Ayurveda

The Hindu god of ayurveda, Dhanvantari.
|
| Acupuncture · Anthroposophic medicine · Ayurveda · Chiropractic · Herbalism · Homeopathy · Naturopathy · Osteopathy · Siddha medicine · Traditional medicine (Chinese · Mongolian · Tibetan) · Unani |
| NCCAM classifications |
| Whole medical systems · Mind-body interventions · Biologically based therapies · Manipulative therapy · Energy therapies |
| See also |
| Alternative medicine · Glossary · People |
Ayurveda (Sanskrit: आयुर्वेद; Āyurveda, the "science of life") Ayurvedic medicine is a system of traditional medicine native to the Indian subcontinent[1] and practiced in other parts of the world as a form of alternative medicine.[2] In Sanskrit, the word ayurveda consists of the words āyus, meaning "longevity", and veda, meaning "related to knowledge" or "science".[1] Evolving throughout its history, ayurveda remains an influential system of medicine in South Asia.[3] The earliest literature on Indian medical practice appeared during the Vedic period in India.[2] The Suśruta Saṃhitā and the Charaka Saṃhitā were influential works on traditional medicine during this era.[2] Over the following centuries, Ayurvedic practitioners developed a number of medicinal preparations and surgical procedures for the treatment of various ailments and diseases.[4]
In Western medicine, Ayurveda is classified as a system of complementary and alternative medicine (CAM) that is used to complement, rather than replace, the treatment regimen and relationship that exists between a patient and their existing physician.[5]
Contents |
Overview

Ayurveda is grounded in a metaphysics of the "five great elements" (Devanāgarī: [महा] पञ्चभूत;Prithvi- earth, Aap-water, Tej-fire, Vaayu-air and Akash-ether)—all of which compose the Universe, including the human body.[1] Chyle or plasma (called rasa dhatu), blood (rakta dhatu), flesh (mamsa dhatu), fat (medha dhatu), bone (asthi dhatu), marrow (majja dhatu), and semen or female reproductive tissue (shukra dhatu) are held to be the seven primary constituent elements -- saptadhatu (Devanāgarī: सप्तधातु) of the body.[6] Ayurveda deals elaborately with measures of healthful living during the entire span of life and its various phases. Ayurveda stresses a balance of three elemental energies or humors: vata (air & space – "wind"), pitta (fire & water – "bile") and kapha (water & earth – "phlegm"). According to ayurveda, these three regulatory principles— Doshas (literally that which deteriorates - Devanāgarī: त्रिदोष)—are important for health, because when they are in balanced state, the body is healthy, and when imbalanced, the body has diseases. Ayurveda holds that each human possesses a unique combination of Doshas. In ayurveda, the human body perceives attributes of experiences as 20 Guna (Devanāgarī: गुण, meaning qualities).[7] Surgery and surgical instruments are employed.[7] It is believed that building a healthy metabolic system, attaining good digestion, and proper excretion leads to vitality.[7] Ayurveda also focuses on exercise, yoga, meditation, and massage.[8] Thus, body, mind, and spirit/consciousness need to be addressed both individually and in unison for health to ensue.
