Testosterone
 |
|
 |
|
|
Testosterone
|
|
| Systematic (IUPAC) name | |
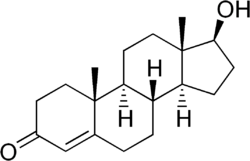
| (8R,9S,10R,13S,14S,17S)- 17-hydroxy-10,13-dimethyl- 1,2,6,7,8,9,11,12,14,15,1
6,17- dodecahydrocyclopenta[a] phenanthren-3-one |
|
| Identifiers | |
| CAS number | |
| ATC code | G03 |
| PubChem | |
| ChemSpider | |
| Chemical data | |
| Formula | C19H28O2 |
| Mol. mass | 288.43 |
| SMILES | & |
| Physical data | |
| Melt. point | 155–156 °C (311–313 °F) |
| Spec. rot | +110,2° |
| SEC Combust | −11080 kJ/mol |
| Pharmacokinetic data | |
| Bioavailability | low (due to extensive first pass metabolism) |
| Metabolism | Liver, Testis and Prostate |
| Half life | 2-4 hours |
| Excretion | Urine (90%), feces (6%) |
| Therapeutic considerations | |
| Pregnancy cat. |
X (USA), Teratogenic effects |
| Legal status |
Schedule III (USA) |
| Routes | Intramuscular injection, transdermal (cream, gel, or patch), sub-'Q' pellet |
Testosterone is a steroid hormone from the androgen group. In mammals, testosterone is primarily secreted in the testes of males and the ovaries of females, although small amounts are also secreted by the adrenal glands. It is the principal male sex hormone and an anabolic steroid.
In both men and women, testosterone plays a key role in health and well-being as well as in sexual functioning. Examples include enhanced libido, increased energy, increased production of red blood cells and protection against osteoporosis. On average, an adult human male body produces about forty to sixty times more testosterone than an adult female body, but females are, from a behavioral perspective (rather than from an anatomical or biological perspective), more sensitive to the hormone.[1] However the overall ranges for male and female are very wide, such that the ranges actually overlap at the low end and high end respectively.
Contents |
History
A testicular action was linked to circulating blood fractions—now understood to be a family of androgenic hormones—in the early work on castration and testicular transplantation in fowl by Arnold Adolph Berthold (1803–1861). Research on the action of testosterone received a brief boost in 1889, when the Harvard professor Charles-Édouard Brown-Séquard (1817–1894), then in Paris, self-injected subcutaneously a “rejuvenating elixir” consisting of an extract of dog and guinea pig testicle. He reported in The Lancet that his vigor and feeling of wellbeing were markedly restored but, predictably, the effects were transient (and likely based on placebo), and Brown-Séquard’s hopes for the compound were dashed. Suffering the ridicule of his colleagues, his work on the mechanisms and effects of androgens in human beings was abandoned by Brown-Séquard and succeeding generations of biochemists for nearly 40 years.
The trail remained cold until the University of Chicago’s Professor of Physiologic Chemistry, Fred C. Koch, established easy access to a large source of bovine testicles—the Chicago stockyards—and to students willing to endure the ceaseless toil of extracting their isolates. In 1927, Koch and his student, Lemuel McGee, derived 20mg of a substance from a supply of 40 pounds of bovine testicles that, when administered to castrated roosters, pigs and rats, remasculinized them.[2] The group of Ernst Laqueur at the University of Amsterdam purified testosterone from bovine testicles in a similar manner in 1934, but isolation of the hormone from animal tissues in amounts permitting serious study in humans was not feasible until three European pharmaceutical giants—Schering (Berlin, Germany), Organon (Oss, Netherlands) and Ciba (Basel, Switzerland)—began full-scale steroid research and development programs in the 1930’s.
The Organon group in the Netherlands were the first to isolate the hormone, identified in a May 1935 paper "On Crystalline Male Hormone from Testicles (Testosterone)" by Karoly Gyula David, E. Dingemanse, J. Freud and Ernst Laqueur. They named the hormone testosterone, from the stems of testicle and sterol, and the suffix of ketone. The structure was worked out by Schering’s Adolf Butenandt (1903–1995).
