Cannabinoid
|
Cannabinoid is a generic term for 1. phytocannabinoids, compounds found in the Cannabis plant that are structurally related to tetrahydrocannabinol (THC), 2. endocannabinoids that are found in the nervous and immune systems of animals and that activate cannabinoid receptors , and 3. synthetic cannabinoids, a structurally diverse class of mostly synthetic substances that bind to cannabinoid receptors. The latter group encompasses a variety of distinct chemical classes: the classical cannabinoids structurally related to THC, the nonclassical cannabinoids including the aminoalkylindoles, 1,5-diarylpyrazoles, quinolines and arylsulphonamides, as well as eicosanoids related to the endocannabinoids.[1]
Cannabinoid receptors
Before the 1980s, it was often speculated that cannabinoids produced their physiological and behavioral effects via nonspecific interaction with cell membranes, instead of interacting with specific membrane-bound receptors. The discovery of the first cannabinoid receptors in the 1980s helped to resolve this debate. These receptors are common in animals, and have been found in mammals, birds, fish, and reptiles. At present, there are two known types of cannabinoid receptors, termed CB1 and CB2, with mounting evidence of more.[2]
Cannabinoid receptor type 1
CB1 receptors are found primarily in the brain, to be specific in the basal ganglia and in the limbic system, including the hippocampus. They are also found in the cerebellum and in both male and female reproductive systems. CB1 receptors are absent in the medulla oblongata, the part of the brain stem responsible for respiratory and cardiovascular functions. Thus, there is not a risk of respiratory or cardiovascular failure as there is with many other drugs. CB1 receptors appear to be responsible for the euphoric and anticonvulsive effects of cannabis.
Cannabinoid receptor type 2
CB2 receptors are almost exclusively found in the immune system, with the greatest density in the spleen. While found only in the peripheral nervous system, a report does indicate that CB2 is expressed by a subpopulation of microglia in the human cerebellum [3]. CB2 receptors appear to be responsible for the anti-inflammatory and possibly other therapeutic effects of cannabis.
Phytocannabinoids
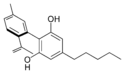
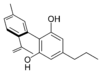
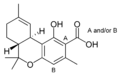
| Type | Skeleton | Cyclization |
|---|---|---|
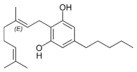
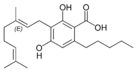
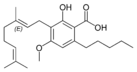
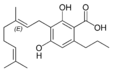
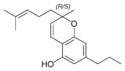
| Cannabigerol-type CBG |
 |
 |
| Cannabichromene-type CBC |
 |
 |
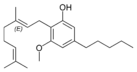
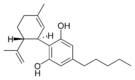
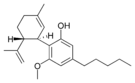
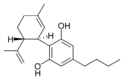
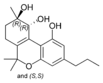
| Cannabidiol-type CBD |
 |
 |
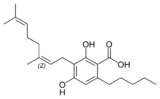
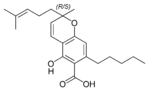
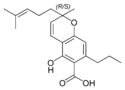
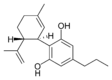
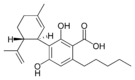
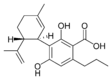
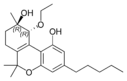
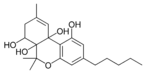
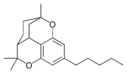
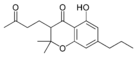
| Tetrahydrocannabinol- and Cannabinol-type THC, CBN |
 |
 |
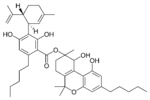
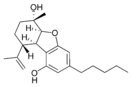
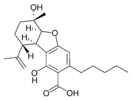
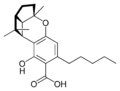
| Cannabielsoin-type CBE |
 |
 |
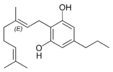
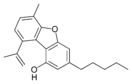
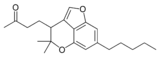
| iso- Tetrahydrocannabinol- type iso-THC |
 |
 |
| Cannabicyclol-type CBL |
 |
 |
| Cannabicitran-type CBT |
 |
 |
| Main classes of natural cannabinoids | ||
Phytocannabinoids, also called natural cannabinoids, herbal cannabinoids, and classical cannabinoids, are only known to occur naturally in significant quantity in the cannabis plant, and are concentrated in a viscous resin that is produced in glandular structures known as trichomes. In addition to cannabinoids, the resin is rich in terpenes, which are largely responsible for the odour of the cannabis plant.
