Phencyclidine
 |
|
 |
|
|
Phencyclidine
|
|
| Systematic (IUPAC) name | |
| 1-(1-phenylcyclohexyl)piperidine | |
| Identifiers | |
| CAS number | |
| ATC code | ? |
| PubChem | |
| ChemSpider | |
| Chemical data | |
| Formula | C17H25N |
| Mol. mass | 243.387 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | 7-46 hours |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Schedule II / Class A |
| Routes | Smoked, Insufflate, Oral |
Phencyclidine (a complex clip of the chemical name phenylcyclohexylpiperidine, commonly initialised as PCP), is a dissociative drug formerly used as an anesthetic agent, exhibiting hallucinogenic and neurotoxic effects.[1] It was first patented in 1952 by the Parke-Davis pharmaceutical company and marketed under the brand name Sernyl. PCP is listed as a Schedule II drug in the United States under the Convention on Psychotropic Substances.[2]
In chemical structure, PCP is an arylcyclohexylamine derivative, and, in pharmacology, it is a member of the family of dissociative anesthetics. PCP works primarily as an NMDA receptor antagonist, which blocks the activity of the NMDA Receptor.[3] Other NMDA receptor antagonists include ketamine, tiletamine, and dextromethorphan. Although the primary psychoactive effects of the drug last only hours, total elimination from the body is prolonged, typically extending over weeks.
Contents |
Biochemistry and pharmacology
Biochemical action
The N-methyl-D-Aspartate (NMDA) receptor, a type of ionotropic receptor, is found on the dendrites of neurons and receives signals in the form of neurotransmitters. It is a major excitatory receptor in the brain. Normal physiological function requires that the activated receptor fluxes positive ions through the channel part of the receptor. PCP enters the ion channel from the outside of the neuron and binds, reversibly, to a site in the channel pore, blocking the flux of positive ions into the cell. PCP therefore inhibits depolarization of neurons and interferes with cognitive and other functions of the nervous system.
In a similar manner, PCP and analogues also inhibit nicotinic acetylcholine receptor channels (nAChR). Some analogues have greater potency at nAChR than at NMDAR. In some brain regions, these effects act synergistically to inhibit excitatory activity.
PCP is retained in fatty tissue and is broken down by the human metabolism into PCHP, PPC and PCAA.
The most troubling clinical effects are likely produced by the indirect action of phencyclidine on the presynaptic dopamine receptor (DA-2). This has been suggested to account for most of the psychotic features. [4] The relative immunity to pain is likely produced by indirect interaction with the endogenous endorphin and enkephalin system in rats. [5]
Structural analogs

More than 30 different analogues of PCP were reported as being used on the street during the 1970s and 1980s, mainly in the USA. The best known of these are PCPy (rolicyclidine, 1-(1-phenylcyclohexyl)pyrrolidine); PCE (eticyclidine, N-ethyl-1-phenylcyclohexylamine); and TCP (tenocyclidine, 1-(1-(2-Thienyl)cyclohexyl)piperidine). These compounds were never widely-used and did not seem to be as well-accepted by users as PCP itself, however they were all added onto Schedule I of the Controlled Substance Act because of their putative similar effects.[6]
The generalized structural motif required for PCP-like activity is derived from structure-activity relationship studies of PCP analogues, and summarized below. All of these analogues would have somewhat similar effects to PCP itself, although, with a range of potencies and varying mixtures of anesthetic, dissociative and stimulant effects depending on the particular substituents used. In some countries such as the USA, Australia, and New Zealand, all of these compounds would be considered controlled substance analogues of PCP, and are hence illegal drugs, even though many of them have never been made or tested.[7][8]
Brain effects
Like other NMDA receptor antagonists, it is postulated that phencyclidine can cause a certain kind of brain damage called Olney's Lesions.[9][10] Studies conducted on rats showed that high doses of the NMDA receptor antagonist MK-801 caused irreversible vacuoles to form in certain regions of the rats' brains, and experts say that it is possible that similar brain damage can occur in humans. All studies of Olney's Lesions were performed only on other animals and may not apply to humans. Critics have cited poorly-performed studies and differences in animal metabolism to suggest that Olney's Lesions may not occur in humans.[11][12]
Phencyclidine has also been shown to cause schizophrenia-like changes in the rat brain, which are detectable both in living rats and upon post-mortem examination of brain tissue.[13] It also induces symptoms in humans that are virtually indistinguishable from schizophrenia.[14]
History and medicinal use
PCP was first tested after World War II as a surgical anesthetic. Because of its adverse side-effects, such as hallucinations, mania, delirium, and disorientation, it was shelved until the 1950s. In 1963, it was patented by Parke-Davis and named Sernyl (referring to serenity), but was withdrawn from the market two years later because of side-effects. It was renamed Sernylan in 1967, and marketed as a veterinary anesthetic, but again discontinued. Its side-effects and long half-life in the human body made it unsuitable for medical applications.
When smoked, some of it is broken down by heat into 1-phenyl-1-cyclohexene (PC) and piperidine.