The practice of Panchakarma (Devanāgarī: पंचकर्म) is believed to eliminate toxic elements from the body.[9]
Eight disciplines of ayurveda treatment, called ashtangas (Devanāgarī: अष्टांग), are given below:[10]
- Internal medicine (Kaaya-chikitsa)
- Paediatrics (Kaumarabhrtyam)
- Surgery (Shalya-chikitsa)
- Eye and ENT (Shalakya tantra)
- Demonic possession (Bhuta vidya): Bhuta vidya has been called psychiatry.[2]
- Toxicology (Agadatantram)
- Prevention diseases and improving immunity and rejuvenation (rasayana)
- Aphrodisiacs and improving health of progeny (Vajikaranam)
In Hindu mythology, the origin of Ayurveda medicine is attributed to the physician of the gods, Dhanvantari.[11]
Practices

Balance
Hinduism and Buddhism have been an influence on the development of many of ayurveda's central ideas — particularly its fascination with balance, known in Buddhism as Mādhyamaka (Devanāgarī: माध्यात्मिक).[13] Balance is emphasized; suppressing natural urges is seen to be unhealthy, and doing so may almost certainly lead to illness.[13] However, people are cautioned to stay within the limits of reasonable balance and measure.[13] For example, emphasis is placed on moderation of food intake[1], sleep, sexual intercourse, and the intake of medicine.[13]
Diagnosis
The Charaka Samhita recommends a tenfold examination of the patient.[14] The qualities to be judged are:[14]
- constitution
- abnormality
- essence
- stability
- body measurements
- diet suitability
- psychic strength
- digestive capacity
- physical fitness
- age
In addition, Chopra (2003) identifies five influential criteria for diagnosis:[14]
- origin of the disease
- prodrominal (precursory) symptoms
- typical symptoms of the fully developed disease
- observing the effect of therapeutic procedures
- the pathological process'
Ayurvedic practitioners approach diagnosis by using all five senses.[14] Hearing is used to observe the condition of breathing and speech.[6] The study of the vital pressure points or marma is of special importance.[7]
Hygiene
Hygiene is an Indian cultural value and a central practice of Ayurvedic medicine.[6] Hygienic living involves regular bathing, cleansing of teeth, skin care, and eye washing.[6] Occasional anointing of the body with oil is also prescribed.[6]

Treatments
Ayurveda stresses the use of plant-based medicines and treatments.[6] Hundreds of plant-based medicines are employed, including cardamom and cinnamon.[6] Some animal products may also be used, for example milk, bones, and gallstones.[6] In addition, fats are used both for consumption and for external use.[6] Minerals, including sulfur, arsenic, lead, copper sulfate and gold are also consumed as prescribed.[6] This practice of adding minerals to herbal medicine is known as rasa shastra.
In some cases, alcohol is used as a narcotic for the patient undergoing an operation.[6] The advent of Islam introduced opium as a narcotic.[10] Both oil and tar are used to stop bleeding.[6] Traumatic bleeding is said to be stopped by four different methods ligation of the blood vessel; cauterisation by heat; using different herbal or animal preparations locally which facilitate clotting; and different medical preparations which constrict the bleeding or oozing vessels. Different oils may be used in a number of ways including regular consumption as a part of food, anointing, smearing, head massage, and prescribed application to infected areas.[17]
Shrotas
Ensuring the proper functions of channels (shrotas) that transport fluids from one point to another is a vital goal of Ayurvedic medicine, because the lack of healthy shrotas is thought to cause rheumatism, epilepsy, paralysis, convulsions, and insanity. Practitioners induce sweating and prescribe steam-based treatments as a means to open up the channels and dilute the Doshas that cause the blockages and lead to disease.[18]
History

Around 1500 BC, ayurveda's fundamental and applied principles got organised and enunciated. Ayurveda traces its origins to the Vedas, Atharvaveda in particular, and is connected to Hindu religion. Atharvaveda (one of the four most ancient books of Indian knowledge, wisdom and culture) contains 114 hymns or formulations for the treatment of diseases. Ayurveda originated in and developed from these hymns. In this sense, ayurveda is considered by some to have divine origin. Indian medicine has a long history, and is one of the oldest organised systems of medicine. Its earliest concepts are set out in the sacred writings called the Vedas, especially in the metrical passages of the Atharvaveda, which may possibly date as far back as the 2nd millennium BC. According to a later writer, the system of medicine was received by a man named Dhanvantari from Brahma, and Dhanvantari was deified as the god of medicine. In later times his status was gradually reduced, until he was credited with having been an earthly king.[6] The Sushruta Samhita of Sushruta appeared during the 1st millennium BC.[4] Dwivedi & Dwivedi (2007) – on the work of the surgeon Sushruta – write:[4]
"The main vehicle of the transmission of knowledge during that period was by oral method. The language used was Sanskrit — the vedic language of that period (2000–500 BC). The most authentic compilation of his teachings and work is presently available in a treatise called Sushruta Samhita. This contains 184 chapters and description of 1,120 illnesses, 700 medicinal plants, 64 preparations from mineral sources and 57 preparations based on animal sources."
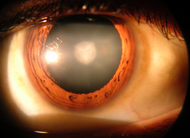
Underwood & Rhodes (2008) hold that this early phase of traditional Indian medicine identified 'fever (takman), cough, consumption, diarrhea, dropsy, abscesses, seizures, tumours, and skin diseases (including leprosy)'.[6] Treatment of complex ailments, including angina pectoris, diabetes, hypertension, and stones, also ensued during this period.[4][20] Plastic surgery, cataract surgery, puncturing to release fluids in the abdomen, extraction of foreign elements, treatment of anal fistulas, treating fractures, amputations, cesarean sections, and stitching of wounds were known.[6] The use of herbs and surgical instruments became widespread.[6] The Charaka Samhita text is arguably the principal classic reference. It gives emphasis to the triune nature of each person: body care, mental regulation, and spiritual/consciousness refinement.
