Oxygen toxicity
| Oxygen toxicity Classification and external resources |
|
 |
|
|---|---|
| Paul Bert first described oxygen toxicity in 1878 | |
| ICD-10 | T59.8 |
| ICD-9 | 987.8 |
| MeSH | D018496 |
Oxygen toxicity is a condition resulting from the harmful effects of breathing molecular oxygen (O2) at elevated partial pressures. It is also known as oxygen toxicity syndrome, oxygen intoxication, hyperoxia, or the Paul Bert effect and Lorrain Smith effect, after the researchers who pioneered its discovery and description in the late 19th century. Severe oxygen toxicity can result in cell damage and death, and its effects are most often observed as damage to the central nervous system, lungs and eye. Oxygen toxicity is a concern for scuba divers, premature babies on supplemental oxygen, and astronauts.
The result of breathing elevated concentrations of oxygen is hyperoxia, an excess of oxygen in body tissues. Central nervous system toxicity is caused by short exposure to high concentrations of oxygen at greater than atmospheric pressure. Pulmonary and ocular toxicity result from longer exposure to elevated oxygen levels at normal pressure. Serious incidents can cause oxidation damage to cell membranes, collapse of the alveoli in lungs, myopia, retinal detachment, and seizures. Symptoms include disorientation, breathing difficulty and vision changes. Treatment is by reducing the exposure to elevated oxygen levels and studies show that the long term recovery from most types of oxygen toxicity is good.
Prevention of oxygen toxicity is an important precaution whenever oxygen is breathed at greater than normal partial pressures, and has led to use of protocols for avoidance of hyperoxia in such fields as diving, hyperbaric therapy, neonatal care and human spaceflight. This has resulted in oxygen toxicity seizures becoming increasingly rare, with pulmonary and ocular damage being mainly confined to the problems of managing premature infants.
Contents |
Classification

The effects of oxygen toxicity are commonly classified by the organs affected.
There are three principal types of oxygen toxicity:[1][2][3]
- Central nervous system (CNS), characterised by convulsions followed by unconsciousness, occurring under hyperbaric conditions;
- Pulmonary (lungs), characterised by difficulty in breathing and pain within the chest, occurring when breathing elevated pressures of oxygen for extended periods;
- Ocular (retinopathic conditions), characterised by alterations to the eye, occurring when breathing elevated pressures of oxygen for extended periods.
Central nervous system oxygen toxicity can cause a seizure, a brief period of rigidity followed by convulsions and unconsciousness, and is of concern to divers who encounter greater than atmospheric pressures. Pulmonary oxygen toxicity results in damage to the lungs, causing pain and difficulty in breathing. Oxidative damage to the eye may lead to myopia or partial detachment of the retina. Pulmonary and ocular damage are most likely to occur when supplemental oxygen is administered as part of a treatment, particularly to newborn infants, but are also a concern during hyperbaric oxygen therapy (HBOT).
Oxidative damage may occur in any cell in the body but the effects on the three most susceptible organs will be the primary concern. It may also be implicated in red blood cell destruction (hemolysis),[4][5] liver (hepatic) effects,[6] heart (myocardial) damage,[7] endocrine effects (adrenal, gonads, and thyroid),[8][9][10] kidney (renal) damage,[11] and general damage to cells.[1][12]
In unusual circumstances, effects on other tissues may be observed: it is suspected that during spaceflight, high oxygen concentrations may contribute to bone damage.[13] Hyperoxia can also indirectly cause carbon dioxide narcosis in patients with chronic obstructive pulmonary disease (COPD).[13] Oxygen toxicity is not associated with hyperventilation, because breathing air at atmospheric pressure always has a partial pressure of oxygen (ppO2) of 0.21 bar (21 kPa) and the lower limit for toxicity is more than 0.3 bar (30 kPa).[14]
Signs and symptoms

