Electroencephalography


Electroencephalography (EEG) is the recording of electrical activity along the scalp produced by the firing of neurons within the brain.[2] In clinical contexts, EEG refers to the recording of the brain's spontaneous electrical activity over a short period of time, usually 20–40 minutes, as recorded from multiple electrodes placed on the scalp. In neurology, the main diagnostic application of EEG is in the case of epilepsy, as epileptic activity can create clear abnormalities on a standard EEG study.[3] A secondary clinical use of EEG is in the diagnosis of coma, encephalopathies, and brain death. EEG used to be a first-line method for the diagnosis of tumors, stroke and other focal brain disorders, but this use has decreased with the advent of anatomical imaging techniques such as MRI and CT.
Derivatives of the EEG technique include evoked potentials (EP), which involves averaging the EEG activity time-locked to the presentation of a stimulus of some sort (visual, somatosensory, or auditory). Event-related potentials refer to averaged EEG responses that are time-locked to more complex processing of stimuli; this technique is used in cognitive science, cognitive psychology, and psychophysiological research.
Contents |
Source of EEG activity
The electrical activity of the brain can be described in spatial scales from the currents within a single dendritic spine to the relatively gross potentials that the EEG records from the scalp, much the same way that economics can be studied from the level of a single individual's personal finances to the macro-economics of nations. Neurons, or nerve cells, are electrically active cells that are primarily responsible for carrying out the brain's functions. Neurons create action potentials, which are discrete electrical signals that travel down axons and cause the release of chemical neurotransmitters at the synapse, which is an area of near contact between two neurons. This neurotransmitter then activates a receptor in the dendrite or body of the neuron that is on the other side of the synapse, the post-synaptic neuron. The neurotransmitter, when combined with the receptor, typically causes an electrical current within the dendrite or body of the post-synaptic neuron. Thousands of post-synaptic currents from a single neuron's dendrites and body then sum up to cause the neuron to generate an action potential. This neuron then synapses on other neurons, and so on.
EEG reflects correlated synaptic activity caused by post-synaptic potentials of cortical neurons. The ionic currents involved in the generation of fast action potentials may not contribute greatly to the averaged field potentials representing the EEG .[4][5] More specifically, the scalp electrical potentials that produce EEG are generally thought to be caused by the extracellular ionic currents caused by dendritic electrical activity, whereas the fields producing magnetoencephalographic signals[6] are associated with intracellular ionic currents .[7]
The electric potentials generated by single neurons are far too small to be picked by EEG or MEG.[5] EEG activity therefore always reflects the summation of the synchronous activity of thousands or millions of neurons that have similar spatial orientation. Because voltage fields fall off with the square of the distance, activity from deep sources is more difficult to detect than currents near the skull.[8]
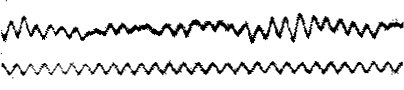
Scalp EEG activity shows oscillations at a variety of frequencies. Several of these oscillations have characteristic frequency ranges, spatial distributions and are associated with different states of brain functioning (e.g., waking and the various sleep stages). These oscillations represent synchronized activity over a network of neurons. The neuronal networks underlying some of these oscillations are understood (e.g., the thalamocortical resonance underlying sleep spindles), while many others are not (e.g., the system that generates the posterior basic rhythm). Research that measures both EEG and neuron spiking finds the relationship between the two is complex with the power of surface EEG only in two bands that of gamma and delta relating to neuron spike activity.[9]
Clinical use
A routine clinical EEG recording typically lasts 20–30 minutes (plus preparation time) and usually involves recording from scalp electrodes. Routine EEG is typically used in the following clinical circumstances:
- to distinguish epileptic seizures from other types of spells, such as psychogenic non-epileptic seizures, syncope (fainting), sub-cortical movement disorders and migraine variants.
- to differentiate "organic" encephalopathy or delirium from primary psychiatric syndromes such as catatonia
- to serve as an adjunct test of brain death
- to prognosticate, in certain instances, in patients with coma
- to determine whether to wean anti-epileptic medications
At times, a routine EEG is not sufficient, particularly when it is necessary to record a patient while he/she is having a seizure. In this case, the patient may be admitted to the hospital for days or even weeks, while EEG is constantly being recorded (along with time-synchronized video and audio recording). A recording of an actual seizure (i.e., an ictal recording, rather than an inter-ictal recording of a possibly epileptic patient at some period between seizures) can give significantly better information about whether or not a spell is an epileptic seizure and the focus in the brain from which the seizure activity emanates.
Epilepsy monitoring is typically done:
- to distinguish epileptic seizures from other types of spells, such as psychogenic non-epileptic seizures, syncope (fainting), sub-cortical movement disorders and migraine variants.