Other early works of ayurveda include the Charaka Samhita, attributed to Charaka.[6] The earliest surviving excavated written material which contains the works of Sushruta is the Bower Manuscript, dated to the 4th century AD.[22] The Bower manuscript quotes directly from Sushruta and is of special interest to historians due to the presence of Indian medicine and its concepts in Central Asia.[23] Vagbhata, the son of a senior doctor by the name of Simhagupta,[24] also compiled his works on traditional medicine.[6] Early ayurveda had a school of physicians and a school of surgeons.[2] Tradition holds that the text Agnivesh tantra, written by the sage Agnivesh, a student of the sage Bharadwaja, influenced the writings of ayurveda.[25]
The Chinese pilgrim Fa Hsien (ca. 337–422 AD) wrote about the health care system of the Gupta empire (320–550) and described the institutional approach of Indian medicine, also visible in the works of Charaka, who mentions a clinic and how it should be equipped.[26] Madhava (fl. 700), Sarngadhara (fl. 1300), and Bhavamisra (fl. 1500) compiled works on Indian medicine.[23] The medical works of both Sushruta and Charaka were translated into the Arabic language during the Abbasid Caliphate (ca. 750).[27] These Arabic works made their way into Europe via intermediaries.[27] In Italy, the Branca family of Sicily and Gaspare Tagliacozzi (Bologna) became familiar with the techniques of Sushruta.[27]
British physicians traveled to India to see rhinoplasty being performed by native methods.[28] Reports on Indian rhinoplasty were published in the Gentleman's Magazine in 1794.[28] Joseph Constantine Carpue spent 20 years in India studying local plastic surgery methods.[28] Carpue was able to perform the first major surgery in the western world in 1815.[29] Instruments described in the Sushruta Samhita were further modified in the Western World.[29]
Current status
Within India
.jpg)
In 1970, the Indian Medical Central Council Act which aims to standardize qualifications for ayurveda and provide accredited institutions for its study and research was passed by the Parliament of India.[30] In India, over 100 colleges offer degrees in traditional ayurvedic medicine.[8] The Indian government supports research and teaching in ayurveda through many channels at both the national and state levels, and helps institutionalize traditional medicine so that it can be studied in major towns and cities.[31] The state-sponsored Central Council for Research in Ayurveda and Siddha (CCRAS) is the premier institution for promotion of traditional medicine in India.[32] The studies conducted by this institution encompass clinical, drug, literary, and family welfare research.[32] To fight biopiracy and unethical patents, the Government of India, in 2001, set up the Traditional Knowledge Digital Library as repository of 1200 formulations of various systems of Indian medicine, such as Ayurveda, Unani and Siddha.[33][34] The library also has 50 traditional Ayurveda books digitized and available online.[35]
Central Council of Indian Medicine (CCIM) a statutory body established in 1971, under Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH), Ministry of Health and Family Welfare, Government of India, monitors higher education in Ayurveda.[36] The Bachelor of Ayurveda, Medicine and Surgery (BAMS) degree is the basic five-and-a-half year course of graduation. It includes eighteen different subjects comprising courses on anatomy with cadaver dissections, physiology, pharmacology, pathology, modern clinical medicine & clinical surgery, pediatrics, along with subjects on ayurveda like Charaka Samhita, history and evolution of ayurveda, identification and usage of herbs (dravyaguna), and ayurvedic philosophy in diagnostics and treatment.
Many clinics in urban and rural areas are run by professionals who qualify from these institutes.[30] Mukherjee & Wahile cite World Health Organization statistics to demonstrate the popularity of traditional medicine as the primary system of health care.[37]
Outside India
Academic institutions related to traditional medicine in India have contributed to ayurveda's international visibility.[38] Kurup (2003) comments on the role of Gujarat Ayurved University:[38]
Several international and national initiatives have been formed to legitimize the practice of Ayurvedic medicine as CAM in countries outside India:
- WHO policy of traditional medicine practice [39]
- The US National Center for Complementary and Alternative Medicine [40]
- The National Ayurvedic Medical Association[41]
- The European Federation for Complementary and Alternative Medicine[42]
- The European Ayurveda Association[43]
In 2009, the United States of America National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health expended $1.2 million[44] of its $123 million annual budget on ayurvedic medicine-related research.