Phytocannabinoids are nearly insoluble in water but are soluble in lipids, alcohols, and other non-polar organic solvents. However, as phenols, they form more water-soluble phenolate salts under strongly alkaline conditions.
All-natural cannabinoids are derived from their respective 2-carboxylic acids (2-COOH) by decarboxylation (catalyzed by heat, light, or alkaline conditions).
Types
At least 66 cannabinoids have been isolated from the cannabis plant[4][5] To the right the main classes of natural cannabinoids are shown. All classes derive from cannabigerol-type compounds and differ mainly in the way this precursor is cyclized.
Tetrahydrocannabinol (THC), cannabidiol (CBD) and cannabinol (CBN) are the most prevalent natural cannabinoids and have received the most study. Other common cannabinoids are listed below:
- CBG Cannabigerol
- CBC Cannabichromene
- CBL Cannabicyclol
- CBV Cannabivarin
- THCV Tetrahydrocannabivarin
- CBDV Cannabidivarin
- CBCV Cannabichromevarin
- CBGV Cannabigerovarin
- CBGM Cannabigerol Monoethyl Ether
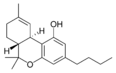
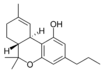
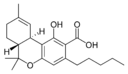
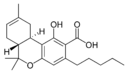
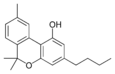
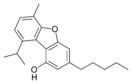
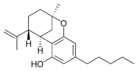
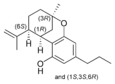
Tetrahydrocannabinol
Tetrahydrocannabinol (THC) is the primary psychoactive component of the plant. It appears to ease moderate pain (analgetic) and to be neuroprotective. THC has approximately equal affinity for the CB1 and CB2 receptors.[6] Its effects are perceived to be more cerebral.
Delta-9-Tetrahydrocannabinol (Δ9-THC, THC) and delta-8-tetrahydrocannabinol (Δ8-THC), mimic the action of anandamide, a neurotransmitter produced naturally in the body. The THCs produce the high associated with cannabis by binding to the CB1 cannabinoid receptors in the brain.
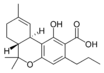
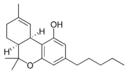
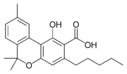
Cannabidiol
Cannabidiol (CBD) is not psychoactive, and was thought not to affect the psychoactivity of THC.[7] However, recent evidence shows that smokers of cannabis with a higher CBD/THC ratio were less likely to experience schizophrenia-like symptoms.[8] This is supported by psychological tests, in which participants experience less intense psychotic effects when intravenous THC was co-administered with CBD (as measured with a PANSS test).[9] It has been hypothesized that CBD acts as an allosteric antagonist at the CB1 receptor and thus alters the psychoactive effects of THC.
It appears to relieve convulsion, inflammation, anxiety, and nausea.[10] CBD has a greater affinity for the CB2 receptor than for the CB1 receptor.[10]
CBD shares a precursor with THC and is the main cannabinoid in low-THC Cannabis strains.
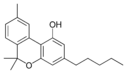
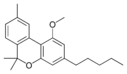
Cannabinol
Cannabinol (CBN) is the primary product of THC degradation, and there is usually little of it in a fresh plant. CBN content increases as THC degrades in storage, and with exposure to light and air. It is only mildly psychoactive. Its affinity to the CB2 receptor is higher than for the CB1 receptor.[11]
Cannabigerol
Cannabigerol (CBG) is non-psychotomimetic but still affects the overall effects of Cannabis. It acts as an α2-adrenergic receptor agonist, 5-HT1A receptor antagonist, and CB1 receptor antagonist.[12] It also binds to the CB2 receptor.[12]
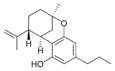
Tetrahydrocannabivarin
Tetrahydrocannabivarin (THCV) is prevalent in certain South African and Southeast Asian strains of Cannabis. It is an antagonist of THC at CB1 receptors and attenuates the psychoactive effects of THC.[13]
Cannabichromene
Cannabichromene (CBC) is non-psychoactive and does not affect the psychoactivity of THC [7].
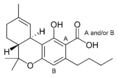
Double bond position
In addition, each of the compounds above may be in different forms depending on the position of the double bond in the alicyclic carbon ring. There is potential for confusion because there are different numbering systems used to describe the position of this double bond. Under the dibenzopyran numbering system widely used today, the major form of THC is called Δ9-THC, while the minor form is called Δ8-THC. Under the alternate terpene numbering system, these same compounds are called Δ1-THC and Δ6-THC, respectively.