The chemical synthesis of testosterone was achieved in August that year, when Butenandt and G. Hanisch published a paper describing "A Method for Preparing Testosterone from Cholesterol." Only a week later, the Ciba group in Zurich, Leopold Ruzicka (1887–1976) and A. Wettstein, announced a patent application in a paper "On the Artificial Preparation of the Testicular Hormone Testosterone (Androsten-3-one-17-ol)." These independent partial syntheses of testosterone from a cholesterol base earned both Butenandt and Ruzicka the joint 1939 Nobel Prize in Chemistry.[3] Testosterone was identified as 17β-hydroxandrost-4-en-3-one (C19H28O2), a solid polycyclic alcohol with a hydroxyl group at the 17th carbon atom. This also made it obvious that additional modifications on the synthesized testosterone could be made, i.e., esterification and alkylation.
The partial synthesis in the 1930s of abundant, potent testosterone esters permitted the characterization of the hormone’s effects, so that Kochakian and Murlin (1936) were able to show that testosterone raised nitrogen retention (a mechanism central to anabolism) in the dog, after which Charles Kenyon’s group[4] was able to demonstrate both anabolic and androgenic effects of testosterone propionate in eunuchoidal men, boys, and women. The period of the early 1930s to the 1950s has been called "The Golden Age of Steroid Chemistry",[5] and work during this period progressed quickly. Research in this golden age proved that this newly synthesized compound—testosterone—or rather family of compounds (for many derivatives were developed from 1940 to 1960), was a potent multiplier of muscle, strength, and wellbeing.[6]
Production
Natural

Like other steroid hormones, testosterone is derived from cholesterol. The largest amounts of testosterone are produced by the testes in men. It is also synthesized in far smaller quantities in women by the thecal cells of the ovaries, by the placenta, as well as by the zona reticularis of the adrenal cortex in both sexes.
In the testes, testosterone is produced by the Leydig cells. The male generative glands also contain Sertoli cells which require testosterone for spermatogenesis. Like most hormones, testosterone is supplied to target tissues in the blood where much of it is transported bound to a specific plasma protein, sex hormone binding globulin (SHBG).
Artificial
Testosterone is synthesizable in almost unlimited quantities. Furthermore, there are two possible modifications on it, giving it further abilities. First, it can be esterified, permitting a long-lasting effect when injected into the body. Second, it can be alkylated, permitting oral intake instead of injection.
Esterification
The second importance of the hydroxyl side chain at the C-17 position is that it can not only be esterified, but it can also be alkylated (by Alkylation permits oral steroids, substitution of an ethyl or methyl group for the hydroxyl group). the so-called “17-aa” or alkylated family of androgens such as methyl testosterone, which can be taken up by the digestive tract, and so be easily administered in pill form.
Virilizing and effects on humans
In general, androgens promote protein synthesis and growth of those tissues with androgen receptors. Testosterone effects can be classified as virilizing and anabolic, although the distinction is somewhat artificial, as many of the effects can be considered both.
- Anabolic effects include growth of muscle mass and strength, increased bone density and strength, and stimulation of linear growth and bone maturation.
- Virilizing effects include maturation of the sex organs, particularly the penis and the formation of the scrotum in unborn children, and after birth (usually at puberty) a deepening of the voice, growth of the beard and axillary hair. Many of these fall into the category of male secondary sex characteristics.
Testosterone effects can also be classified by the age of usual occurrence. For postnatal effects in both males and females, these are mostly dependent on the levels and duration of circulating free testosterone.
Prenatal androgen effects
Most of the prenatal androgen effects occur between 7 and 12 weeks of gestation.
- Genital virilization (midline fusion, phallic urethra, scrotal thinning and rugation, phallic enlargement); although the role of testosterone is far smaller than that of Dihydrotestosterone.
- Development of prostate and seminal vesicles
Early infancy androgen effects
Early infancy androgen effects are the least understood. In the first weeks of life for male infants, testosterone levels rise. The levels remain in a pubertal range for a few months, but usually reach the barely detectable levels of childhood by 4-6 months of age. The function of this rise in humans is unknown. It has been speculated that "brain masculinization" is occurring since no significant changes have been identified in other parts of the body.
Pre- Peripubertal effects
Pre- Peripubertal effects are the first visible effects of rising androgen levels at the end of childhood, occuring in both boys and girls.
- Adult-type body odour
- Increased oiliness of skin and hair, acne
- Pubarche (appearance of pubic hair)
- Axillary hair
- Growth spurt, accelerated bone maturation
- Develop hair on upper lip and sideburns.
Pubertal effects
Pubertal effects begin to occur when androgen has been higher than normal adult female levels for months or years. In males these are usual late pubertal effects, and occur in women after prolonged periods of heightened levels of free testosterone in the blood.