Due to different laws and medical regulations in the rest of the world, the unregulated practice and commercialization of Ayurvedic medicine has raised ethical and legal issues; in some cases, this damages the reputation of Ayurvedic medicine outside India.[45][46][47]
Journals
A variety of peer reviewed journals focus on the topic of ayurvedic medicine:
- Ancient Science of Life[48]
- Theoretical and Experimental Journal of Ayurveda and Siddha[49]
- Journal of Research & Education in Indian Medicine (JREIM),[50]
- AYU[51]
- The International Journal for Ayurveda Research[52]
None of the journals except IJAR[53] are PubMed indexed. The first subspeciality journal for the field of Ayurvedic medicine was launched in July 2010[54]. It's focus is rheumatology and it is titled the Journal of Clinical Rheumatology in Ayurveda[55].
Patents
In December 1993, the University of Mississippi Medical Center had a patent issued to them by United States Patent and Trademark Office on the use of turmeric for healing.[56] The patent was contested by India's industrial research organization, Council for Scientific and Industrial Research (CSIR), on the grounds that traditional ayurvedic practitioners were already aware of the healing properties of the substance for centuries, and that this prior art made the patent a case of bio-piracy.[57] The Government of India had become involved in promoting traditional medicine by 1997.[3] R A Mashelkar, director-general of the Indian Council of Scientific and Industrial Research, made the following observation:[58]
"This is a significant development of far-reaching consequences for the protection of the traditional knowledge base in the public domain, which has been an emotional issue for not only the people of India but also for the other third world countries."
Scientific evidence
.svg.png)

As a traditional medicine, many ayurveda products have not been tested in rigorous scientific studies and clinical trials.In India, research in ayurveda is largely undertaken by the statutory body of the Central Government, the Central Council for Research in Ayurveda and Siddha (CCRAS), through a national network of research institutes.[60] A systematic review of ayurveda treatments for rheumatoid arthritis concluded that there was insufficient evidence, as most of the trials were not done properly, and the one high-quality trial showed no benefits.[61] A review of ayurveda and cardiovascular disease concluded that while the herbal evidence is not yet convincing, the spices are appropriate, some herbs are promising, and yoga is also a promising complementary treatment.[62]
Some ayurvedic products, mainly herbs used for phytotherapy, have been tested with promising results. Studies suggest that Turmeric and its derivative curcumin are antioxidants.[63][64] Tinspora cordifolia has been tested.[65] Among the medhya rasayanas (intellect rejuvenation), two varieties of Salvia have been tested in small trials; one trial provided evidence that Salvia lavandulifolia (Spanish sage) may improve word recall in young adults,[66] and another provided evidence that Salvia officinalis (Common sage) may improve symptoms in Alzheimer's patients.[67] In some cases, ayurvedic medicine may provide clues to therapeutic compounds. For example, derivatives of snake venom have various therapeutic properties.[68] Many plants used as rasayana (rejuvenation) medications are potent antioxidants.[69] Neem appears to have beneficial pharmacological properties.[70]


Mitra & Rangesh (2003) hold that cardamom and cinnamon stimulate digestive enzymes that break down polymeric macromolecules in the human body.[16] Research suggests that T. arjuna is useful in alleviating the of angina pectoris and in treating heart failure and coronary artery disease.[59] T. arjuna may also be useful in treating hypercholesterolemia.[59]


Safety
Rasa shastra, the practice of adding metals, minerals or gems to herbs, is a source of toxic heavy metals such as lead, mercury and arsenic.[73] Adverse reactions to herbs due to their pharmacology are described in traditional ayurvedic texts, but ayurvedic practitioners are reluctant to admit that herbs could be toxic and the reliable information on herbal toxicity is not readily available.[74]