Length
Most herbal cannabinoid compounds are 21-carbon compounds. However, some do not follow this rule, primarily because of variation in the length of the side-chain attached to the aromatic ring. In THC, CBD, and CBN, this side-chain is a pentyl (5-carbon) chain. In the most common homologue, the pentyl chain is replaced with a propyl (3-carbon) chain. Cannabinoids with the propyl side-chain are named using the suffix varin, and are designated, for example, THCV, CBDV, or CBNV.
Plant profile
Cannabis plants can exhibit wide variation in the quantity and type of cannabinoids they produce. The mixture of cannabinoids produced by a plant is known as the plant's cannabinoid profile. Selective breeding has been used to control the genetics of plants and modify the cannabinoid profile. For example, strains that are used as fiber (commonly called hemp) are bred such that they are low in psychoactive chemicals like THC. Strains used in medicine are often bred for high CBD content, and strains used for recreational purposes are usually bred for high THC content or for a specific chemical balance. Some strains of more than 20% THC in their flowering buds have been created.
Quantitative analysis of a plant's cannabinoid profile is usually determined by gas chromatography (GC), or more reliably by gas chromatography combined with mass spectrometry (GC/MS). Liquid chromatography (LC) techniques are also possible, although these are often only semi-quantitative or qualitative. There have been systematic attempts to monitor the cannabinoid profile of cannabis over time, but their accuracy is impeded by the illegal status of the plant in many countries.
Pharmacology
Cannabinoids can be administered by smoking, vaporizing, oral ingestion, transdermal patch, intravenous injection, sublingual absorption, or rectal suppository. Once in the body, most cannabinoids are metabolized in the liver, especially by cytochrome P450 mixed-function oxidases, mainly CYP 2C9. Thus supplementing with CYP 2C9 inhibitors leads to extended intoxication.
Some is also stored in fat in addition to being metabolized in liver. Δ9-THC is metabolized to 11-hydroxy-Δ9-THC, which is then metabolized to 9-carboxy-THC. Some cannabis metabolites can be detected in the body several weeks after administration.
Plant synthesis
Cannabinoid production starts when an enzyme causes geranyl pyrophosphate and olivetolic acid to combine and form CBG. Next, CBG is independently converted to either CBD or CBC by two separate synthase enzymes. CBD is then enzymatically cyclized to THC. For the propyl homologues (THCV, CBDV and CBNV), there is a similar pathway that is based on CBGV.
Separation
Cannabinoids can be separated from the plant by extraction with organic solvents. Hydrocarbons and alcohols are often used as solvents. However, these solvents are flammable and many are toxic. Supercritical solvent extraction with carbon dioxide is an alternative technique. Although this process requires high pressures (73 atmospheres or more), there is minimal risk of fire or toxicity, solvent removal is simple and efficient, and extract quality can be well-controlled. Once extracted, cannabinoid blends can be separated into individual components using wiped film vacuum distillation or other distillation techniques. However, to produce high purity cannabinoids, chemical synthesis or semisynthesis is generally required.
History
Cannabinoids were first discovered in the 1940s, when CBD and CBN were identified. The structure of THC was first determined in 1964.
Due to molecular similarity and ease of synthetic conversion, CBD was originally believed to be a natural precursor to THC. However, it is now known that CBD and THC are produced independently in the cannabis plant.
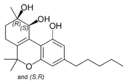
Endocannabinoids

Endocannabinoids are substances produced from within the body that activate cannabinoid receptors. After the discovery of the first cannabinoid receptor in 1988, scientists began searching for an endogenous ligand for the receptor.