Recreational use
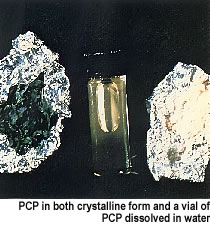
PCP is consumed recreationally. It comes in both powder and liquid forms (PCP base is dissolved most often in ether), but typically it is sprayed onto leafy material such as marijuana, mint, oregano, parsley, or ginger leaves, then smoked. Common street names for the drug vary from locale to locale, but include "angel dust", "illy", "wet", "BrainTree", "fry", "shit", "dumb dust", "cannibonal", "rocket fuel", "cake,", "nature boy", "love boat", "cornbread", "Hairy Jerry", "supergrass" (when combined with marijuana), "Water", "Sherman Hemsley" (from the street name "sherm"), "George Jefferson", and "leak". In Quebec it is known as "paste".
PCP is a Schedule II substance in the United States, a List II drug of the Opium Law in the Netherlands and a Class A substance in the United Kingdom.
Method of absorption
The term "embalming fluid" is often used to refer to the liquid PCP in which a cigarette or joint is dipped (a "sherm", "dipper" or "dippy"), to be ingested through smoking. Smoking PCP is known as "getting wet." There is much confusion over the practice of dipping cigarettes in "embalming fluid" leading some to think that real embalming fluid may actually be used. Smoking actual formaldehyde will cause intoxication, and may cause serious health consequences beyond those of consuming PCP, due to the toxicity of formaldehyde and other embalming chemicals. The slang term "embalming fluid" likely originated from PCP's somatic "numbing" effect and the feeling of physical dissociation from the body.
In its powder form, PCP can be insufflated.
In Canada, particularly in the provinces of Quebec and New Brunswick, PCP is mostly encountered as "mescaline" (often locally called "mess" or "mesc"), although most local users are aware that the drug is not, in fact, mescaline, but is actually a mixture of quinine or lactose and PCP freebase (chemistry). The most common form of ingesting PCP is through smoking; however, the drug may also be insufflated.
In its pure form, PCP is a white crystalline powder that readily dissolves in water. However, most PCP on the illicit market contains a number of contaminants as a result of makeshift manufacturing, causing the color to range from tan to brown, and the consistency to range from powder to a gummy mass.
Effects
Behavioral effects can vary by dosage. Small doses produce a numbness in the extremities and intoxication, characterized by staggering, unsteady gait, slurred speech, bloodshot eyes, and loss of balance. Moderate doses (5-10 mg intranasal, or 0.01-0.02 mg/kg intramuscular or intravenous), will produce analgesia and anesthesia. High doses may lead to convulsions.[15]
Psychological effects include severe changes in body image, loss of ego boundaries, and depersonalization. Visual hallucinations and euphoria are reported infrequently.[15]
The drug has been known to alter mood states in an unpredictable fashion, causing some individuals to become detached, and others to become animated. Intoxicated individuals may act in an unpredictable fashion, driven by their delusions and hallucinations. Included in the portfolio of behavioral disturbances are acts of self-injury including suicide, and attacks on others or destruction of property. The analgesic properties of the drug can cause users to feel less pain, and persist in violent or injurious acts as a result. Recreational doses of the drug can also induce a psychotic state that resembles schizophrenic episodes which can last for months at a time with toxic doses. However, users generally report an "outer body" experience where they feel detatched from reality, or one's consciousness seems somewhat disconnected from normal reality. Symptoms can be easily recalled by the mnemonic device "RED DANES": rage, erythema (redness of skin), dilated pupils, delusions, amnesia, nystagmus (oscillation of the eyeball when moving laterally), excitation, and skin dry.[16]
Management of intoxication
Management of phencyclidine intoxication mostly consists of supportive care—controlling breathing, circulation, and body temperature—and, in the early stages, treating psychiatric symptoms.[17][18][19] Benzodiazepines, such as lorazepam, are the drugs of choice to control agitation and seizures (when present). Typical antipsychotics such as phenothiazines and haloperidol have been used to control psychotic symptoms, but may produce many undesirable side effects—such as dystonia—and their use is therefore no longer preferred; phenothiazines are particularly risky, as they may lower the seizure threshold, worsen hyperthermia, and boost the anticholinergic effects of PCP.[17][18] If an antipsychotic is given, intramuscular haloperidol has been recommended.[19][20][21]
Forced acid diuresis (with ammonium chloride or, more safely, ascorbic acid) may increase clearance of PCP from the body, and was somewhat controversially recommended in the past as a decontamination measure.[17][18][19] However, it is now known that only around 10% of a dose of PCP is removed by the kidneys, which would make increased urinary clearance of little consequence; furthermore, urinary acidification is dangerous, as it may induce acidosis and worsen rhabdomyolysis (muscle breakdown), which is not an unusual manifestation of PCP toxicity.[17][18]
References
- ↑ Maisto, Stephen A.; Mark Galizio, Gerard Joseph Connors (2004). Drug Use and Abuse. Thompson Wadsworth. ISBN 0155085174.