- Enlargement of sebaceous glands. This might cause acne.
- Phallic enlargement or clitoromegaly
- Increased libido and frequency of erection or clitoral engorgement
- Pubic hair extends to thighs and up toward umbilicus
- Facial hair (sideburns, beard, moustache)
- Chest hair, periareolar hair, perianal hair
- Subcutaneous fat in face decreases
- Increased muscle strength and mass [7]
- Deepening of voice
- Growth of the Adam's apple
- Growth of spermatogenic tissue in testes, male fertility
- Growth of jaw, brow, chin, nose, and remodeling of facial bone contours
- Shoulders become broader and rib cage expands
- Completion of bone maturation and termination of growth. This occurs indirectly via estradiol metabolites and hence more gradually in men than women.
Adult testosterone effects
Adult testosterone effects are more clearly demonstrable in males than in females, but are likely important to both sexes. Some of these effects may decline as testosterone levels decline in the later decades of adult life.
- Libido and clitoral engorgement/penile erection frequency.
- Mental and physical energy
- The most recent and reliable studies have shown that testosterone does not cause Prostate cancer, but that it can increase the rate of spread of any existing prostate cancer. Recent studies have also shown its importance in maintaining cardiovascular health.
- Increase eumelanin and reduce pheomelanin
Testosterone regulates the population of thromboxane A2 receptors on megakaryocytes and platelets and hence platelet aggregation in humans ( Ajayi and Halushka 2005, Ajayi et al 1995)[8,9].
Effects on the brain
As testosterone affects the entire body (often by enlarging; men have bigger hearts, lungs, liver, etc.), the brain is also affected by this "sexual" advancement; the enzyme aromatase converts testosterone into estradiol that is responsible for masculinization of the brain in a male fetus.
There are some differences in a male and female brain (the result of different testosterone levels). A clear difference is the size: the male human brain is, on average, larger; however, in females (who generally do not have as high testosterone levels) the corpus callosum is proportionally larger. This means that the effect of testosterone is a greater overall brain volume, but a decreased connection between the hemispheres.[8]
A study conducted in 1996 found no effects on mood or behavior from the administration of supraphysiologic doses of testosterone for 10 weeks to healthy men.[9]
The literature suggests that attention, memory, and spatial ability are key cognitive functions affected by testosterone in humans, though the literature is rather sparse. Preliminary evidence suggests that low testosterone levels may be a risk factor for cognitive decline and possibly for dementia of the Alzheimer’s type,[10] a key argument in Life Extension Medicine for the use of testosterone in anti-aging therapies. Much of the literature, however, suggests a curvilinear or even quadratic relationship between spatial performance and circulating testosterone,[11] where both hypo- and hypersecretion of circulating androgens have negative effects on cognition and cognitively-modulated aggressivity, as detailed above.
Contrary to what has been postulated in outdated studies and by certain sections of the media, aggressive behaviour is not typically seen in hypergonadal men who have their testosterone replaced adequately to the eugonadal/normal range. In fact aggressive behaviour has been associated with hypogonadism and low testosterone levels and it would seem as though supraphysiological and low levels of testosterone and hypogonadism cause mood disorders and aggressive behaviour, with eugondal/normal testosterone levels being important for mental well-being. Testosterone depletion is a normal consequence of aging in men. One consequence of this is an increased risk for the development of Alzheimer’s Disease (Pike et al, 2006, Rosario 2004).
Mechanism
The effects of testosterone in humans and other vertebrates occur by way of two main mechanisms: by activation of the androgen receptor (directly or as DHT), and by conversion to estradiol and activation of certain estrogen receptors.
Free testosterone (T) is transported into the cytoplasm of target tissue cells, where it can bind to the androgen receptor, or can be reduced to 5α-dihydrotestosterone (DHT) by the cytoplasmic enzyme 5-alpha reductase. DHT binds to the same androgen receptor even more strongly than T, so that its androgenic potency is about 2.5 times that of T. The T-receptor or DHT-receptor complex undergoes a structural change that allows it to move into the cell nucleus and bind directly to specific nucleotide sequences of the chromosomal DNA. The areas of binding are called hormone response elements (HREs), and influence transcriptional activity of certain genes, producing the androgen effects. It is important to note that if there is a 5-alpha reductase deficiency, the body (of a human) will continue growing into a female with testicles.
Androgen receptors occur in many different vertebrate body system tissues, and both males and females respond similarly to similar levels. Greatly differing amounts of testosterone prenatally, at puberty, and throughout life account for a share of biological differences between males and females.