Types of endocannabinoid ligands
- Arachidonoylethanolamine (Anandamide or AEA)
In 1992, in Raphael Mechoulam's Israeli lab, the first such compound was identified as arachidonoyl ethanolamine and named anandamide, a name derived from the Sanskrit word for bliss and -amide. Anandamide is derived from the essential fatty acid arachidonic acid. It has a pharmacology similar to THC, although its chemical structure is different. Anandamide binds to the central (CB1) and, to a lesser extent, peripheral (CB2) cannabinoid receptors, where it acts as a partial agonist. Anandamide is about as potent as THC at the CB1 receptor.[14] It is found in nearly all tissues in a wide range of animals.[15]
Two analogs of anandamide, 7,10,13,16-docosatetraenoylethanolamide and homo-γ-linolenoylethanolamine, have similar pharmacology. All of these are members of a family of signalling lipids called N-acylethanolamides, which also includes the noncannabimimetic palmitoylethanolamide and oleoylethanolamine, which possess anti-inflammatory and orexigenic effects, respectively. Many N-acylethanolamines have also been identified in plant seeds[16] and in molluscs.[17]
- 2-arachidonoyl glycerol (2-AG)
Another endocannabinoid, 2-arachidonoyl glycerol, binds to both the CB1 and CB2 receptors with similar affinity, acting as a full agonist at both.[14] 2-AG is present at significantly higher concentrations in the brain than anandamide[18], and there is some controversy over whether 2-AG rather than anandamide is chiefly responsible for endocannabinoid signalling in vivo[19]. In particular, one in vitro study suggests that 2-AG is capable of stimulating higher G-protein activation than anandamide, although the physiological implications of this finding are not yet known.[20]
- 2-arachidonyl glyceryl ether (noladin ether)
In 2001, a third, ether-type endocannabinoid, 2-arachidonyl glyceryl ether (noladin ether), was isolated from porcine brain. [21] Prior to this discovery, it had been synthesized as a stable analog of 2-AG; indeed, some controversy remains over its classification as an endocannabinoid, as another group failed to detect the substance at "any appreciable amount" in the brains of several different mammalian species.[22] It binds to the CB1 cannabinoid receptor (Ki = 21.2 nmol/L) and causes sedation, hypothermia, intestinal immobility, and mild antinociception in mice. It binds primarily to the CB1 receptor, and only weakly to the CB2 receptor.[14]
- N-arachidonoyl-dopamine (NADA)
Discovered in 2000, NADA preferentially binds to the CB1 receptor.[23] Like anandamide, NADA is also an agonist for the vanilloid receptor subtype 1 (TRPV1), a member of the vanilloid receptor family.[24][25]
- Virodhamine (OAE)
A fifth endocannabinoid, virodhamine, or O-arachidonoyl-ethanolamine (OAE), was discovered in June 2002. Although it is a full agonist at CB2 and a partial agonist at CB1, it behaves as a CB1 antagonist in vivo. In rats, virodhamine was found to be present at comparable or slightly lower concentrations than anandamide in the brain, but 2- to 9-fold higher concentrations peripherally.[26]
Function
Endocannabinoids serve as intercellular 'lipid messengers', signaling molecules that are released from one cell and activating the cannabinoid receptors present on other nearby cells. Although in this intercellular signaling role they are similar to the well-known monoamine neurotransmitters, such as acetylcholine and dopamine, endocannabinoids differ in numerous ways from them. For instance, they use retrograde signaling. Furthermore, endocannabinoids are lipophilic molecules that are not very soluble in water. They are not stored in vesicles, and exist as integral constituents of the membrane bilayers that make up cells. They are believed to be synthesized 'on-demand' rather than made and stored for later use. The mechanisms and enzymes underlying the biosynthesis of endocannabinoids remain elusive and continue to be an area of active research.
The endocannabinoid 2-AG has been found in bovine and human maternal milk.[27]
Retrograde signal
Conventional neurotransmitters are released from a ‘presynaptic’ cell and activate appropriate receptors on a ‘postsynaptic’ cell, where presynaptic and postsynaptic designate the sending and receiving sides of a synapse, respectively. Endocannabinoids, on the other hand, are described as retrograde transmitters because they most commonly travel ‘backwards’ against the usual synaptic transmitter flow. They are, in effect, released from the postsynaptic cell and act on the presynaptic cell, where the target receptors are densely concentrated on axonal terminals in the zones from which conventional neurotransmitters are released. Activation of cannabinoid receptors temporarily reduces the amount of conventional neurotransmitter released. This endocannabinoid mediated system permits the postsynaptic cell to control its own incoming synaptic traffic. The ultimate effect on the endocannabinoid-releasing cell depends on the nature of the conventional transmitter being controlled. For instance, when the release of the inhibitory transmitter GABA is reduced, the net effect is an increase in the excitability of the endocannabinoid-releasing cell. On the converse, when release of the excitatory neurotransmitter glutamate is reduced, the net effect is a decrease in the excitability of the endocannabinoid-releasing cell.
Range
Endocannabinoids are hydrophobic molecules. They cannot travel unaided for long distances in the aqueous medium surrounding the cells from which they are released, and therefore act locally on nearby target cells. Hence, although emanating diffusely from their source cells, they have much more restricted spheres of influence than do hormones, which can affect cells throughout the body.
Other thoughts
Endocannabinoids constitute a versatile system for affecting neuronal network properties in the nervous system.
Scientific American published an article in December 2004, entitled "The Brain's Own Marijuana" discussing the endogenous cannabinoid system. [28]
The current understanding recognizes the role that endocannabinoids play in almost every major life function in the human body.