A 2004 study found such toxic metals in 20% of ayurvedic preparations that were made in South Asia for sale around Boston and extrapolated the data to the United States more broadly. It concluded that excess consumption of these products could cause health risks.[75] A 2008 study of more than 230 products found that approximately 20% of remedies (and 40% of rasa shastra medicines) purchased over the Internet from both US and Indian suppliers contained lead, mercury or arsenic.[73][76][77]
Traditionally the toxicity of these materials are believed to be reduced through purification processes such as samskaras or shodhanas (for metals), which is similar to the Chinese pao zhi, although the ayurvedic technique is more complex and may involve prayers as well as physical pharmacy techniques. One medical journal reported:
"Crude aconite is an extremely lethal substance, yet ayurveda looks upon it as a therapeutic entity. Crude aconite is always processed, i.e. it undergoes 'samskaras' before being utilised in the Ayurvedic formulations. This study was undertaken in mice, to ascertain whether "processed" aconite is less toxic as compared to the crude or unprocessed one. It was seen that crude aconite was significantly toxic to mice (100% mortality at a dose of 2.6 mg/mouse) whereas the fully processed aconite was absolutely non-toxic (no mortality at a dose even 8 times as high as that of crude aconite). Further, all the steps in the processing were essential for complete detoxification."[78][79]
Following concerns about metal toxicity, the Government of India ruled that ayurvedic products must specify their metallic content directly on the labels of the product.[80] The harmful effects of the samples is attributed in part to the adulterated raw material and lack of workers trained in traditional medicine.[81] In a letter to the Indian Academy of Sciences, director of the Interdisciplinary School of Health Sciences, University of Pune Patwardhan Bhushan stated that the metal adulteration is due to contamination and carelessness during the much faster modern manufacturing processes, and does not occur with traditional methods of preparation.[82]
Notes
- ↑ 1.0 1.1 1.2 1.3 Chopra, p. 75
- ↑ 2.0 2.1 2.2 2.3 2.4 "Ayurveda". New Delhi, India: Department of Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy, Ministry of Health & Family Welfare, Government of India. http://indianmedicine.nic.in/ayurveda.asp.
- ↑ 3.0 3.1 Sharma, H. M.; Bodeker, Gerard C (1997). "Alternative Medicine (medical system)". Encyclopædia Britannica (2008 ed. ed.).
- ↑ 4.0 4.1 4.2 4.3 Dwivedi & Dwivedi (2007)
- ↑ "A Closer Look at Ayurvedic Medicine". Focus on Complementary and Alternative Medicine (Bethesda, MD: National Center for Complementary and Alternative Medicine (NCCAM), US National Institutes of Health (NIH)) XII (4). Fall 2005/Winter 2006. http://nccam.nih.gov/news/newsletter/2006_winter/ayurveda.htm.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 Underwood & Rhodes (2008)
- ↑ 7.0 7.1 7.2 7.3 Chopra, p. 76
- ↑ 8.0 8.1 "Ayurveda". Encarta. Redmond, WA: Microsoft. 2008. http://encarta.msn.com/encyclopedia_761596196/Ayurveda.html.
- ↑ Sharma, A. K. (2003). "Panchkarma Therapy in Ayurvedic Medicine". In Mishra, Lakshmi Chandra. Scientific Basis for Ayurvedic Therapies. Boca Raton, FL: CRC Press. p. 43. ISBN 0-8493-1366-X.
- ↑ 10.0 10.1 Chopra, p. 80
- ↑ Dhanvantari. (2010). In Encyclopædia Britannica. Retrieved August 04, 2010, from Encyclopædia Britannica Online: http://www.britannica.com/EBchecked/topic/160641/Dhanvantari
- ↑ Clifford, Terry (2003). Tibetan Buddhist Medicine and Psychiatry. 42. Motilal Banarsidass Publications. ISBN 81-208-1784-2.
- ↑ 13.0 13.1 13.2 13.3 Wujastyk, p. XVIII
- ↑ 14.0 14.1 14.2 14.3 Chopra, p. 79
- ↑ Sahu, S. & Mishra, L. C. (2003) in "Benign Growths, Cysts, and Malignant Tumors", Scientific Basis for Ayurvedic Therapies edited by Mishra, L.C. 300. CRC Press: ISBN 0-8493-1366-X.
- ↑ 16.0 16.1 Mitra & Rangesh, p. 363
- ↑ Wujastyk, p. XX
- ↑ Wujastyk, pages XIX-XX
- ↑ Kasulis, Thomas P.; Aimes, Roger T.; Dissanayake, Wimal (1993). Self as Body in Asian Theory and Practice. Albany, NY: State University of New York Press. p. 104. ISBN 0-7914-1079-X.
- ↑ Lock et al., p. 836
- ↑ 21.0 21.1 21.2 Finger, p. 66
- ↑ Kutumbian, pages XXXII-XXXIII
- ↑ 23.0 23.1 Wujastyk, p. XXVI
- ↑ Wujastyk, p. 224
- ↑ Ṭhākara, Vināyaka Jayānanda (1989). Methodology of Research in Ayurveda. Jamnagar, India: Gujarat Ayurved University Press. p. 7.