- to characterize seizures for the purposes of treatment
- to localize the region of brain from which a seizure originates for work-up of possible seizure surgery
Additionally, EEG may be used to monitor certain procedures:
- to monitor the depth of anesthesia
- as an indirect indicator of cerebral perfusion in carotid endarterectomy
- to monitor amobarbital effect during the Wada test
EEG can also be used in intensive care units for brain function monitoring:
- to monitor for non-convulsive seizures/non-convulsive status epilepticus
- to monitor the effect of sedative/anesthesia in patients in medically induced coma (for treatment of refractory seizures or increased intracranial pressure)
- to monitor for secondary brain damage in conditions such as subarachnoid hemorrhage (currently a research method)
If a patient with epilepsy is being considered for resective surgery, it is often necessary to localize the focus (source) of the epileptic brain activity with a resolution greater than what is provided by scalp EEG. This is because the cerebrospinal fluid, skull and scalp smear the electrical potentials recorded by scalp EEG. In these cases, neurosurgeons typically implant strips and grids of electrodes (or penetrating depth electrodes) under the dura mater, through either a craniotomy or a burr hole. The recording of these signals is referred to as electrocorticography (ECoG), subdural EEG (sdEEG) or intracranial EEG (icEEG)--all terms for the same thing. The signal recorded from ECoG is on a different scale of activity than the brain activity recorded from scalp EEG. Low voltage, high frequency components that cannot be seen easily (or at all) in scalp EEG can be seen clearly in ECoG. Further, smaller electrodes (which cover a smaller parcel of brain surface) allow even lower voltage, faster components of brain activity to be seen. Some clinical sites record from penetrating microelectrodes.[2]
Research use
EEG, and its derivative, ERPs, are used extensively in neuroscience, cognitive science, cognitive psychology, and psychophysiological research. Many techniques used in research contexts are not standardized sufficiently to be used in the clinical context.
A different method to study brain function is functional magnetic resonance imaging (fMRI). Some benefits of EEG compared to fMRI include:
- Hardware costs are significantly lower for EEG sensors versus an fMRI machine
- EEG sensors can be deployed into a wider variety of environments than can a bulky, immobile fMRI machine
- EEG enables higher temporal resolution, on the order of milliseconds, rather than seconds
- EEG is relatively tolerant of subject movement versus an fMRI (where the subject must remain completely still)
- EEG is silent, which allows for better study of the responses to auditory stimuli
- EEG does not aggravate claustrophobia
Limitations of EEG as compared with fMRI include:
- Significantly lower spatial resolution
- ERP studies require relatively simple paradigms, compared with block-design fMRI studies
EEG recordings have been successfully obtained simultaneously with fMRI scans, though successful simultaneous recording requires that several technical issues be overcome, such as the presence of ballistocardiographic artifact, MRI pulse artifact and the induction of electrical currents in EEG wires that move within the strong magnetic fields of the MRI.
EEG also has some characteristics that compare favorably with behavioral testing:
- EEG can detect covert processing (i.e., processing that does not require a response)
- EEG can be used in subjects who are incapable of making a motor response
- Some ERP components can be detected even when the subject is not attending to the stimuli
- As compared with other reaction time paradigms, ERPs can elucidate stages of processing (rather than just the final end result)
Method
.jpg)
In conventional scalp EEG, the recording is obtained by placing electrodes on the scalp with a conductive gel or paste, usually after preparing the scalp area by light abrasion to reduce impedance due to dead skin cells. Many systems typically use electrodes, each of which is attached to an individual wire. Some systems use caps or nets into which electrodes are embedded; this is particularly common when high-density arrays of electrodes are needed.
Electrode locations and names are specified by the International 10–20 system[10] for most clinical and research applications (except when high-density arrays are used). This system ensures that the naming of electrodes is consistent across laboratories. In most clinical applications, 19 recording electrodes (plus ground and system reference) are used. A smaller number of electrodes are typically used when recording EEG from neonates. Additional electrodes can be added to the standard set-up when a clinical or research application demands increased spatial resolution for a particular area of the brain. High-density arrays (typically via cap or net) can contain up to 256 electrodes more-or-less evenly spaced around the scalp.
Each electrode is connected to one input of a differential amplifier (one amplifier per pair of electrodes); a common system reference electrode is connected to the other input of each differential amplifier. These amplifiers amplify the voltage between the active electrode and the reference (typically 1,000–100,000 times, or 60–100 dB of voltage gain). In analog EEG, the signal is then filtered (next paragraph), and the EEG signal is output as the deflection of pens as paper passes underneath. Most EEG systems these days, however, are digital, and the amplified signal is digitized via an analog-to-digital converter, after being passed through an anti-aliasing filter. Analog-to-digital sampling typically occurs at 256–512 Hz in clinical scalp EEG; sampling rates of up to 20 kHz are used in some research applications.
During the recording, a series of activation procedures may be used. These procedures may induce normal or abnormal EEG activity that might not otherwise be seen. These procedures include hyperventilation, photic stimulation (with a strobe light), eye closure, mental activity, sleep and sleep deprivation. During (inpatient) epilepsy monitoring, a patient's typical seizure medications may be withdrawn.