U.S. Patent # 6630507
In 2003 The U.S.A.'s Government as represented by the Department of Health and Human Services was awarded a patent on cannabinoids as antioxidants and neuroprotectants. U.S. Patent 6630507.
Synthetic and patented cannabinoids
Historically, laboratory synthesis of cannabinoids were often based on the structure of herbal cannabinoids, and a large number of analogs have been produced and tested, especially in a group led by Roger Adams as early as 1941 and later in a group led by Raphael Mechoulam. Newer compounds are no longer related to natural cannabinoids or are based on the structure of the endogenous cannabinoids.
Synthetic cannabinoids are particularly useful in experiments to determine the relationship between the structure and activity of cannabinoid compounds, by making systematic, incremental modifications of cannabinoid molecules.
Medications containing natural or synthetic cannabinoids or cannabinoid analogs:
- Dronabinol (Marinol), is Δ9-tetrahydrocannabinol (THC), used as an appetite stimulant, anti-emetic, and analgesic
- Nabilone (Cesamet), a synthetic cannabinoid and an analog of Marinol. It is Schedule II unlike Marinol, which is Schedule III
- Sativex, a cannabinoid extract oral spray containing THC, CBD, and other cannabinoids used for neuropathic pain and spasticity in 22 countries including England, Canada and Spain. Sativex develops whole-plant cannabinoid medicines
- Rimonabant (SR141716), a selective cannabinoid (CB1) receptor antagonist used as an anti-obesity drug under the proprietary name Acomplia. It is also used for smoking cessation
Other notable synthetic cannabinoids include:
- CP-55940, produced in 1974, this synthetic cannabinoid receptor agonist is many times more potent than THC
- Dimethylheptylpyran
- HU-210, about 100 times as potent as THC[29]
- HU-331 a potential anti-cancer drug derived from cannabidiol that specifically inhibits topoisomerase II.
- SR144528, a CB2 receptor antagonists
- WIN 55,212-2, a potent cannabinoid receptor agonist
- JWH-133, a potent selective CB2 receptor agonist
- Levonantradol (Nantrodolum), an anti-emetic and analgesic but not currently in use in medicine
Table of natural cannabinoids
| Cannabigerol-type (CBG) | ||||
|---|---|---|---|---|
Cannabigerol |
Cannabigerol |
Cannabinerolic acid A |
Cannabigerovarin |
|
Cannabigerolic acid A |
Cannabigerolic acid A |
Cannabigerovarinic acid A |
||
| Cannabichromene-type (CBC) | ||||

(±)-Cannabichromene |
(±)-Cannabichromenic acid A |
(±)-Cannabivarichromene, |
(±)-Cannabichromevarinic |
|
| Cannabidiol-type (CBD) | ||||
(−)-Cannabidiol |
Cannabidiol |
Cannabidiol-C4 |
(−)-Cannabidivarin |

Cannabidiorcol |
Cannabidiolic acid |
Cannabidivarinic acid |
|||
| Cannabinodiol-type (CBND) | ||||
Cannabinodiol |
Cannabinodivarin |
|||
| Tetrahydrocannabinol-type (THC) | ||||

Δ9-Tetrahydrocannabinol |
Δ9-Tetrahydrocannabinol-C4 |
Δ9-Tetrahydrocannabivarin |

Δ9-Tetrahydrocannabiorcol |
|
Δ9-Tetrahydro- |
Δ9-Tetrahydro- |
Δ9-Tetrahydro- |
Δ9-Tetrahydro- |
Δ9-Tetrahydro- |

(−)-Δ8-trans-(6aR,10aR)- |
(−)-Δ8-trans-(6aR,10aR)- |
(−)-(6aS,10aR)-Δ9- |
||
| Cannabinol-type (CBN) | ||||
Cannabinol |
Cannabinol-C4 |

Cannabivarin |

Cannabinol-C2 |

Cannabiorcol |
Cannabinolic acid A |
Cannabinol methyl ether |
|||
| Cannabitriol-type (CBT) | ||||