- ↑ Wujastyk, pages XV-XVI
- ↑ 27.0 27.1 27.2 Lock et al., p. 607
- ↑ 28.0 28.1 28.2 Lock "et al., p. 651
- ↑ 29.0 29.1 Lock et al., p. 652
- ↑ 30.0 30.1 Wujastyk, p. XXII
- ↑ Wujastyk, p. XVI
- ↑ 32.0 32.1 Kurup, p. 7
- ↑ Traditional Knowledge Digital Library website.
- ↑ "Know Instances of Patenting on the UES of Medicinal Plants in India". PIB, Ministry of Environment and Forests. May 6, 2010. http://pib.nic.in/release/release.asp?relid=61511. Retrieved 22 May 2010.
- ↑ 50 Ayurveda books online Traditional Knowledge Digital Library (Govt. of India)
- ↑ CCIM
- ↑ Mukherjee, P. K.; Wahile, A. (January 3, 2006). "Integrated Approaches Towards Drug Development from Ayurveda and Other Indian System of Medicines". Journal of Ethnopharmacology 103 (1): 25–35.. http://www.ncbi.nlm.nih.gov/pubmed/16271286.
- ↑ 38.0 38.1 Kurup 2003, p. 6
- ↑ http://www.searo.who.int/meeting/rc/rc55/rc55-13.htm
- ↑ http://nccam.nih.gov/
- ↑ http://www.Ayurveda-nama.org/about_nama.php
- ↑ http://www.efcam.eu/
- ↑ http://p121583.mittwaldserver.info/
- ↑ NIH RePORTER, http://projectreporter.nih.gov/reporter_SearchResults.cfm?icde=4809741
- ↑ Skolnick, Andrew A. (1991). "The Maharishi Caper: Or How to Hoodwink Top Medical Journals". ScienceWriters (New York, NY: National Association of Science Writers) Fall. Archived from the original on Jul 16, 2008. http://web.archive.org/web/20080716041551/http://www.aaskolnick.com/naswmav.htm. Retrieved July 6, 2010.
- ↑ Skolnick, Andrew A. (1991). "Maharishi Ayur-Veda: Guru’s Marketing Scheme Promises the World Eternal 'Perfect Health'!". Journal of the American Medical Association (Chicago, IL: AMA) 266: 1741–1750. doi:10.1001/jama.266.13.1741.
- ↑ National Policy on Traditional Medicine and Regulation of Herbal Medicines - Report of a WHO Global Survey, http://apps.who.int/medicinedocs/pdf/s7916e/s7916e.pdf
- ↑ http://ayurvedajournals.org/index.php/asl
- ↑ http://ayurvedajournals.org/index.php/tejas/login
- ↑ "Journal of Research & Education in Indian Medicine". homepage. http://www.jreim.com. Retrieved May 1, 2009.
- ↑ "AYU: An International Quarterly Journal of Research in Ayurveda". homepage. http://www.ayujournal.org/. Retrieved August 30, 2010.
- ↑ "International Journal for Ayurveda Research". homepage. http://www.ijaronline.com/. Retrieved May 1, 2009.
- ↑ http://ijaronline.com/
- ↑ http://www.hindu.com/2010/07/15/stories/2010071551090300.htm
- ↑ http://www.ayurvedarheumatology.org
- ↑ US Patent No. 5,401,504
- ↑ Johnston, Barbara & Webb, Ginger (1997). "Turmeric Patent Overturned in Legal Victory". HerbalGram Fall 1997 (41): 11. http://web.ebscohost.com/ehost/detail?vid=7&hid=108&sid=ecc8454b-c5ab-4d0c-9358-e355356593fe%40sessionmgr103.
- ↑ Kumar, Sanjay. India wins battle with USA over turmeric patent. The Lancet, Volume 350, Issue 9079, Page 724, 6 September 1997. The Lancet, Volume 350, Issue 9079, Page 724, 6 September 1997
- ↑ 59.0 59.1 59.2 Miller, A. L. (1998). "Botanical Influences on Cardiovascular Disease". Alternative Medicine Review 3 (6): 422–431. PMID 9855567.
- ↑ "Central Council for Research in Ayurveda and Siddha (Government of India)". http://www.ccras.nic.in/.
- ↑ Park, J.; Ernst, E. (April 2005). "Ayurvedic Medicine for Rheumatoid Arthritis: A Systematic Review". Seminars in Arthritis and Rheumatism 34 (5): 705–713. doi:10.1016/j.semarthrit.2004.11.005. PMID 15846585.