The digital EEG signal is stored electronically and can be filtered for display. Typical settings for the high-pass filter and a low-pass filter are 0.5-1 Hz and 35–70 Hz, respectively. The high-pass filter typically filters out slow artifact, such as electrogalvanic signals and movement artifact, whereas the low-pass filter filters out high-frequency artifacts, such as electromyographic signals. An additional notch filter is typically used to remove artifact caused by electrical power lines (60 Hz in the United States and 50 Hz in many other countries).[2] As part of an evaluation for epilepsy surgery, it may be necessary to insert electrodes near the surface of the brain, under the surface of the dura mater. This is accomplished via burr hole or craniotomy. This is referred to variously as "electrocorticography (ECoG)", "intracranial EEG (I-EEG)" or "subdural EEG (SD-EEG)". Depth electrodes may also be placed into brain structures, such as the amygdala or hippocampus, structures, which are common epileptic foci and may not be "seen" clearly by scalp EEG. The electrocorticographic signal is processed in the same manner as digital scalp EEG (above), with a couple of caveats. ECoG is typically recorded at higher sampling rates than scalp EEG because of the requirements of Nyquist theorem—the subdural signal is composed of a higher predominance of higher frequency components. Also, many of the artifacts that affect scalp EEG do not impact ECoG, and therefore display filtering is often not needed.
A typical adult human EEG signal is about 10µV to 100 µV in amplitude when measured from the scalp [11] and is about 10–20 mV when measured from subdural electrodes.
Since an EEG voltage signal represents a difference between the voltages at two electrodes, the display of the EEG for the reading encephalographer may be set up in one of several ways. The representation of the EEG channels is referred to as a montage.
- Bipolar montage
- Each channel (i.e., waveform) represents the difference between two adjacent electrodes. The entire montage consists of a series of these channels. For example, the channel "Fp1-F3" represents the difference in voltage between the Fp1 electrode and the F3 electrode. The next channel in the montage, "F3-C3," represents the voltage difference between F3 and C3, and so on through the entire array of electrodes.
- Referential montage
- Each channel represents the difference between a certain electrode and a designated reference electrode. There is no standard position for this reference; it is, however, at a different position than the "recording" electrodes. Midline positions are often used because they do not amplify the signal in one hemisphere vs. the other. Another popular reference is "linked ears," which is a physical or mathematical average of electrodes attached to both earlobes or mastoids.
- Average reference montage
- The outputs of all of the amplifiers are summed and averaged, and this averaged signal is used as the common reference for each channel.
- Laplacian montage
- Each channel represents the difference between an electrode and a weighted average of the surrounding electrodes.[12]
When analog (paper) EEGs are used, the technologist switches between montages during the recording in order to highlight or better characterize certain features of the EEG. With digital EEG, all signals are typically digitized and stored in a particular (usually referential) montage; since any montage can be constructed mathematically from any other, the EEG can be viewed by the electroencephalographer in any display montage that is desired.
The EEG is read by a neurologist, optimally one who has specific training in the interpretation of EEGs. This is done by visual inspection of the waveforms, called graphoelements. The use of computer signal processing of the EEG—so-called quantitative EEG—is somewhat controversial when used for clinical purposes (although there are many research uses).
Limitations
EEG has several limitations. Most important is its poor spatial resolution. EEG is most sensitive to a particular set of post-synaptic potentials: those generated in superficial layers of the cortex, on the crests of gyri directly abutting the skull and radial to the skull. Dendrites, which are deeper in the cortex, inside sulci, in midline or deep structures (such as the cingulate gyrus or hippocampus), or producing currents that are tangential to the skull, have far less contribution to the EEG signal.
The meninges, cerebrospinal fluid and skull "smear" the EEG signal, obscuring its intracranial source.
It is mathematically impossible to reconstruct a unique intracranial current source for a given EEG signal,[2] as some currents produce potentials that cancel each other out. This is referred to as the inverse problem. However, much work has been done to produce remarkably good estimates of, at least, a localized electric dipole that represents the recorded currents.
EEG vs fMRI and PET
EEG has several strong points as a tool for exploring brain activity. EEG's can detect changes within a millisecond timeframe, excellent considering an action potential takes approximately 0.5-130 milliseconds to propagate across a single neuron, depending on the type of neuron.[13] Other methods of looking at brain activity, such as PET and fMRI have time resolution between seconds and minutes. EEG measures the brain's electrical activity directly, while other methods record changes in blood flow (e.g., SPECT, fMRI) or metabolic activity (e.g., PET), which are indirect markers of brain electrical activity. EEG can be used simultaneously with fMRI so that high-temporal-resolution data can be recorded at the same time as high-spatial-resolution data, however, since the data derived from each occurs over a different time course, the data sets do not necessarily represent the exact same brain activity. There are technical difficulties associated with combining these two modalities, including the need to remove the MRI gradient artifact present during MRI acquisition and the ballistocardiographic artifact (resulting from the pulsatile motion of blood and tissue) from the EEG. Furthermore, currents can be induced in moving EEG electrode wires due to the magnetic field of the MRI.
EEG can be recorded at the same time as MEG so that data from these complementary high-time-resolution techniques can be combined.
Normal activity

The EEG is typically described in terms of (1) rhythmic activity and (2) transients. The rhythmic activity is divided into bands by frequency. To some degree, these frequency bands are a matter of nomenclature (i.e., any rhythmic activity between 8–12 Hz can be described as "alpha"), but these designations arose because rhythmic activity within a certain frequency range was noted to have a certain distribution over the scalp or a certain biological significance. Frequency bands are usually extracted using spectral methods (for instance Welch) as implemented for instance in freely available EEG software such as EEGLAB.
