Density Lipoprotein Cholesterol Assay on a BM/Hitachi 747-200 Analyzer". Clinical Chemistry 44 (5): 1050. PMID 9590383. http://www.clinchem.org/cgi/content/short/44/5/1050.
- ↑ "Lipid Measurement Fact Sheet". University of Michigan Health System. http://www.med.umich.edu/mdrtc/cores/ChemCore/lipids.htm. Retrieved October 8, 2009.
- ↑ Bairaktari, E; Elisaf, M; Katsaraki, A; Tsimihodimos, V; Tselepis, AD; Siamopoulos, KC; Tsolas, O (1999). "Homogeneous HDL-cholesterol assay versus ultracentrifugation/dextran sulfate-Mg2+ precipitation and dextran sulfate-Mg2+ precipitation in healthy population and in hemodialysis patients". Clinical Biochemistry 32 (5): 339. doi:10.1016/S0009-9120(99)00031-4. PMID 10480448.
- ↑ Okazaki, Mitsuyo; Sasamoto, Keiko; Muramatsu, Toshio; Hosaki, Seijin (1997). "Evaluation of precipitation and direct methods for HDL-cholesterol assay by HPLC". Clinical Chemistry 43 (10): 1885. PMID 9342008. http://www.clinchem.org/cgi/content/abstract/43/10/1885.
- ↑ Hirano, Tsutomu; Nohtomi, Kyoko; Koba, Shinji; Muroi, Ayako; Ito, Yasuki (2008). "A simple and precise method for measuring HDL-cholesterol subfractions by a single precipitation followed by homogenous HDL-cholesterol assay". The Journal of Lipid Research 49: 1130. doi:10.1194/jlr.D700027-JLR200.
- ↑ "Cholesterol Levels". American Heart Association. http://www.americanheart.org/presenter.jhtml?identifier=4500. Retrieved November 14, 2009.
- ↑ "What Do My Cholesterol Levels Mean?" (PDF). American Heart Association. September 2007. http://www.americanheart.org/downloadable/heart/119618151049911%20CholLevels%209_07.pdf. Retrieved November 14, 2009.
- ↑ "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Executive Summary". National Heart, Lung, and Blood Institute (NHLBI). National Institutes of Health. May 2001. http://www.nhlbi.nih.gov/guidelines/cholesterol/atp3xsum.pdf.
- ↑ Nagourney, Eric (July 1, 2008). "Aging: Good Cholesterol, Good Memory". The New York Times. http://www.nytimes.com/2008/07/01/health/research/01agin.html. Retrieved October 8, 2009.
- ↑ Singh-manoux, A; Gimeno, D; Kivimaki, M; Brunner, E; Marmot, MG (2008). "Low HDL cholesterol is a risk factor for deficit and decline in memory in midlife: the Whitehall II study". Arteriosclerosis, thrombosis, and vascular biology 28 (8): 1556–62. doi:10.1161/ATVBAHA.108.163998. PMID 18591462.
- ↑ Fogoros, Richard N. (September 15, 2009). "Raising Your HDL Levels". About.com. http://heartdisease.about.com/cs/cholesterol/a/raiseHDL.htm. Retrieved October 8, 2009.
- ↑ Spate-douglas, T; Keyser, RE (1999). "Exercise intensity: its effect on the high-density lipoprotein profile". Archives of physical medicine and rehabilitation 80 (6): 691–5. doi:10.1016/S0003-9993(99)90174-0. PMID 10378497.
- ↑ 17.0 17.1 17.2 Hausenloy DJ, Yellon DM (June 2008). "Targeting residual cardiovascular risk: raising high-density lipoprotein cholesterol levels". Heart 94 (6): 706–14. doi:10.1136/hrt.2007.125401. PMID 18480348.
- ↑ "Trans fat: Avoid this cholesterol double whammy". Mayo Foundation for Medical Education and Research (MFMER). http://www.mayoclinic.com/health/trans-fat/CL00032. Retrieved 2010-06-25.
- ↑ Weidner, G; Connor, SL; Chesney, MA; Burns, JW; Connor, WE; Matarazzo, JD; Mendell, NR (1991). "Sex differences in high density lipoprotein cholesterol among low-level alcohol consumers". Circulation 83 (1): 176–80. PMID 1984880. http://circ.ahajournals.org/cgi/reprint/83/1/176.pdf.
- ↑ "The Power of Fish". The Cleveland Clinic Heart and Vascular Institute. http://my.clevelandclinic.org/heart/prevention/nutrition/omega3.aspx. Retrieved October 8, 2009.
- ↑ Mensink, Ronald P.; Zock, Peter L.; Kester, Arnold D. M.; Katan, Martijn B. (2003). "Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials". American Journal of Clinical Nutrition 77 (5): 1146. PMID 12716665. http://www.ajcn.org/cgi/content/abstract/77/5/1146.
- ↑ 22.0 22.1 Soudijn, W; Van Wijngaarden, I; Ijzerman, AP (2007). "Nicotinic acid receptor subtypes and their ligands". Medicinal research reviews 27 (3): 417–33. doi:10.1002/med.20102. PMID 17238156.
- ↑ Benatar, JR; Stewart, RA (2007). "Is it time to stop treating dyslipidaemia with fibrates?". The New Zealand medical journal 120 (1261): U2706. PMID 17853928. http://www.nzma.org.nz/journal/120-1261/2706/.
- ↑ Meyers, CD; Kamanna, VS; Kashyap, ML (2004). "Niacin therapy in atherosclerosis". Current opinion in lipidology 15 (6): 659–65. doi:10.1097/00041433-200412000-00006. PMID 15529025.
- ↑ Rader, Daniel J. (2004). "Raising HDL in Clinical Practice". Raising HDL in Clinical Practice: Clinical Strategies to Elevate HDL. http://cme.medscape.com/viewarticle/479499_5. Retrieved October 8, 2009.
- ↑ 26.0 26.1 Brewer, H. Bryan (December 27, 2005). "Raising HDL-Cholesterol and Reducing Cardiovascular Risk: An Expert Interview With H. Bryan Brewer, Jr, MD". http://cme.medscape.com/viewarticle/520393. Retrieved October 8, 2009.
- ↑ Chapman, M. John; Assmann, Gerd; Fruchart, Jean-Charles; Shepherd, James; Sirtori, Cesare; European Consensus Panel on HDL-C (2004). "Raising high-density lipoprotein cholesterol with reduction of cardiovascular risk: the role of nicotinic acid – a position paper developed by the European Consensus Panel on HDL-C". Current medical research and opinion 20 (8): 1253–68. doi:10.1185/030079904125004402. PMID 15324528.
- ↑ Drexel, H. (2006). "Reducing risk by raising HDL-cholesterol: the evidence". European Heart Journal Supplements 8: F23. doi:10.1093/eurheartj/sul037.
- ↑ Meyers, C. Daniel; Carr, Molly C.; Park, Sang; Brunzell, John D. (2003). "Varying Cost and Free Nicotinic Acid Content in Over-the-Counter Niacin Preparations for Dyslipidemia". Annals of Internal Medicine 139 (12): 996. PMID 14678919. http://www.annals.org/cgi/content/abstract/139/12/996.
External links
|
||||||||||||||||||||||||||