The bones and the brain are two important tissues in humans where the primary effect of testosterone is by way of aromatization to estradiol. In the bones, estradiol accelerates maturation of cartilage into bone, leading to closure of the epiphyses and conclusion of growth. In the central nervous system, testosterone is aromatized to estradiol. Estradiol rather than testosterone serves as the most important feedback signal to the hypothalamus (especially affecting LH secretion). In many mammals, prenatal or perinatal "masculinization" of the sexually dimorphic areas of the brain by estradiol derived from testosterone programs later male sexual behavior.
The human hormone testosterone is produced in greater amounts by males, and less by females. The human hormone estrogen is produced in greater amounts by females, and less by males. Testosterone causes the appearance of masculine traits (i.e., deepening voice, pubic and facial hairs, muscular build, etc.) Like men, women rely on testosterone to maintain libido, bone density and muscle mass throughout their lives. In men, inappropriately high levels of estrogens lower testosterone, decrease muscle mass, stunt growth in teenagers, introduce gynecomastia, increase feminine characteristics, and decrease susceptibility to prostate cancer, reduces libido and causes erectile dysfunction and can cause excessive sweating and hot flushes. However, an appropriate amount of estrogens is required in the male in order to ensure well-being, bone density, libido, erectile function, etc.
Therapeutic use
Routes of administration
There are many routes of administration for testosterone. Forms of testosterone for human administration currently available include injectable (such as testosterone cypionate or testosterone enanthate in oil), oral,[12] buccal,[13] transdermal skin patches, and transdermal creams or gels.[14] In the pipeline are "roll on" methods and nasal sprays.
Indications
The original and primary use of testosterone is for the treatment of males who have too little or no natural endogenous testosterone production—males with hypogonadism. Appropriate use for this purpose is legitimate hormone replacement therapy (testosterone replacement therapy (TRT)), which maintains serum testosterone levels in the normal range.
However, over the years, as with every hormone, testosterone or other anabolic steroids has also been given for many other conditions and purposes besides replacement, with variable success but higher rates of side effects or problems. Examples include infertility, lack of libido or erectile dysfunction, osteoporosis, penile enlargement, height growth, bone marrow stimulation and reversal of anemia, and even appetite stimulation. By the late 1940s testosterone was being touted as an anti-aging wonder drug (e.g., see Paul de Kruif's The Male Hormone). Decline of testosterone production with age has led to a demand for Androgen Replacement Therapy.
To take advantage of its virilizing effects, testosterone is often administered to transmen as part of the hormone replacement therapy, with a "target level" of the normal male testosterone level. Like-wise, transwomen are sometimes prescribed anti-androgens to decrease the level of testosterone in the body and allow for the effects of estrogen to develop.
Testosterone patches are effective at treating low libido in post-menopausal women.[15] Low libido may also occur as a symptom or outcome of hormonal contraceptive use. Women may also use testosterone therapies to treat or prevent loss of bone density, muscle mass and to treat certain kinds of depression and low energy state. Women on testosterone therapies may experience an increase in weight without an increase in body fat due to changes in bone and muscle density. Most undesired effects of testosterone therapy in women may be controlled by hair-reduction strategies, acne prevention, etc. There is a theoretical risk that testosterone therapy may increase the risk of breast or gynaecological cancers, and further research is needed to allay these fears.[15]
There is a myth that exogenous testosterone can more or less definitively be used for male birth control. However, the vast majority of physicians will agree that to prescribe exogenous testosterone for this purpose is inappropriate. But, perhaps more important, many men found this, in first-hand experience, to be untrue or at least, unreliable.
Other drugs
Some drugs specifically target testosterone as a way of treating certain conditions. For example, finasteride inhibits the conversion of testosterone into dihydrotestosterone (DHT), a metabolite which is more potent than testosterone. By lowering the levels of dihydrotestosterone, finasteride may be used for various conditions associated with androgens, such as benign prostatic hyperplasia (BPH) and androgenetic alopecia (male-pattern baldness). That said there are many men who have complained of long lasting or permanent adverse effects resulting from the use of finasteride and Dr Eugene Shippen has spoken for many years of finasteride causing a difficult to treat form of hypogonadism in some men.).