Most of the cerebral signal observed in the scalp EEG falls in the range of 1–20 Hz (activity below or above this range is likely to be artifactual, under standard clinical recording techniques).
Comparison table
| Type | Frequency (Hz) | Location | Normally | Pathologically |
|---|---|---|---|---|
| Delta | up to 4 | frontally in adults, posteriorly in children; high amplitude waves |
|
|
| Theta | 4 – 7 Hz | Found in locations not related to task at hand |
|
|
| Alpha | 8 – 12 Hz | posterior regions of head, both sides, higher in amplitude on dominant side. Central sites (c3-c4) at rest . |
|
|
| Beta | 12 – 30 Hz | both sides, symmetrical distribution, most evident frontally; low amplitude waves |
|
|
| Gamma | 30 – 100 + | Somatosensory cortex |
|
|
It should be noted that while these are the universally recognized ranges, they are not concrete definitions of the range of brain-waves. While researchers tend to follow these guidelines, many scholars use their own specific boundaries depending on the range they choose to focus on. Additionally, some researchers define the bands using decimal values rather than rounding to whole numbers (for example, one researcher may define the lower Beta band cut-off as 12.1, while another may use the value 13), while still others sometimes divide the bands into sub-bands. Generally, this is only done for the sake of analysis.
Wave patterns

- Delta is the frequency range up to 4 Hz. It tends to be the highest in amplitude and the slowest waves. It is seen normally in adults in slow wave sleep. It is also seen normally in babies. It may occur focally with subcortical lesions and in general distribution with diffuse lesions, metabolic encephalopathy hydrocephalus or deep midline lesions. It is usually most prominent frontally in adults (e.g. FIRDA - Frontal Intermittent Rhythmic Delta) and posteriorly in children (e.g. OIRDA - Occipital Intermittent Rhythmic Delta).

- Theta is the frequency range from 4 Hz to 7 Hz. Theta is seen normally in young children. It may be seen in drowsiness or arousal in older children and adults; it can also be seen in meditation.[14] Excess theta for age represents abnormal activity. It can be seen as a focal disturbance in focal subcortical lesions; it can be seen in generalized distribution in diffuse disorder or metabolic encephalopathy or deep midline disorders or some instances of hydrocephalus. On the contrary this range has been associated with reports of relaxed, meditative, and creative states.

- Alpha is the frequency range from 8 Hz to 12 Hz. Hans Berger named the first rhythmic EEG activity he saw, the "alpha wave." This is activity in the 8–12 Hz range seen in the posterior regions of the head on both sides, being higher in amplitude on the dominant side. It is brought out by closing the eyes and by relaxation. It was noted to attenuate with eye opening or mental exertion. This activity is now referred to as "posterior basic rhythm," the "posterior dominant rhythm" or the "posterior alpha rhythm." The posterior basic rhythm is actually slower than 8 Hz in young children (therefore technically in the theta range). In addition to the posterior basic rhythm, there are two other normal alpha rhythms that are typically discussed: the mu rhythm and a temporal "third rhythm". Alpha can be abnormal; for example, an EEG that has diffuse alpha occurring in coma and is not responsive to external stimuli is referred to as "alpha coma".

- Mu rhythm is alpha-range activity that is seen over the sensorimotor cortex. It characteristically attenuates with movement of the contralateral arm (or mental imagery of movement of the contralateral arm).

- Beta is the frequency range from 12 Hz to about 30 Hz. It is seen usually on both sides in symmetrical distribution and is most evident frontally. Beta activity is closely linked to motor behavior and is generally attenuated during active movements.[15] Low amplitude beta with multiple and varying frequencies is often associated with active, busy or anxious thinking and active concentration. Rhythmic beta with a dominant set of frequencies is associated with various pathologies and drug effects, especially benzodiazepines. It may be absent or reduced in areas of cortical damage. It is the dominant rhythm in patients who are alert or anxious or who have their eyes open.

- Gamma is the frequency range approximately 30–100 Hz. Gamma rhythms are thought to represent binding of different populations of neurons together into a network for the purpose of carrying out a certain cognitive or motor function.
"Ultra-slow" or "near-DC" activity is recorded using DC amplifiers in some research contexts. It is not typically recorded in a clinical context because the signal at these frequencies is susceptible to a number of artifacts.
Some features of the EEG are transient rather than rhythmic. Spikes and sharp waves may represent seizure activity or interictal activity in individuals with epilepsy or a predisposition toward epilepsy. Other transient features are normal: vertex waves and sleep spindles are seen in normal sleep.
Note that there are types of activity that are statistically uncommon, but not associated with dysfunction or disease. These are often referred to as "normal variants." The mu rhythm is an example of a normal variant.
The normal Electroencephalography (EEG) varies by age. The neonatal EEG is quite different from the adult EEG. The EEG in childhood generally has slower frequency oscillations than the adult EEG.