- ↑ Mamtani, R.; Mamtani, R. (2005). "Ayurveda and Yoga in Cardiovascular Diseases". Cardiology Review 13 (3): 155–162. doi:10.1097/01.crd.0000128730.31658.36. PMID 15834238. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1061-5377&volume=13&issue=3&spage=155.
- ↑ Tilak, JC, M Banerjee, H Mohan, TP Devasagayam. "Antioxidant availability of turmeric in relation to its medicinal and culinary uses." Phytother Res. 2004 Oct;18(10):798-804.
- ↑ Aggarwal, B. B.; Sundaram, C.; Malani, N.; Ichikawa, H. (2007). "Curcumin: the Indian Solid Gold". Advances in Experimental Medicine and Biology 595: 1–75. doi:10.1007/978-0-387-46401-5_1. PMID 17569205.
- ↑ Panchabhai T.S., Kulkarni U.P., Rege N.N., TS; Kulkarni, UP; Rege, NN (April 2008). "Validation of therapeutic claims of Tinospora cordifolia: a review". Phytother Res 22 (4): 425–41. doi:10.1002/ptr.2347. PMID 18167043.
- ↑ Tildesley, N. T.; Kennedy, D. O.; Perry, E. K.; et al. (June 2003). "Salvia lavandulaefolia (Spanish Sage) Enhances Memory in Healthy Young Volunteers". Pharmacology Biochemistry and Behavior 75 (3): 669–674. doi:10.1016/S0091-3057(03)00122-9. PMID 12895685.
- ↑ Akhondzadeh, S.; Noroozian, M.; Mohammadi, M.; Ohadinia, S.; Jamshidi, A. H.; Khani M. (February 2003). "Salvia officinalis Extract in the Treatment of Patients with Mild to Moderate Alzheimer's Disease: A Double Blind, Randomized and Placebo-controlled Trial". Journal of Clinical Pharmacy and Therapeutics 28 (1): 53–59. doi:10.1046/j.1365-2710.2003.00463.x. PMID 12605619.
- ↑ Koh, D. C.; Armugam, A.; Jeyaseelan, K. (December 2006). "Snake Venom Components and Their Applications in Biomedicine". Cellular and Molecular Life Sciences 63 (24): 3030–3041. doi:10.1007/s00018-006-6315-0. PMID 17103111.
- ↑ Govindarajan, R.; Vijayakumar, M.; Pushpangadan, P. (June 2005). "Antioxidant Approach to Disease Management and the Role of 'Rasayana' Herbs of Ayurveda". Journal of Ethnopharmacology 99 (2): 165–178. doi:10.1016/j.jep.2005.02.035. PMID 15894123.
- ↑ Subapriya, R.; Nagini, S. (March 2005). "Medicinal Properties of Neem Leaves: A Review". Curr Med Chem Anticancer Agents 5 (2): 1496. doi:10.2174/1568011053174828. PMID 15777222. http://openurl.ingenta.com/content/nlm?genre=article&issn=1568-0118&volume=5&issue=2&spage=149&aulast=Subapriya.
- ↑ 71.0 71.1 Mungantiwar, A. A.; Phadke, A. S. (2003). "Immunomodulation: Therapeutic Strategy through Ayurveda". Scientific Basis for Ayurvedic Therapies. op. cit.. p. 72.
- ↑ 72.0 72.1 Mitra & Rangesh, p. 319
- ↑ 73.0 73.1 Saper, R. B.; Phillips, R. S.; Sehgal, A., et al. (August 2008). "Lead, Mercury, and Arsenic in US- and Indian-manufactured ayurvedic Medicines Sold via the Internet". Journal of the American Medical Association 300 (8): 915–923. doi:10.1001/jama.300.8.915. PMID 18728265.
- ↑ Urmila, T; Supriya, B. (2008). "Pharmacovigilance of Ayurvedic Medicines in India". Indian Journal of Pharmacology 40 (S1): 10–12. http://www.bioline.org.br/request?ph08015.
- ↑ Saper, R. B.; Kales, S. N.; Paquin, J.; et al. (December 2004). "Heavy Metal Content of Ayurveda Herbal Medicine Products". Journal of the American Medical Association 292 (23): 2868–2673. doi:10.1001/jama.292.23.2868. PMID 15598918. http://jama.ama-assn.org/cgi/content/full/292/23/2868.