-trans-cannabitriol.png)
(−)-(9R,10R)-trans- |
-trans-cannabitriol.png)
(+)-(9S,10S)-Cannabitriol |
(±)-(9R,10S/9S,10R)- |
(−)-(9R,10R)-trans- |
(±)-(9R,10R/9S,10S)- |
-tetrahydrocannabinol.png)
8,9-Dihydroxy-Δ6a(10a)- |
Cannabidiolic acid A |
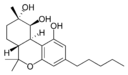
(−)-(6aR,9S,10S,10aR)- |
(−)-6a,7,10a-Trihydroxy- |
-tetrahydrocannabinol.png)
10-Oxo-Δ6a(10a)- |
| Cannabielsoin-type (CBE) | ||||
(5aS,6S,9R,9aR)- |

(5aS,6S,9R,9aR)- |

(5aS,6S,9R,9aR)- |
(5aS,6S,9R,9aR)- |

(5aS,6S,9R,9aR)- |

Cannabiglendol-C3 |
Dehydrocannabifuran |
Cannabifuran |
||
| Isocannabinoids | ||||
(−)-Δ7-trans-(1R,3R,6R)- |
(±)-Δ7-1,2-cis- |
(−)-Δ7-trans-(1R,3R,6R)- |
||
| Cannabicyclol-type (CBL) | ||||
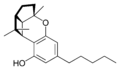
(±)-(1aS,3aR,8bR,8cR)- |
(±)-(1aS,3aR,8bR,8cR)- |

(±)-(1aS,3aR,8bR,8cR)- |
||
| Cannabicitran-type (CBT) | ||||
Cannabicitran |
||||
| Cannabichromanone-type (CBCN) | ||||
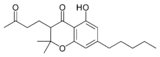
Cannabichromanone |
Cannabichromanone-C3 |
Cannabicoumaronone |
||
See also
- Cannabinoid receptor antagonist
References
- ↑ Lambert DM, Fowler CJ (2005). "The endocannabinoid system: drug targets, lead compounds, and potential therapeutic applications". J. Med. Chem. 48 (16): 5059–87. doi:10.1021/jm058183t. PMID 16078824.
- ↑ Begg M, Pacher P, Bátkai S, Osei-Hyiaman D, Offertáler L, Mo FM, Liu J, Kunos G (2005). "Evidence for novel cannabinoid receptors". Pharmacol. Ther. 106 (2): 133–45. doi:10.1016/j.pharmthera.2004.11.005. PMID 15866316.
- ↑ Núñez E, Benito C, Pazos MR, et al. (2004). "Cannabinoid CB2 receptors are expressed by perivascular microglial cells in the human brain: an immunohistochemical study". Synapse 53 (4): 208–13. doi:10.1002/syn.20050. PMID 15266552.
- ↑ Burns TL, Ineck JR. "Cannabinoid analgesia as a potential new therapeutic option in the treatment of chronic pain." The Annals of Pharmacotherapy. 2006 Feb;40(2):251-60. PMID 16449552
- ↑ Downer EJ, Campbell, VA. "Phytocannabinoids, CNS cells and development: A dead issue?" Drug and Alcohol Review. 2010 Jan;29(1):91-98. PMID 20078688
- ↑ Huffman JW (2000). "The search for selective ligands for the CB2 receptor". Curr. Pharm. Des. 6 (13): 1323–37. doi:10.2174/1381612003399347. PMID 10903395.
- ↑ 7.0 7.1 "Behavioural Pharmacology - Abstract: Volume 16(5-6) September 2005 p 487-496 Neurophysiological and subjective profile of marijuana with varying concentrations of cannabinoids.". http://www.behaviouralpharm.com/pt/re/bpharm/abstract.00008877-200509000-00023.htm. Retrieved 2007-06-24.
- ↑ Morgan CJ, Curran HV (April 2008). "Effects of cannabidiol on schizophrenia-like symptoms in people who use cannabis". The British journal of psychiatry : the journal of mental science 192 (4): 306–7. doi:10.1192/bjp.bp.107.046649. PMID 18378995.
- ↑ "Should I Smoke Dope?". http://www.bbc.co.uk/programmes/b009nyxf. Retrieved 2008-05-24.
- ↑ 10.0 10.1 Mechoulam R, Peters M, Murillo-Rodriguez E, Hanuš LO (August 2007). "Cannabidiol--recent advances". Chemistry & biodiversity 4 (8): 1678–92. doi:10.1002/cbdv.200790147. PMID 17712814.
- ↑ Mahadevan A, Siegel C, Martin BR, Abood ME, Beletskaya I, Razdan RK (October 2000). "Novel cannabinol probes for CB1 and CB2 cannabinoid receptors". Journal of medicinal chemistry 43 (20): 3778–85. doi:10.1021/jm0001572. PMID 11020293.