The normal EEG also varies depending on state. The EEG is used along with other measurements (EOG, EMG) to define sleep stages in polysomnography. Stage I sleep (equivalent to drowsiness in some systems) appears on the EEG as drop-out of the posterior basic rhythm. There can be an increase in theta frequencies. Santamaria and Chiappa cataloged a number of the variety of patterns associated with drowsiness. Stage II sleep is characterized by sleep spindles—transient runs of rhythmic activity in the 12–14 Hz range (sometimes referred to as the "sigma" band) that have a frontal-central maximum. Most of the activity in Stage II is in the 3–6 Hz range. Stage III and IV sleep are defined by the presence of delta frequencies and are often referred to collectively as "slow-wave sleep." Stages I-IV comprise non-REM (or "NREM") sleep. The EEG in REM (rapid eye movement) sleep appears somewhat similar to the awake EEG.
EEG under general anesthesia depends on the type of anesthetic employed. With halogenated anesthetics, such as halothane or intravenous agents, such as propofol, a rapid (alpha or low beta), nonreactive EEG pattern is seen over most of the scalp, especially anteriorly; in some older terminology this was known as a WAR (widespread anterior rapid) pattern, contrasted with a WAIS (widespread slow) pattern associated with high doses of opiates. Anesthetic effects on EEG signals are beginning to be understood at the level of drug actions on different kinds of synapses and the circuits that allow synchronized neuronal activity (see: http://www.stanford.edu/group/maciverlab/).
Artifacts
Biological artifacts
Electrical signals detected along the scalp by an EEG, but that originate from non-cerebral origin are called artifacts. EEG data is almost always contaminated by such artifacts. The amplitude of artifacts can be quite large relative to the size of amplitude of the cortical signals of interest. This is one of the reasons why it takes considerable experience to correctly interpret EEGs clinically. Some of the most common types of biological artifacts include:
- Eye-induced artifacts (includes eye blinks, eye movements and extra-ocular muscle activity)
- EKG (cardiac) artifacts
- EMG (muscle activation)-induced artifacts
- Glossokinetic artifacts
The most prominent eye-induced artifacts are caused by the potential difference between the cornea and retina, which is quite large compared to cerebral potentials. When the eyes and eyelids are completely still, this corneo-retinal dipole does not affect EEG. However, blinks occur several times per minute, the eyes movements occur several times per second. Eyelid movements, occurring mostly during blinking or vertical eye movements, elicit a large potential seen mostly in the difference between the Electrooculography (EOG) channels above and below the eyes. An established explanation of this potential regards the eyelids as sliding electrodes that short-circuit the positively charged cornea to the extra-ocular skin [16][17]. Rotation of the eyeballs, and consequently of the corneo-retinal dipole, increases the potential in electrodes towards which the eyes are rotated, and decrease the potentials in the opposing electrodes[18]. Eye movements called saccades also generate transient electromyographic potentials, known as saccadic spike potentials (SPs)[19]. The spectrum of these SPs overlaps the gamma-band (see Gamma wave), and seriously confounds analysis of induced gamma-band responses[20], requiring tailored artifact correction approaches[21]. Purposeful or reflexive eye blinking also generates electromyographic potentials, but more importantly there is reflexive movement of the eyeball during blinking that gives a characteristic artifactual appearance of the EEG (see Bell's phenomenon).
Eyelid fluttering artifacts of a characteristic type were previously called Kappa rhythm (or Kappa waves). It is usually seen in the prefrontal leads, that is, just over the eyes. Sometimes they are seen with mental activity. They are usually in the Theta (4–7 Hz) or Alpha (8–13 Hz) range. They were named because they were believed to originate from the brain. Later study revealed they were generated by rapid fluttering of the eyelids, sometimes so minute that it was difficult to see. They are in fact noise in the EEG reading, and should not technically be called a rhythm or wave. Therefore, current usage in electroencephalography refers to the phenomenon as an eyelid fluttering artifact, rather than a Kappa rhythm (or wave).[22]
Some of these artifacts can be useful in various applications. The EOG signals, for instance, can be used to detect[23] and track eye-movements, which are very important in polysomnography, and is also in conventional EEG for assessing possible changes in alertness, drowsiness or sleep.
EKG artifacts are quite common and can be mistaken for spike activity. Because of this, modern EEG acquisition commonly includes a one-channel EKG from the extremities. This also allows the EEG to identify cardiac arrhythmias that are an important differential diagnosis to syncope or other episodic/attack disorders.
Glossokinetic artifacts are caused by the potential difference between the base and the tip of the tongue. Minor tongue movements can contaminate the EEG, especially in parkinsonian and tremor disorders.
Environmental artifacts
In addition to artifacts generated by the body, many artifacts originate from outside the body. Movement by the patient, or even just settling of the electrodes, may cause electrode pops, spikes originating from a momentary change in the impedance of a given electrode. Poor grounding of the EEG electrodes can cause significant 50 or 60 Hz artifact, depending on the local power system's frequency. A third source of possible interference can be the presence of an IV drip; such devices can cause rhythmic, fast, low-voltage bursts, which may be confused for spikes.
Artifact correction
Recently, independent component analysis techniques have been used to correct or remove EEG contaminates[24][25][26][27][28]. These techniques attempt to "unmix" the EEG signals into some number of underlying components. There are many source separation algorithms, often assuming various behaviors or natures of EEG. Regardless, the principle behind any particular method usually allow "remixing" only those components that would result in "clean" EEG by nullifying (zeroing) the weight of unwanted components. Fully automated artifact rejection methods, which use ICA, have also been developed[29].