Adverse effects
Exogenous testosterone supplementation comes with a number of health risks. Fluoxymesterone and methyltestosterone are synthetic derivatives of testosterone. In 2006 it was reported that women taking Estratest, a combination pill including estrogen and methyltestosterone, were at considerably heightened risk of breast cancer. That said methyltestosterone and Fluoxymesterone are no longer prescribed by physicians given their poor safety record, and testosterone replacement in men does have a very good safety record as evidenced by over sixty years of medical use in hypogonadal men.
One adverse effect that many men complain of is that of the development of gynecomastia (breasts), but this is something that can be prevented by appropriate choice and dosing of medication, and, in required cases, the use of ancillary medications that help lower SHBG or estradiol. Another side-effect is having difficulty urinating.
Athletic use
Testosterone may be administered to an athlete in order to improve performance, and is considered to be a form of doping in most sports. There are several application methods for testosterone, including intramuscular injections, transdermal gels and patches, and implantable pellets.
Anabolic steroids (of which testosterone is one) have also been taken to enhance muscle development, strength, or endurance. They do so directly by increasing the muscles' protein synthesis. As a result, muscle fibers become larger and repair faster than the average person's. After a series of scandals and publicity in the 1980s (such as Ben Johnson's improved performance at the 1988 Summer Olympics), prohibitions of anabolic steroid use were renewed or strengthened by many sports organizations. Testosterone and other anabolic steroids were designated a "controlled substance" by the United States Congress in 1990, with the Anabolic Steroid Control Act.[16] The levels of testosterone abused in sport greatly exceed the quantities of the steroid that are prescribed for medical use in hypogonadism. It is the supraphysiological doses and ultra high levels of testosterone that bring with it many undesirable effects and potential long term adverse health effects. Coupled with the nature of cheating in sport, this is seen as being a seriously problematic issue in modern sport, particularly given the lengths to which athletes and professional laboratories go to in trying to conceal such abuse from sports regulators. Steroid abuse once again came into the spotlight recently as a result of the Chris Benoit double murder-suicide in 2007, and the media frenzy surrounding it - however, there has been no evidence indicating steroid use as a contributing factor.
Changes during aging
Testosterone levels decline gradually with age in human beings. The clinical significance of this decrease is debated (see andropause). There is disagreement about if and when to treat aging men with testosterone replacement therapy. The American Society of Andrology's position is that testosterone therapy "is indicated when both clinical symptoms and signs suggestive of androgen deficiency and decreased testosterone levels are present". The American Association of Clinical Endocrinologists says "Hypogonadism is defined as a free testosterone level that is below the lower limit of normal for young adult control subjects. Previously, age-related decreases in free testosterone were once accepted as normal. Currently, they are not considered normal....Patients with low-normal to subnormal range testosterone levels warrant a clinical trial of testosterone."[17]
There isn't total agreement on the threshold of testosterone value below which a man would be considered hypogonadal. (Currently there are no standards as to when to treat women.) Testosterone can be measured as "free" (that is, bioavailable and unbound) or more commonly, "total" (including the percentage which is chemically bound and unavailable). In the United States, male total testosterone levels below 300 to 400 ng/dl from a morning sample
are generally considered low. However these numbers are typically not age-adjusted, but based on an average of a test group which includes elderly males with low testosterone levels. Therefore a value of 300 ng/dl might be normal for a 65-year-old male, but not normal for a 30-year-old. Identification of inadequate testosterone in an aging male by symptoms alone can be difficult. The signs and symptoms are non-specific, and might be confused with normal aging characteristics, such as loss of muscle mass and bone density, decreased physical endurance, decreased memory ability and loss of libido.
Replacement therapy can take the form of injectable depots, transdermal patches and gels, subcutaneous pellets and oral therapy. Adverse effects of testosterone supplementation include minor side effects such as acne and oily skin, and more significant complications such as increased hematocrit which can require venipuncture in order to treat, exacerbation of sleep apnea and acceleration of pre-existing prostate cancer growth. Exogenous testosterone also causes suppression of spermatogenesis and can lead to infertility.[18] It is recommended that physicians screen for prostate cancer with a digital rectal exam and PSA (prostate specific antigen) level prior to initiating therapy, and monitor hematocrit and PSA levels closely during therapy.
Benefits
Appropriate testosterone therapy can prevent or reduce the likelihood of osteoporosis, type 2 diabetes, cardio-vascular disease (CVD), obesity, depression and anxiety and the statistical risk of early mortality. Low testosterone also brings with it an increased risk for the development of Alzheimer’s Disease (Pike et al, 2006, Rosario 2004).
