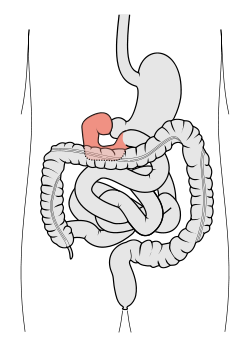
Duodenum
| Duodenum | |
|---|---|
 |
|
| Schematic diagram of the gastrointestinal tract, highlighting the duodenum. | |
| Gray's | subject #248 1169 |
| Artery | Inferior pancreaticoduodenal artery, Superior pancreaticoduodenal artery |
| Vein | Pancreaticoduodenal veins |
| Nerve | celiac ganglia, vagus [1] |
| Precursor | Foregut (1st and 2nd parts), Midgut (3rd and 4th part) |
| MeSH | duodenum |
| Dorlands/Elsevier | Duodenum |
The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In fish, the divisions of the small intestine are not as clear and the terms anterior intestine or proximal intestine may be used instead of duodenum.[2] In mammals the duodenum may be the principal site for iron absorption.[3]
The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine, where most chemical digestion takes place. The name duodenum is from the Latin duodenum digitorum, or twelve fingers' breadths.
In humans, the duodenum is a hollow jointed tube about 25-30 cm (10-12 in) long[4] connecting the stomach to the jejunum. It begins with the duodenal bulb and ends at the ligament of Treitz.
Contents |
Function
The duodenum is largely responsible for the breakdown of food in the small intestine, using enzymes. Brunner's glands, which secrete mucus, are found in the duodenum. The duodenum wall is composed of a very thin layer of cells that form the muscularis mucosae. The duodenum is almost entirely retroperitoneal.
The duodenum also regulates the rate of emptying of the stomach via hormonal pathways. Secretin and cholecystokinin are released from cells in the duodenal epithelium in response to acidic and fatty stimuli present there when the pylorus opens and releases gastric chyme into the duodenum for further digestion. These cause the liver and gall bladder to release bile, and the pancreas to release bicarbonate and digestive enzymes such as trypsin, lipase and amylase into the duodenum as they are needed.
New studies have shown that around 80% of obese people who had gastric bypass surgery (bypassing the duodenum) were cured of their type 2 diabetes. However, the disappearance of their diabetes came long before the actual weight loss. When the same operation was performed on diabetic rats, they too were rid of their diabetes. However, when the operation was reversed in the animals, the diabetes returned. This shows that preventing food from entering the duodenum can have a dramatic impact on people suffering from type 2 diabetes.[5]
It is most likely that one of the digestive additives produced by the Duodenum on entry of food in to it (or a secondary product) is absorbed by the jejunum and ileum and spread into the body instead of passing through the digestive system. The presence of those chemicals causes the muscles to exhibit insulin resistance and ultimately Type 2 Diabetes. Identification of these chemicals may lead to a cure for type 2 diabetes.
Sections
The duodenum is divided into four sections for the purposes of description. The first three sections curve in a "C"-loop concavity in which the head of the pancreas lies. Only the first 2 cm of the superior part is mobile (covered by peritoneum) - the distal 3cm of the first part along with the rest of the duodenum is retroperitoneal (immobile).

First part
The first (superior) part begins as a continuation of the duodenal end of the pylorus. From here it passes laterally (right), superiorly and posteriorly, for approximately 5 cm, before making a sharp curve inferiorly into the superior duodenal flexure (the end of the superior part). It is intraperitoneal.
Relations
- Anterior
- Peritoneum
- Gallbladder
- Quadrate lobe of liver
- Posterior
- Bile duct
- Gastroduodenal artery
- Portal vein
- IVC
- Superior
- Neck of gallbladder
- Hepatoduodenal ligament (lesser omentum)
- Inferior
- Neck of pancreas
- Greater omentum
Second part
The second (descending) part of the duodenum begins at the superior duodenal flexure. It passes inferiorly to the lower border of vertebral body L3, before making a sharp turn medially into the inferior duodenal flexure (the end of the descending part).