Abnormal activity
Abnormal activity can broadly be separated into epileptiform and non-epileptiform activity. It can also be separated into focal or diffuse.
Focal epileptiform discharges represent fast, synchronous potentials in a large number of neurons in a somewhat discrete area of the brain. These can occur as interictal activity, between seizures, and represent an area of cortical irritability that may be predisposed to producing epileptic seizures. Interictal discharges are not wholly reliable for determining whether a patient has epilepsy nor where his/her seizure might originate. (See focal epilepsy.)
Generalized epileptiform discharges often have an anterior maximum, but these are seen synchronously throughout the entire brain. They are strongly suggestive of a generalized epilepsy.
Focal non-epileptiform abnormal activity may occur over areas of the brain where there is focal damage of the cortex or white matter. It often consists of an increase in slow frequency rhythms and/or a loss of normal higher frequency rhythms. It may also appear as focal or unilateral decrease in amplitude of the EEG signal.
Diffuse non-epileptiform abnormal activity may manifest as diffuse abnormally slow rhythms or bilateral slowing of normal rhythms, such as the PBR.
More advanced measures of abnormal EEG signals have also recently received attention as possible biomarkers for different disorders such as Alzheimer's disease.[30]
History
A timeline of the history of EEG is given by Swartz.[31] Richard Caton (1842–1926), a physician practicing in Liverpool, presented his findings about electrical phenomena of the exposed cerebral hemispheres of rabbits and monkeys in the British Medical Journal in 1875. In 1890, Polish physiologist Adolf Beck published an investigation of spontaneous electrical activity of the brain of rabbits and dogs that included rhythmic oscillations altered by light.
In 1912, Russian physiologist, Vladimir Vladimirovich Pravdich-Neminsky published the first EEG and the evoked potential of the mammalian (dog).[32] In 1914, Napoleon Cybulski and Jelenska-Macieszyna photographed EEG-recordings of experimentally induced seizures.
German physiologist and psychiatrist Hans Berger (1873–1941) began his studies of the human EEG in 1920. He gave the device its name and is sometimes credited with inventing the EEG, though others had performed similar experiments. His work was later expanded by Edgar Douglas Adrian. In 1934, Fisher and Lowenback first demonstrated epileptiform spikes. In 1935 Gibbs, Davis and Lennox described interictal spike waves and the 3 cycles/s pattern of clinical absence seizures, which began the field of clinical electroencephalography. Subsequently, in 1936 Gibbs and Jasper reported the interictal spike as the focal signature of epilepsy. The same year, the first EEG laboratory opened at Massachusetts General Hospital.
Franklin Offner (1911–1999), professor of biophysics at Northwestern University developed a prototype of the EEG that incorporated a piezoelectric inkwriter called a Crystograph (the whole device was typically known as the Offner Dynograph).
In 1947, The American EEG Society was founded and the first International EEG congress was held. In 1953 Aserinsky and Kleitman describe REM sleep.
In the 1950s, William Grey Walter developed an adjunct to EEG called EEG topography, which allowed for the mapping of electrical activity across the surface of the brain. This enjoyed a brief period of popularity in the 1980s and seemed especially promising for psychiatry. It was never accepted by neurologists and remains primarily a research tool.
Various uses
The EEG has been used for many purposes besides the conventional uses of clinical diagnosis and conventional cognitive neuroscience. Long-term EEG recordings in epilepsy patients are used for seizure prediction. Neurofeedback remains an important extension, and in its most advanced form is also attempted as the basis of brain computer interfaces. The EEG is also used quite extensively in the field of neuromarketing. There are many commercial products substantially based on the EEG.
Honda is attempting to develop a system to move its Asimo robot using EEG, a technology it eventually hopes to incorporate into its automobiles.[33]
EEGs have been used as evidence in trials in the Indian state of Maharastra.[34]
EEG and Telepathy
DARPA has budgeted $4 million in 2009 to investigate technology to enable soldiers on the battlefield to communicate via computer-mediated telepathy. The aim is to analyse neural signals that exist in the brain before words are spoken. [35]
Games
Recently a few companies have scaled back medical grade EEG technology (and in one case, NeuroSky, rebuilt the technology from the ground up) to create inexpensive devices based on EEG. Two of these companies, NeuroSky and OCZ, have even built commercial EEG devices retailing for under 100$.
- In 2007 NeuroSky released the first affordable consumer based EEG along with the game NeuroBoy. This was also the first large scale EEG device to use dry sensor technology.[36]
- In 2008 OCZ Technology developed device for use in video games relying primarily on electromyography.