A small trial in 2005 showed mixed results.[19]
Large scale trials to assess the efficiency and long-term safety of testosterone are still lacking.[20]
See also
- Male
- Testosterone poisoning
- Testosterone spray
Notes
- ↑ James McBride Dabbs, 2000
- ↑ Gallagher and Koch, 1929.
- ↑ Hoberman and Yesalis 1995, Freeman et al. 2001.
- ↑ Kenyon et al. 1940.
- ↑ Schwarz et al. 1999.
- ↑ deKruif, 1945.
- ↑ Bhasin S, Storer TW, Berman N, et al
- ↑ Solms and Turnbull 2002.
- ↑ Bhasin S, Storer TW, Berman N, et al
- ↑ e.g., Moffat et al, 2005; Hogervorst et al 2005.
- ↑ e.g., Moffat and Hampson, 1996.
- ↑ "Andriol". Food and Drug Administration.
- ↑ "Striant". Food and Drug Administration.
- ↑ "Androgel". Food and Drug Administration. and "Testim". Food and Drug Administration.
- ↑ 15.0 15.1 Davis SR, Moreau M, Kroll R, et al. (2008). "Testosterone for low libido in postmenopausal women not taking estrogen". N Engl J Med 359 (19): 2005–2017. http://content.nejm.org/cgi/content/short/359/19/2005?query=TOC.
- ↑ "Anabolic Steroid Control Act". United States Sentencing Commission (1990).
- ↑ "Medical guidelines for clinical practice for the evaluation and treatment of male sexual dysfunction". American association of clinical endocrinologists.
- ↑ World Health Organisation (1990), The Lancet.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/18167405 "Effect of testosterone supplementation on functional mobility, cognition, and other parameters in older men: a randomized controlled trial."
- ↑ http://www.endocrinetoday.com/view.aspx?rid=29171 "Testosterone treatment in aging men"
References
- Ajayi AAL, Mathur R, Halushka PV. Testosterone increases platelet TXA2 receptor density and aggregation responses (1995). Circulation 91 : 2742-7.
- Ajayi AAL, Halushka PV. Castration reduces platelet TXA2 receptor density and aggregability (2005). QJM 98 : 349-57.
- Bhasin S, Storer TW, Berman N, et al (1996). "The effects of supraphysiologic doses of testosterone on muscle size and strength in normal men". N. Engl. J. Med. 335 (1): 1–7. doi:. PMID 8637535.
- E.R. Freeman, D.A. Bloom, and E.J. McGuire (2001). "A brief history of testosterone". Journal of Urology 165: 371–373. doi:. PMID 11176375.
- J.M. Hoberman and C.E. Yesalis (1995). "The history of synthetic testosterone". Scientific American 272: 76–81. PMID 7817189.
- P.R. Larsen et al. (2003). Williams textbook of endocrinology (10th edition ed.). Saunders. ISBN 978-0-7216-9184-8. OCLC 48942603 50841393. (Seventh edition by J.D. Wilson and R.H. Williams, 1985, ISBN 072161082X.)
- S.D. Moffat and E. Hampson (1996). "A curvilinear relationship between testosterone and spatial cognition in humans: Possible influence of hand preference". Psychoneuroendocrinology 21 (3): 323–337. doi:.
- S.D. Moffat, A.B. Zonderman, E.J. Metter et al. (2004). "Free testosterone and risk for Alzheimer's disease in older men". Neurology 62: 188–193.
- M. Parssinen, U. Kujala, E. Vartiainen, et al. (2000). "Increased premature mortality of competitive powerlifters suspected to have used anabolic agents". International Journal of Sports Medicine 21: 225–227. doi:.
- S. Schwarz, D. Onken, and A. Schubert (1999). "The steroid story of Jenapharm: From the late 1940s to the early 1970s". Steroids 64: 439–445. doi:. http://www.ingentaconnect.com/content/els/0039128x/1999/00000064/00000007/art00003.
- M. Solms and O. Turnbull (2002). The brain and the inner world. Other Press, New York. ISBN 978-1590510179. OCLC 48761737 59373319.
- World Health Organization Task Force on methods for the regulation of male fertility (1990). "Contraceptive efficacy of testosterone-induced azoospermia in normal men". Lancet 336: 955–959. doi:. PMID 1977002.
External links
- NIST entry for Testosterone
- NIST results of search for Testosterone (Shows androstenone.)
- Results of research on the efficacy of differing body locations for the absorption of topical testosterone creams
- "Calls for testosterone trials in CHD "
|
|||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||