The pancreatic duct and common bile duct enter the descending duodenum, commonly known together as the hepatopancreatic duct (or pancreatic duct in the United States), through the major duodenal papilla (known as Ampulla of Vater). This part of the duodenum also contains the minor duodenal papilla, the entrance for the accessory pancreatic duct. The junction between the embryological foregut and midgut lies just below the major duodenal papilla.
Third part
The third (inferior/horizontal) part of the duodenum begins at the inferior duodenal flexure and passes transversely to the left, crossing the right ureter, right testicular/ovarian vessels, inferior vena cava, abdominal aorta, superior mesenteric artery and the vertebral column.
Fourth part
The fourth (ascending) part passes superiorly, either anterior to, or to the right of, the aorta, until it reaches the inferior border of the body of the pancreas. Then, it curves anteriorly and terminates at the duodenojejunal flexure where it joins the jejunum. The duodenojejunal flexure is surrounded by a peritoneal fold containing muscle fibres: the ligament of Treitz.
Blood Supply
The duodenum receives arterial blood from two different sources. The transition between these sources is important as it determines the foregut from the midgut. Proximal to the 2nd part of the duodenum (approximately at the major duodenal papilla - where the bile duct enters) the arterial supply is from the gastroduodenal artery and its branch the superior pancreaticoduodenal artery. Distal to this point (the midgut) the arterial supply is from the superior mesenteric artery, and its branch the inferior pancreaticoduodenal artery supplies the 3rd and 4th sections. The superior and inferior pancreaticoduodenal arteries (from the gastroduodenal artery and SMA respectively) form an anastomotic loop between the celiac trunk and the SMA; so there is potential for collateral circulation here.
The venous drainage of the duodenum follows the arteries. Ultimately these veins drain into the portal system, either directly or indirectly through the splenic or superior mesenteric vein.
Lymphatic Drainage
The lymphatic vessels follow the arteries in a retrograde fashion. The anterior lymphatic vessels drain into the pancreatoduodenal lymph nodes located along the superior and inferior pancreatoduodenal arteries and then into the pyloric lymph nodes (along the gastroduodenal artery). The posterior lymphatic vessels pass posterior to the head of the pancreas and drain into the superior mesenteric lymph nodes. Efferent lymphatic vessels from the duodenal lymph nodes ultimately pass into the celiac lymph nodes.
Additional images
 The celiac artery and its branches; the stomach has been raised and the peritoneum removed. |
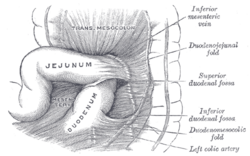 Superior and inferior duodenal fossæ. |
 Duodenojejunal fossa. |
 Interior of the stomach. |
 Section of duodenum of cat. X 60. |
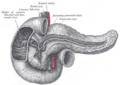
 The pancreas and duodenum from behind. |
 Transverse section through the middle of the first lumbar vertebra, showing the relations of the pancreas. |
 The pancreatic duct. |
 Duodenum with amyloid deposition in lamina propria. |
 Region of pancreas |
 Stomach |
Duodenum with brush border (microvillus) |
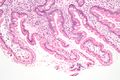 Micrograph showing gardiasis on a duodenal biopsy. H&E stain. |
References
- ↑ Physiology at MCG 6/6ch2/s6ch2_30
- ↑ Guillaume, Jean; Praxis Publishing, Sadasivam Kaushik, Pierre Bergot, Robert Metailler (2001). Nutrition and Feeding of Fish and Crustaceans. Springer. p. 31. ISBN 1852332417, 9781852332419. http://books.google.com/?id=As0flTZo_EAC&pg=PA31&lpg=PA31&dq=fish+cytology+jejunum+duodenum. Retrieved 2009-01-09.
- ↑ Latunde-Dada GO, Van der Westhuizen J, Vulpe CD et al. (2002). "Molecular and functional roles of duodenal cytochrome B (Dcytb) in iron metabolism". Blood Cells Mol. Dis. 29 (3): 356–60. doi:10.1006/bcmd.2002.0574. PMID 12547225.
- ↑ CT of the Duodenum: An Overlooked Segment Gets Its Due
- ↑ The Bypass Effect On Diabetes, Cancer
- 60 Minutes "The Bypass Effect On Diabetes, Cancer" April 20, 2008
External links
- duodenum at The Anatomy Lesson by Wesley Norman (Georgetown University)
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||