Central nervous system (CNS) oxygen toxicity manifests as symptoms such as visual changes (especially tunnel vision), ringing in the ears (tinnitus), nausea, twitching (especially on the face), irritability (personality changes, anxiety, confusion, etc.), and dizziness. This may be followed by a tonic-clonic seizure where intense muscle contraction occurs for several seconds followed by rapid spasms of alternate muscle relaxation and contraction producing convulsive jerking, which is followed by a period of unconsciousness (the postictal state).[1][15] The onset depends upon partial pressure of oxygen (ppO2) in the breathing gas and exposure duration but experiments have shown that there is a wide variation in exposure time before onset amongst individuals and in the same individual from day to day.[1][15][16] In addition, many external factors, such as underwater immersion, exposure to cold, and exercise will decrease the time to onset of CNS symptoms.[17][18] Decrease of tolerance has been shown to be closely linked to retention of carbon dioxide.[19][20][21] Other factors, such as darkness and caffeine increase tolerance in test animals, but these effects have not been proven in humans.[22][23]
Pulmonary toxicity symptoms result from an inflammation of the airways leading to and within the lungs (tracheobronchitis) which appears in the upper chest region (substernal and carinal) and spreads to the remaining area of the lungs (tracheobronchial tree).[1][24][25] This begins as a mild tickle on inhalation and progresses into frequent coughing.[1] If oxygen breathing is not discontinued, patients will have a mild burning on inhalation along with uncontrollable coughing and occasional shortness of breath (dyspnea).[1] Physical findings related to pulmonary toxicity have included bubbling sounds heard through a stethoscope (bubbling rales), fever, and increased blood flow to the lining of the nose (hyperemia of the nasal mucosa).[25] The radiological finding from the lungs show inflammation and swelling (pulmonary edema).[1][15][24] Pulmonary function measurements are reduced as noted by the reduction in vital capacity and change in expiratory function and lung elasticity.[1][25] Tests in animals have indicated a variation in tolerance similar to that found in CNS toxicity, as well as significant variations between species. When the exposure to oxygen above 0.5 bar (50 kPa) is intermittent, it permits the lungs to recover and delays the onset of toxicity.[26]
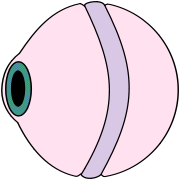
The signs of retinopathy of prematurity (ROP) are observed (via an opthalmoscope) as a demarcation between the vascularised and non-vascularised regions of an infant's retina. The degree of this demarcation is used to designate four stages: (I) the demarcation is a line; (II) the demarcation becomes a ridge; (III) growth of new blood vessels occurs around the ridge; (IV) the retina begins to detach from the inner wall of the eye (choroid).[27]
Causes
CNS toxicity
- See also: Maximum operating depth
Short exposures (from minutes to a few hours) to partial pressure of oxygen above 1.6 bars (160 kPa) (about 8 times the atmospheric concentration) are usually associated with central nervous system (CNS) oxygen toxicity and are most likely to occur among patients undergoing hyperbaric oxygen therapy (HBOT) and divers. Since atmospheric pressure is about 1 bar (100 kPa), CNS toxicity can only occur under hyperbaric conditions, where ambient pressure is above normal.[1][28][29]
Divers breathing air at depths greater than 60 metres (200 feet) face a risk of an oxygen toxicity "hit" (seizure). Divers using a gas mixture enriched with oxygen (nitrox) who descend below the maximum depth allowed for the mixture can similarly suffer a CNS seizure at lesser depths.[19]
Pulmonary toxicity
The lungs have a very large area in contact with the breathing gas and contain thin membranes with limited antioxidant defenses, making them particularly susceptible to damage by oxygen. Pulmonary toxicity occurs with prolonged exposure of 16–24 hours or more to elevated concentrations of oxygen greater than 50%. Pulmonary manifestations of oxygen toxicity are not the same for normobaric conditions as they are for hyperbaric conditions.[30]