- ↑ "List of psychotropic substances under control, in accordance with the Convention on Psychotropic Substances of 1971": Report from 2003 (pdf)
- ↑ Kapur, S. and P. Seeman. "NMDA receptor antagonists ketamine and PCP have direct effects on the dopamine D2 and serotonin 5-HT2receptors¾implications for models of schizophrenia" Molecular Psychiatry. 7(8): 837–844 (2002)
- ↑ Giannini AJ, Nageotte C, Loiselle RH, Malone DA, Price WA (1984). "Comparison of chlorpromazine, haloperidol and pimozide in the treatment of phencyclidine psychosis: DA-2 receptor specificity". Journal of Toxicology. Clinical Toxicology 22 (6): 573–9. PMID 6535849.
- ↑ Castellani S, Giannini AJ, Adams PM (1982). "Effects of naloxone, metenkephalin, and morphine on phencyclidine-induced behavior in the rat". Psychopharmacology 78 (1): 76–80. PMID 6815700.
- ↑ PCP synthesis and effects: table of contents
- ↑ Itzhak Y, Kalir A, Weissman BA, Cohen S. New analgesic drugs derived from phencyclidine. Journal of Medicinal Chemistry. 1981; 24(5):496–499
- ↑ Chaudieu I, Vignon J, Chicheportiche M, Kamenka JM, Trouiller G, Chicheportiche R. Role of the aromatic group in the inhibition of phencyclidine binding and dopamine uptake by PCP analogs. Pharmacology Biochemistry and Behaviour. 1989 Mar;32(3):699–705.
- ↑ Olney J, Labruyere J, Price M (1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science 244 (4910): 1360–2. doi:. PMID 2660263.
- ↑ Hargreaves R, Hill R, Iversen L. "Neuroprotective NMDA antagonists: the controversy over their potential for adverse effects on cortical neuronal morphology". Acta Neurochir Suppl (Wien) 60: 15–9. PMID 7976530.
- ↑ Jansen, Karl. Ketamine: Dreams and Realities. MAPS, 2004. ISBN 0966001974
- ↑ Erowid DXM Vault : Response to "The Bad News Isn't In": Please Pass The Crow, by William E. White
- ↑ Reynolds, Lindsay M.; Susan M. Cochran, Brian J. Morris, Judith A. Pratt and Gavin P. Reynolds (March 1, 2005). "Chronic phencyclidine administration induces schizophrenia-like changes in N-acetylaspartate and N-acetylaspartylglutamate in rat brain". Schizophrenia Research 73 (2-3): 147–152. doi:. PMID 15653257. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?itool=pubmed_AbstractPlus&cmd=Retrieve&db=pubmed&list_uids=15653257&dopt=ExternalLink. Retrieved on 2006-09-29.
- ↑ Murray JB (May 2002). "Phencyclidine (PCP): a dangerous drug, but useful in schizophrenia research". J Psychol 136 (3): 319–27. PMID 12206280.
- ↑ 15.0 15.1 Diaz, Jaime. How Drugs Influence Behavior. Englewood Cliffs: Prentice Hall, 1996.
- ↑ AJ Giannini. Drugs of Abuse--Second Edition. Los Angeles, Practice Management Information Corp.,1997,pg. 126. ISBN 1-57066-053-0.
- ↑ 17.0 17.1 17.2 17.3 Helman RS, Habal R (October 6, 2008). "Phencyclidine Toxicity". eMedicine. Retrieved on November 3, 2008.
- ↑ 18.0 18.1 18.2 18.3 Olmedo R (2002). "Chapter 69: Phencyclidine and ketamine". in Goldfrank LR, Flomenbaum NE, Lewin NA, Howland MA, Hoffman RS, Nelson LS (eds.). Goldfrank's Toxicologic Emergencies. New York: McGraw-Hill. pp. 1034–41. ISBN 0-07-136001-8. http://books.google.com/books?id=HVYyRsuUEc0C&pg=PA1041. Retrieved on November 3, 2008 through Google Book Search.
- ↑ 19.0 19.1 19.2 Milhorn HT (April 1991). "Diagnosis and management of phencyclidine intoxication". American Family Physician 43 (4): 1293–302. PMID 2008817.
- ↑ Giannini AJ. Price WA. PCP: Management of acute intoxication. Medical Times. 1985;113(9):43-49
- ↑ Giannini AJ, Eighan MS, Loiselle RH, Giannini MC (April 1984). "Comparison of haloperidol and chlorpromazine in the treatment of phencyclidine psychosis". Journal of Clinical Pharmacology 24 (4): 202–4. PMID 6725621. http://jcp.sagepub.com/cgi/pmidlookup?view=long&pmid=6725621.
See also
- Dissociatives
- Ketamine
- Rolicyclidine
- Eticyclidine
- Tenocyclidine
- Nitrous oxide
- Dextromethorphan
- Psychoactive drug
External links
- Erowid.org - PCP Information
- National Institute of Drug Abuse InfoFacts: PCP (Phencyclidine)
- Drugs and Human Performance Fact Sheets on Phencyclidine
- A site with information on PCP, Partnership for a Drug-Free America
|
|||||||||||
|
||||||||||||||||||||||||