- ↑ 12.0 12.1 Cascio MG, Gauson LA, Stevenson LA, Ross RA, Pertwee R (December 2009). "Evidence that the plant cannabinoid cannabigerol is a highly potent alpha(2)-adrenoceptor agonist and moderately potent 5HT receptor antagonist". British Journal of Pharmacology 159 (1): 129–41. doi:10.1111/j.1476-5381.2009.00515.x. PMID 20002104.
- ↑ "British Journal of Pharmacology - Abstract of article: Evidence that the plant cannabinoid Δ9-tetrahydrocannabivarin is a cannabinoid CB1 and CB2 receptor antagonist". http://www.nature.com/bjp/journal/v146/n7/abs/0706414a.html. Retrieved 2007-06-24.
- ↑ 14.0 14.1 14.2 Grotenhermen F. "Cannabinoids." Current Drug Targets - CNS & Neurological Disorders. 2005 Oct;4(5):507-30. PMID 16266285
- ↑ Martin BR, Mechoulam R, Razdan RK (1999). "Discovery and characterization of endogenous cannabinoids". Life sciences 65 (6-7): 573–95. doi:10.1016/S0024-3205(99)00281-7. PMID 10462059.
- ↑ "N-Acylethanolamines in Seeds. Quantification of Molecular Species and Their Degradation upon Imbibition -- Chapman et al. 120 (4): 1157 -- PLANT PHYSIOLOGY". http://www.plantphysiol.org/cgi/content/abstract/120/4/1157. Retrieved 2007-06-24.
- ↑ "ScienceDirect - Biochimica et Biophysica Acta (BBA) - Lipids and Lipid Metabolism : Bioactive long chain N-acylethanolamines in five species of edible bivalve molluscs: Possible implications for mollusc physiology and sea food industry". doi:10.1016/S0005-2760(97)00132-X. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T1X-3SXDXJ8-C&_user=10&_rdoc=1&_fmt=&_orig=search&_sort=d&view=c&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=2bb2860f5331075a2ed6b97b17cbdb47. Retrieved 2007-06-24.
- ↑ Stella N, Schweitzer P, Piomelli D. "A second endogenous cannabinoid that modulates long-term potentiation." Nature. 1997 Aug 21; 388(6644):773-8. PMID 9285589
- ↑ reviewed in Pacher P, Batkai S, Kunos G. "The endocannabinoid system as an emerging target of pharmacotherapy." Pharmacological Reviews. 2006 Sep;58(3):389-462. PMID 16968947
- ↑ Savinainen JR, Jarvinen T, Laine K, Laitinen JT. "Despite substantial degradation, 2-arachidonoylglycerol is a potent full efficacy agonist mediating CB(1) receptor-dependent G-protein activation in rat cerebellar membranes." British Journal of Pharmacology. 2001 Oct; 134(3):664-72. PMID 11588122
- ↑ Hanuš L, Abu-Lafi S, Fride E, et al. (2001). "2-arachidonyl glyceryl ether, an endogenous agonist of the cannabinoid CB1 receptor". Proc. Natl. Acad. Sci. U.S.A. 98 (7): 3662–5. doi:10.1073/pnas.061029898. PMID 11259648.
- ↑ Oka S, Tsuchie A, Tokumura A, Muramatsu M, Suhara Y, Takayama H, Waku K, Sugiura T. "Ether-linked analogue of 2-arachidonoylglycerol (noladin ether) was not detected in the brains of various mammalian species." Journal of Neurochemistry. 2003 Jun;85(6):1374-81. PMID 12787057
- ↑ Bisogno, T., D. Melck, M. Bobrov, N. M. Gretskaya, V. V. Bezuglov, L. De Petrocellis, V. Di Marzo. "N-acyl-dopamines: novel synthetic CB1 cannabinoid-receptor ligands and inhibitors of anandamide inactivation with cannabimimetic activity in vitro and in vivo." The Biochemical Journal. 2000 Nov 1;351 Pt 3:817-24. PMID 11042139
- ↑ Bisogno T, Ligresti A, Di Marzo V. "The endocannabinoid signalling system: biochemical aspects." Pharmacology, Biochemistry, and Behavior. 2005 Jun;81(2):224-38. PMID 15935454
- ↑ Ralevic V. (July 2003). "Cannabinoid modulation of peripheral autonomic and sensory neurotransmission.". European journal of pharmacology 472 (1-2): 1–21. doi:10.1016/S0014-2999(03)01813-2. PMID 12860468.