The risk of bronchopulmonary dysplasia ("BPD") in infants, or acute respiratory distress syndrome (ARDS) in adults, begins to increase with exposure for over 16 hours to oxygen partial pressures (ppO2) of 0.5 bar (50 kPa) or more.[31][32][33] At sea-level, 0.5 bar (50 kPa) is exceeded by gas mixtures having oxygen fractions greater than 50%, while the rate of damage rises non-linearly between the 50% threshold of toxicity and the rate at 100% oxygen. Partial pressures between 0.2 bar (20 kPa) (normal ppO2 at sea level) and 0.5 bar (50 kPa) are considered non-toxic but intensive care patients breathing more than 60% oxygen, and especially patients at fractions near 100% oxygen, are considered to be at particularly high risk. If the treatment continues for a lengthy period, it may begin to cause lung damage which exacerbates the original problem requiring the high-oxygen mixture. Oxygen toxicity is also a potential complication of mechanical ventilation with oxygen fractions above 50%.[33][34]
Breathing 100% oxygen eventually leads to collapse of the alveoli (atelectasis), while — at same partial pressure of oxygen — the presence of significant partial pressures of inert gases will prevent this effect.[35] In the treatment of decompression sickness, divers are exposed to long periods of oxygen breathing under hyperbaric conditions. This exposure, coupled with that from the dive preceding the symptoms, can be a significant cumulative oxygen exposure and pulmonary toxicity may occur.[28]
Ocular toxicity
Prolonged exposure to high inspired fractions of oxygen causes damage to the retina.[36][37][38][39] Damage to the developing eye of infants exposed to high oxygen fraction at normal pressure has a different mechanism and effect from the eye damage experienced by adult divers under hyperbaric conditions.[40][41] Hyperoxia may be a contributing factor for the disorder called retrolental fibroplasia or retinopathy of prematurity (ROP) in infants.[36][40] In preterm infants, the retina is often not fully vascularised. ROP occurs when the development of the retinal vasculature is arrested and then proceeds abnormally. Associated with the growth of these new vessels is fibrous tissue (scar tissue) that may contract to cause retinal detachment. Supplemental oxygen exposure, while a risk factor, is not the main risk factor for development of this disease. Restricting supplemental oxygen use does not necessarily reduce the rate of ROP, and may raise the risk of other hypoxia-related systemic complications.[40]
Hyperoxic myopia has occurred in closed circuit oxygen rebreather divers with prolonged exposures.[41][37][42][43] This is due to an increase in the refractive power of the lens, since axial length and keratometry readings do not reveal a corneal or length basis for a myopic shift.[44][45]
Mechanism

A high concentration of oxygen damages cells.[16] Higher than normal concentrations lead to increased levels of reactive oxygen species (ROS),[46] and while not all mechanisms of damage are understood, the process of lipid peroxidation is known to cause damage to cell membranes.[47] ROS form as a natural byproduct of the normal metabolism of oxygen and have important roles in cell signaling. However, during times of environmental stress ROS levels can increase dramatically, which can result in significant damage to cell structures. This cumulates into a situation known as oxidative stress.[16][48] One example is that oxygen has a propensity to react with certain metals to form the ROS superoxide, which attacks double bonds in many organic molecules, including the unsaturated fatty acid residues in cells.[49][50] High concentrations of oxygen are also known to increase the formation of free radicals which harm DNA and other structures (see nitric oxide, peroxynitrite, and trioxidane).[16][51] Normally the body has many defense systems against such injury, such as glutathione, catalase, and superoxide dismutase, but at higher concentrations of free oxygen, these systems are eventually overwhelmed, and the rate of damage to cell membranes exceeds the capacity of the systems which control or repair it.[52][53][54] Cell damage and cell death then result.[55]
Diagnosis
Diagnosis of central nervous system (CNS) oxygen toxicity in divers prior to seizure is difficult as the symptoms of visual disturbance, ear problems, dizziness, confusion and nausea can be due to many factors common to the underwater environment such as narcosis, congestion and coldness. However, these symptoms may be helpful in diagnosing the first stages of oxygen toxicity in patients undergoing hyperbaric oxygen therapy. In either case, unless there is a prior history of epilepsy or tests indicate hypoglycemia, a seizure occurring while breathing oxygen at partial pressures greater than 1.4 bar (140 kPa) will be diagnosed as oxygen toxicity by exclusion.