- In 2008 the Final Fantasy developer Square Enix announced that it was partnering with NeuroSky to create a game, Judecca.[37][38]
- In 2009 Mattel partnered with NeuroSky to release the Mindflex, a game that used an EEG to steer a ball through an obstacle course. By far the best selling consumer based EEG to date. ,[37][39]
- In 2009 Uncle Milton Industries partnered with NeuroSky to release the StarWars Force Trainer, a game designed to create the illusion of possessing the force.[37][40]
- In 2009 Emotiv released the EPOC, a 14 channel EEG device. The EPOC is the first commercial BCI to not use dry sensor technology, requiring users to apply a saline solution to their head.[41]
- In 2010 NeuroSky added blink an electromyography function to the MindSet.[42]
Images
 Person wearing electrodes for EEG |
 Portable recording device for EEG |
 EEG electroencephalophone used during a music performance in which bathers from around the world were networked together as part of a collective musical performance, using their brainwaves to control sound, lighting, and the bath environment |
See also
- Binaural beats
- Brain-computer interface
- Brainwave synchronization
- Comparison of consumer brain-computer interface devices
- Direct brain interfaces
- EEG measures during anesthesia
- Electropalatograph
- European data format
- Event-related potential
- Evoked potential
- Hemoencephalography
- Induced activity
- Local field potentials
- Magnetoencephalography
- Mind machine
- Neural oscillations
- Neurofeedback
- Ongoing brain activity
- Intracranial EEG
References
- ↑ A Hydrocel Geodesic Sensor Net by Electrical Geodesics, Inc.
- ↑ 2.0 2.1 2.2 2.3 Niedermeyer E, Lopes da Silva F (2004). Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. Lippincot Williams & Wilkins.
- ↑ Atlas of EEG & Seizure Semiology. B. Abou-Khalil; Musilus, K.E.; Elsevier, 2006.
- ↑ Creutzfeldt OD, Watanabe S, Lux HD (1966). "Relations between EEG phenomena and potentials of single cortical cells. I. Evoked responses after thalamic and epicortical stimulation". Electroencephalogr Clin Neurophysiol 20 (1): 1–18. doi:10.1016/0013-4694(66)90136-2. PMID 4161317.
- ↑ 5.0 5.1 Nunez PL, Srinivasan R (1981). Electric fields of the brain: The neurophysics of EEG. Oxford University Press.
- ↑ Hamalainen M, Hari R, Ilmoniemi RJ, Knuutila J, Lounasmaa OV (1993). "Magnetoencphalography - Theory, instrumentation, and applications to noninvasive studies of the working human brain". Reviews of Modern Physics 65: 413–497. doi:10.1103/RevModPhys.65.413.
- ↑ Buzsaki G (2006). Rhythms of the brain. Oxford University Press.
- ↑ Klein, S., & Thorne, B. M. (2007). Biological psychology. New York, N.Y.: Worth.
- ↑ Whittingstall K, Logothetis NK. (2009). Frequency-band coupling in surface EEG reflects spiking activity in monkey visual cortex. Neuron. 64(2):281-9. PMID 19874794
- ↑ Towle VL, Bolaños J, Suarez D, Tan K, Grzeszczuk R, Levin DN, Cakmur R, Frank SA, Spire JP. (1993). "The spatial location of EEG electrodes: locating the best-fitting sphere relative to cortical anatomy". Electroencephalogr Clin Neurophysiol 86 (1): 1–6. doi:10.1016/0013-4694(93)90061-Y. PMID 7678386.
- ↑ H. Aurlien, I.O. Gjerde, J. H. Aarseth, B. Karlsen, H. Skeidsvoll, N. E. Gilhus (March 2004). "EEG background activity described by a large computerized database.". Clinical Neurophysiology 115 (3): 665–673. doi:10.1016/j.clinph.2003.10.019. PMID 15036063.
- ↑ Nunez PL, Pilgreen KL (1991). "The spline-Laplacian in clinical neurophysiology: a method to improve EEG spatial resolution". J Clin Neurophysiol 8 (4): 397–413. doi:10.1097/00004691-199110000-00005. PMID 1761706.
- ↑ J. Anderson, Cognitive Psychology and It's Implications, 6th Ed., 2005, Worth Publishers, New York, NY, 17 pp.
- ↑ Cahn BR, & Polich J. (2006). Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychological Bulletin. 132 (2), 180-211.
- ↑ Pfurtscheller G, Lopes da Silva FH (1999). "Event-related EEG/MEG synchronization and desynchronization: basic principles". Clin Neurophysiol 110 (11): 1842–1857. doi:10.1016/S1388-2457(99)00141-8. PMID 10576479.
- ↑ Barry, W., Jones, G.M., 1965. Influence of eye lid movement upon electro- oculographic recording of vertical eye movements. Aerospace medicine 36, 855-858
- ↑ Iwasaki, M., Kellinghaus, C., Alexopoulos, A.V., Burgess, R.C., Kumar, A.N., Han, Y.H., Lüders, H.O., Leigh, R.J., 2005. Effects of eyelid closure, blinks, and eye movements on the electroencephalogram. Clinical Neurophysiology 116, 878-885
- ↑ Lins, O.G., Picton, T.W., Berg, P., Scherg, M., 1993. Ocular artifacts in EEG and event-related potentials I: Scalp topography. Brain Topography 6, 51-63.
- ↑ Keren, A.S., Yuval-Greenberg, S., Deouell, L.Y., 2010. Saccadic spike potentials in gamma-band EEG: Characterization, detection and suppression. Neuroimage 49, 2248-2263.
- ↑ Yuval-Greenberg, S., Tomer, O., Keren, A.S., Nelken, I., Deouell, L.Y., 2008. Transient Induced Gamma-Band Response in EEG as a Manifestation of Miniature Saccades. Neuron 58, 429-441.