- ↑ Porter AC, Sauer JM, Knierman MD, Becker GW, Berna MJ, Bao J, Nomikos GG, Carter P, Bymaster FP, Leese AB, Felder CC. (June 2002). "Characterization of a Novel Endocannabinoid, Virodhamine, with Antagonist Activity at the CB1 Receptor". The Journal of pharmacology and experimental therapeutics 301 (3): 1020–1024. doi:10.1124/jpet.301.3.1020. PMID 12023533. http://jpet.aspetjournals.org/cgi/reprint/301/3/1020.pdf.
- ↑ Fride E, Bregman T, Kirkham TC. (April 2005). "Endocannabinoids and food intake: newborn suckling and appetite regulation in adulthood.". Experimental Biology and Medicine 230 (4): 225–234. doi:10.1371/journal.pbio.0020286. PMID 15792943. http://www.ebmonline.org/cgi/reprint/230/4/225.pdf.
- ↑ Nicoll RA, Alger BE (2004). "The brain's own marijuana". Sci. Am. 291 (6): 68–75. doi:10.1038/scientificamerican1204-68. PMID 15597982.
- ↑ http://www.marijuana.org/mydna10-12-05.htm
Further reading
- PMID 12586720 (PubMed)
Citation will be completed automatically in a few minutes.
Jump the queue or expand by hand
- Devane WA, Hanuš L, Breuer A, et al. (1992). "Isolation and structure of a brain constituent that binds to the cannabinoid receptor". Science 258 (5090): 1946–9. doi:10.1126/science.1470919. PMID 1470919.
- Elsohly MA, Slade D (2005). "Chemical constituents of marijuana: the complex mixture of natural cannabinoids". Life Sci. 78 (5): 539–48. doi:10.1016/j.lfs.2005.09.011. PMID 16199061.
- Hanuš L, Gopher A, Almog S, Mechoulam R (1993). "Two new unsaturated fatty acid ethanolamides in brain that bind to the cannabinoid receptor". J. Med. Chem. 36 (20): 3032–4. doi:10.1021/jm00072a026. PMID 8411021.
- Hanuš L (1987). "Biogenesis of cannabinoid substances in the plant". Acta Universitatis Palackianae Olomucensis Facultatis Medicae 116: 47–53. PMID 2962461.
- Hanuš L., Krejčí Z. (1975) "Isolation of two new cannabinoid acids from Cannabis sativa L. of Czechoslovak origin". Acta Univ. Olomuc., Fac. Med. 74: 161-166.
- Hanuš L., Krejčí Z., Hruban L. (1975) "Isolation of cannabidiolic acid from Turkish variety of cannabis cultivated for fibre". Acta Univ. Olomuc., Fac. Med. 74: 167-172.
- doi:10.1007/978-0-387-74349-3
This citation will be automatically completed in the next few minutes. You can jump the queue or expand by hand
- Mechoulam R, Ben-Shabat S, Hanuš L, et al. (1995). "Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors". Biochem. Pharmacol. 50 (1): 83–90. doi:10.1016/0006-2952(95)00109-D. PMID 7605349.
- PMID 19005078 (PubMed)
Citation will be completed automatically in a few minutes.
Jump the queue or expand by hand
- PMID 19005077 (PubMed)
Citation will be completed automatically in a few minutes.
Jump the queue or expand by hand
- Turner C. E., Mole M. L., Hanuš L., ElSohly H. N. (1981) "Constituents of Cannabis sativa L. XIX. Isolation and structure elucidation of cannabiglendol. A novel cannabinoid from an Indian variant." J. Nat. Prod. 44 (1): 27-33.
External links
- Bela Szabo: Pharmacology of Cannabinoid Receptors, BIOTREND Reviews No. 02, February 2008
- The International Cannabinoid Research Society
- The Canadian Consortium for the Investigation of Cannabinoids
- Cannabinoids: A Secret History by Tom Geller, Chemical Heritage Newsmagazine, 25 (2), Summer 2007
- Marijuana and Medicine - Assessing the Science Base (Institute of Medicine) - 1999 at National Academies Press
- House of Lords Report - Cannabis (United Kingdom) - 1998 at Parliament of the United Kingdom
- Cannabis: A Health Perspective and Research Agenda - 1997 at World Health Organization
- Chemical Ecology of Cannabis (J. Intl. Hemp Assn. - 1994)
- Therapeutic Potential in Spotlight at Cannabinoid Researchers' Meeting at California Cannabis Research Medical Group
- THC (tetrahydrocannabinol) accumulation in glands of Cannabis (Cannabaceae)
|
|||||||||||||||||||||||||||||||||||||||||||||||||