Diagnosis of bronchopulmonary dysplasia (BPD) in new-born infants with breathing difficulties is difficult in the first few weeks. However, if the infant's breathing does not improve during this time, blood tests and x-rays may be used to confirm BPD. In addition, an echocardiogram can help to eliminate other possible causes such as congenital heart defects or pulmonary arterial hypertension.[56]
The diagnosis of retinopathy of prematurity (ROP) in infants is typically suggested by the clinical setting. Prematurity, low birth weight and a history of oxygen exposure are the principal indicators, while no hereditary factors have been shown to yield a pattern.[57]
Prevention

A seizure caused by central nervous system (CNS) oxygen toxicity is a deadly but entirely avoidable event while diving.[19] The diver may experience no warning symptoms. The effects are sudden convulsions and unconsciousness, during which victims can lose their regulator and drown.[1][15] One of the advantages of a full-face diving mask is to prevent losing the regulator in the event of a seizure. As there is an increased risk of CNS oxygen toxicity on deep dives, long dives and dives where oxygen-rich breathing gases are used, divers are taught to calculate a maximum operating depth for oxygen-rich breathing gases; and cylinders containing such mixtures must be clearly marked with that depth.[19][21]
In some diver training courses for these types of diving, divers are taught to plan and monitor what is called the "oxygen clock" of their dives.[19] This is a notional alarm clock, which "ticks" more quickly at increased ppO2 and is set to activate at the maximum single exposure limit recommended in the National Oceanic and Atmospheric Administration (NOAA) Diving Manual.[19][21] For the following partial pressures of oxygen the limit is: 45 minutes at 1.6 bar (160 kPa), 120 minutes at 1.5 bar (150 kPa), 150 minutes at 1.4 bar (140 kPa), 180 minutes at 1.3 bar (130 kPa) and 210 minutes at 1.2 bar (120 kPa), but is impossible to predict with any reliability whether or when CNS symptoms will occur.[1][15][58][59] Many Nitrox-capable dive computers calculate an "oxygen loading" and can track it across multiple dives. The aim is to avoid activating the alarm by reducing the ppO2 of the breathing gas or the length of time breathing gas of higher ppO2. As the ppO2 depends on the fraction of oxygen in the breathing gas and the depth of the dive, the diver obtains more time on the oxygen clock by diving at a shallower depth, by breathing a less oxygen-rich gas or by shortening the duration of exposure to oxygen-rich gases.[60][14]
Pulmonary oxygen toxicity is an entirely avoidable event while diving. The limited duration and naturally intermittent nature of most diving makes this a relatively rare (and even then, reversible) complication for divers. Guidelines have been established that allow divers to calculate when they are at risk of pulmonary toxicity.[1][15][61][62][63][64]
Bronchopulmonary dysplasia (BPD) is reversible in the early stages by use of "break periods" on lower oxygen pressures, but it may eventually result in irreversible lung injury if allowed to progress to severe damage. One or two days of exposure without "oxygen breaks" are needed to cause such damage.[65]
In low-pressure environments oxygen toxicity may be avoided since the toxicity is caused by high oxygen partial pressure, not merely by high oxygen fraction. This is illustrated by modern pure oxygen use in spacesuits, which must operate at low pressure (also historically, very high percentage oxygen and lower than normal atmospheric pressure was used in early spacecraft, for example, the Gemini and Apollo spacecraft).[66] In such applications as extra-vehicular activity (EVA), high-fraction oxygen is non-toxic, even at breathing mixture fractions approaching 100%, because the oxygen partial pressure is not allowed to chronically exceed 0.3 bar (4.4 psi).[66]
Vitamin E and selenium were proposed and later rejected as a potential method of protection against pulmonary oxygen toxicity.[67][68][69] There is however some experimental evidence in rats that vitamin E and selenium aid in preventing in vivo lipid peroxidation and free radical damage, and therefore prevent retinal changes following repetitive hyperbaric oxygen exposures.[70]
Management
Treatment of seizures during oxygen therapy consists of removing the patient from oxygen, thereby dropping the partial pressure of oxygen delivered.[15] A seizure underwater requires that the diver is brought to the surface as soon as practicable. The buddy will ensure that the victim's air supply is established and maintained, then carry out a controlled buoyant lift. The buddy will need to ensure their own safety is not compromised during the convulsive phase, but lifting an unconscious body is taught by most diver training agencies. Upon reaching the surface, emergency services should be contacted as there is a possibility of further complications requiring medical attention.[71]
The occurrence of symptoms of bronchopulmonary dysplasia (BPD) or acute respiratory distress syndrome (ARDS) is treated by lowering the fraction of oxygen administered, along with a reduction in the periods of exposure and an increase in the break periods where normal air is supplied. Where supplemental oxygen is required for treatment of another disease (particularly in infants), a ventilator may be needed to ensure that the lung tissue remains inflated. Reductions in pressure and exposure will be made progressively and medications such as bronchodilators and pulmonary surfactants may be used.[72]