- ↑ Keren, A.S., Yuval-Greenberg, S., Deouell, L.Y., 2010. Saccadic spike potentials in gamma-band EEG: Characterization, detection and suppression. Neuroimage 49, 2248-2263.
- ↑ Epstein, Charles M. (1983). Introduction to EEG and evoked potentials. J. B. Lippincot Co.. ISBN 0-397-50598-1.
- ↑ Keren, A.S., Yuval-Greenberg, S., Deouell, L.Y., 2010. Saccadic spike potentials in gamma-band EEG: Characterization, detection and suppression. Neuroimage 49, 2248-2263.
- ↑ Jung, T.P., Makeig, S., Humphries, C., Lee, T., McKeown, M.J., Iragui, V., Sejnowski, T.J., 2000a. Removing electroencephalographic artifacts by blind source separation. Psychophysiology 37, 163-178
- ↑ Jung, T.P., Makeig, S., Westerfield, M., Townsend, J., Courchesne, E., Sejnowski, T.J., 2000b. Removal of eye activity artifacts from visual event-related potentials in normal and clinical subjects. Clinical Neurophysiology 111, 1745-1758
- ↑ Joyce, C.A., Gorodnitsky, I.F., Kutas, M., 2004. Automatic removal of eye movement and blink artifacts from EEG data using blind component separation. Psychophysiology 41, 313-325
- ↑ A. S. Keren, S. Yuval-Greenberg, and L. Y. Deouell, “Saccadic spike potentials in gamma-band EEG: Characterization, detection and suppression,” Neuroimage, vol. 49, no. 3, pp. 2248-2263
- ↑ Shackman, A.J., McMenamin, B.W., Maxwell, J.S., Greischar, L.L., Davidson, R.J., 2010. Identifying robust and sensitive frequency bands for interrogating neural oscillations. NeuroImage vol. no. 4, 51, pp. 1319-1333
- ↑ Nolan, H., Whelan, R., & Reilly, R.B. FASTER: Fully Automated Statistical Thresholding for EEG artifact Rejection. (2010). Journal of Neuroscience Methods, 192, 152-162
- ↑ Montez T, Poil S-S, Jones BF, Manshanden I, Verbunt JPA, van Dijk BW, Brussaard AB, van Ooyen A, Stam CJ, Scheltens P, Linkenkaer-Hansen K (2009). "Altered temporal correlations in parietal alpha and prefrontal theta oscillations in early-stage Alzheimer disease". PNAS 106 (5): 1614–1619. doi:10.1073/pnas.0811699106. PMID 19164579. PMC 2635782. http://www.pnas.org/content/106/5/1614.abstract.
- ↑ Swartz, B.E; Goldensohn, ES (1998). "Timeline of the history of EEG and associated fields" (PDF). Electroencephalography and clinical Neurophysiology 106 (2): 173–176. doi:10.1016/S0013-4694(97)00113-2. PMID 9741779. http://www.sciencedirect.com/science?_ob=MImg&_imagekey=B6SYX-4FV4S6H-1-1&_cdi=4846&_user=10&_orig=browse&_coverDate=02%2F28%2F1998&_sk=998939997&view=c&wchp=dGLbVzz-zSkWb&md5=47fbbe7e51a806779716fba415b96ab7&ie=/sdarticle.pdf.
- ↑ Pravdich-Neminsky VV. Ein Versuch der Registrierung der elektrischen Gehirnerscheinungen (In German). Zbl Physiol 27: 951–960, 1913.
- ↑ [1] 1 Apr 2009, Japan Times
- ↑ This brain test maps the truth 21 Jul 2008, 0348 hrs IST, Nitasha Natu,TNN
- ↑ Katie, Drummond; Noah Schachtman (2009-05-14). "Pentagon Preps Soldier Telepathy Push". Wired. http://www.wired.com/dangerroom/2009/05/pentagon-preps-soldier-telepathy-push/. Retrieved 2009-06-14.
- ↑ "Mind Games". The Economist. 2007-03-23. http://www.economist.com/science/displaystory.cfm?story_id=8847846.
- ↑ 37.0 37.1 37.2 "Mind reading is on the market". Los Angeles Times. 2010-08-08. http://www.latimes.com/business/la-fi-mind-reader-20100808,0,6235181,full.story.
- ↑ http://www.engadget.com/2008/10/09/brains-on-with-neurosky-and-squareenixs-judecca-mind-control-ga/
- ↑ http://www.physorg.com/news150781868.html
- ↑ Snider, Mike (2009-01-07). "Toy trains 'Star Wars' fans to use The Force". USA Today. http://www.usatoday.com/life/lifestyle/2009-01-06-force-trainer-toy_N.htm. Retrieved 2010-05-01.
- ↑ "Emotiv Systems Homepage". Emotiv.com. http://emotiv.com/. Retrieved 2009-12-29.
- ↑ http://www.gamasutra.com/view/news/29190/NeuroSky_Upgrades_SDK_Allows_For_Eye_Blink_BrainwavePowered_Games.php
External links
- Scholarpedia EEG
- FASTER A fully automated, unsupervised method for processing of high density EEG data. FASTER has been peer-reviewed, it is free and the software is open source.
|
||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||