- ↑ Ellin, Abby (September 17, 2008). "Skin Deep: Ancient, but How Safe?". The New York Times (New York, NY: NYTC). http://www.nytimes.com/2008/09/18/fashion/18skin.html?em=&pagewanted=all. Retrieved September 19, 2008. "A report in the August 27 issue of The Journal of the American Medical Association found that nearly 21 percent of 193 ayurvedic herbal supplements bought online, produced in both India and the United States, contained lead, mercury or arsenic."
- ↑ Szabo, Liz (August 26, 2008). "Study Finds Toxins in Some Herbal Medicines". USA Today (McLean, VA: Gannett Co). http://www.usatoday.com/news/health/2008-08-26-ayurvedic-medicines_N.htm.
- ↑ Thorat, S.; Dahanukar, S. (July 1991). "Can We Dispense with Ayurvedic Samskaras?". Journal of Postgraduate Medicine 37 (3): 157–159. PMID 1784028. http://www.jpgmonline.com/article.asp?issn=0022-3859;year=1991;volume=37;issue=3;spage=157;epage=9;aulast=Thorat.
- ↑ Tillotson, Alan Keith (2001). The One Earth Herbal Sourcebook: Everything You Need to Know About Chinese, Western, and Ayurvedic Herbal Treatments.
- ↑ Valiathan, M. S. (January 10, 2006). "Ayurveda: Putting the House in Order". Current Science (Indian Academy of Sciences) 90 (1): 5–6.
- ↑ Dubey, N. K.; Kumar, R.; Tripathi, P. (January 10, 2004). "Global Promotion of Herbal Medicine: India's Opportunity". Current Science 86 (1): 37–41.
- ↑ Bhushan, Patwardhan; Warude Dnyaneshwar and Tillu Girish (May 25, 2005). "Heavy Metals and Ayurveda". Current Science 88 (10): 1535. http://www.ias.ac.in/currsci/may252005/1535a.pdf.
References
- Chopra, Ananda S. (2003). ""Āyurveda"". In Selin, Helaine. Medicine Across Cultures: History and Practice of Medicine in Non-Western Cultures. Norwell, MA: Kluwer Academic Publishers. pp. 75–83. ISBN 1-4020-1166-0.
- Dwivedi, Girish; Dwivedi, Shridhar (2007). "History of Medicine: Sushruta – the Clinician – Teacher par Excellence". Indian Journal of Chest Diseases and Allied Sciences (Delhi, India: Vallabhbhai Patel Chest Institute, U. of Delhi / National College of Chest Physicians) 49: 243–244. http://medind.nic.in/iae/t07/i4/iaet07i4p243.pdf. (Republished by National Informatics Centre, Government of India.)
- Finger, Stanley (2001). Origins of Neuroscience: A History of Explorations into Brain Function. Oxford, England/New York, NY: Oxford University Press. ISBN 0-19-514694-8.
- Kurup, P. N. V. (2003). "Ayurveda – A Potential Global Medical System". Scientific Basis for Ayurvedic Therapies. op. cit.. in Lakshmi C. Mishra (2004). Scientific basis for Ayurvedic therapies. Boca Raton: CRC. ISBN 0-8493-1366-X.
- Kutumbian, P. (1999). Ancient Indian Medicine. Andhra Pradesh, India: Orient Longman. ISBN 978-81-250-1521-5.
- Lock, Stephen; et al. (2001). The Oxford Illustrated Companion to Medicine. Oxford U. Pr. ISBN 0-19-262950-6.
- Mitra, K. S.; Rangesh, P. R. (2003). "Irritable Colon (Grahni)". Scientific Basis for Ayurvedic Therapies. op. cit..
- Ninivaggi, Frank John (2008). Ayurveda: A Comprehensive Guide to Traditional Indian Medicine for the West. Westport, CT: Praeger Press. ISBN 0-313-34837-5.
- Sharma, H. M.; Bodeker, Gerard C (1997). "Alternative Medicine (medical system)". Encyclopædia Britannica (2008 ed. ed.).
- Underwood, E. Ashworth; Rhodes, P. (2008"title=Medicine, History of). Encyclopædia Britannica (2008 ed. ed.).
- Wujastyk, D. (2003). The Roots of Ayurveda: Selections from Sanskrit Medical Writings. Penguin Books. ISBN 0-14-044824-1.
External links
|
||||||||
|
|||||||||||||||||||||||||
|
|||||