Retinopathy of prematurity (ROP) may regress spontaneously, but should the disease progress beyond a threshold (defined as five contiguous or eight cumulative hours of stage 3 ROP), both cryosurgery and laser surgery have been shown to reduce the risk of blindness as an outcome. Where the disease has progressed further, techniques such as scleral buckling and vitrectomy surgery may assist in re-attaching the retina.[57]
Prognosis
Although the convulsions caused by central nervous system (CNS) oxygen toxicity may lead to incidental injury to the victim, it remained uncertain for many years whether damage to the nervous system following the seizure could occur and several studies searched for evidence of such damage. An overview of these studies by Bitterman in 2004 concluded that following removal of breathing gas containing high fractions of oxygen, no long-term neurological damage from the seizure remains.[16][73]
The majority of infants who have survived following an incidence of bronchopulmonary dysplasia (BPD) will eventually recover near-normal lung function, since lungs continue to grow during the first 5–7 years and the damage caused by BPD is to some extent reversible (even in adults). However, they are likely be more susceptible to respiratory infections for the rest of their lives and the severity of later infections is often greater than that in their peers.[74][75]
Retinopathy of prematurity (ROP) in infants frequently regresses without intervention and eyesight may be normal in later years. Where the disease has progressed to the stages requiring surgery, the outcomes are generally good for the treatment of stage 3 ROP, but are much worse for the later stages. Although surgery is usually successful in restoring the anatomy of the eye, damage to the nervous system by the progression of the disease leads to comparatively poorer results in restoring vision. The presence of other complicating diseases also reduces the likelihood of a favourable outcome.[57]
Epidemiology

The incidence of central nervous system (CNS) toxicity among divers has decreased since the Second World War, as protocols have developed to limit exposure and partial pressure of oxygen inspired. In 1947, Donald recommended limiting the depth breathing pure oxygen to 7.6 m (25 ft), or a ppO2 of 1.8 bar (180 kPa).[76] This limit has been reduced until today a limit of 1.4 bar (140 kPa) during a recreational dive and 1.6 bar (160 kPa) during shallow decompression stops is accepted: oxygen toxicity has become a rare occurrence other than when caused by equipment malfunction and human error. Historically, the U.S. Navy has refined its Navy Diving Manual Tables to reduce oxygen toxicity incidents. Between 1995 and 1999, reports showed 405 surface-supported dives using the helium-oxygen tables; of these, oxygen toxicity symptoms were observed on 6 dives (1.5%). As a result, the U.S. Navy in 2000 modified the schedules and conducted field tests of 150 dives, none of which produced symptoms of oxygen toxicity. Revised tables were published in 2001.[77]
The variability in tolerance and other variable factors such as workload have resulted in the U.S. Navy abandoning screening for oxygen tolerance. Of the 6,250 oxygen-tolerance tests performed between 1976 and 1997, only 6 episodes of oxygen toxicity were observed (0.1%).[78][79]
The incidence of CNS oxygen toxicity among patients undergoing hyperbaric oxygen therapy is rare and influenced by a number of a factors: individual sensitivity and treatment protocol; and probably therapy indication and equipment used. A study by Welslau in 1996 reported 16 incidents out of a population of 107,264 patients (0.015%), while Hampson and Atik in 2003 found a rate of 0.03%.[80][81] Yildiz, Ay and Qyrdedi, in a summary of 36,500 patient treatments between 1996 and 2003, reported only 3 oxygen toxicity incidents, giving a rate of 0.008%.[82]
Bronchopulmonary dysplasia (BPD) is among the most common complications of prematurely born infants and its incidence has grown as the survival of extremely premature infants has increased. Nevertheless, the severity has decreased as better management of supplemental oxygen has resulted in the disease now being related mainly to factors other than hyperoxia.[31]
In 1997 a summary of studies of neonatal intensive care units in industrialised countries showed that up to 60% of low birth weight babies develop retinopathy of prematurity (ROP) , which rises to 72% in extremely low birth weight babies, i.e. less than 1 kilogram (2.2 pounds) at birth. However, severe outcomes are much less frequent: for very low birth weight babies (defined as less than 1.5 kg (3.3 lb) at birth), the incidence of blindness was found to be no more than 8%.[83]
History

Central nervous system (CNS) toxicity was first described by Paul Bert in 1878.[1][84][85] He showed that oxygen was toxic to insects, arachnids, myriapods, molluscs, earthworms, fungi, germinating seeds, birds, and other animals. CNS toxicity may be referred to as the "Paul Bert effect".[13] Pulmonary oxygen toxicity was first described by J. Lorrain Smith in 1899 when he noted CNS toxicity and discovered in experiments in mice and birds that 0.43 bar (43 kPa) had no effect but 0.75 bar (75 kPa) of oxygen was a pulmonary irritant.[26] Pulmonary toxicity may be referred to as the "Lorrain Smith effect"[13] The first recorded human exposure was undertaken in 1910 by Bornstein when two men breathed oxygen at 2.8 bar (280 kPa) for 30 minutes while he went on to 48 minutes with no symptoms.[86] In 1912, Bornstein developed cramps in his hands and legs while breathing oxygen at 2.8 bar (280 kPa) for 51 minutes.[87] Smith then went on to show that intermittent exposure to a breathing gas with less oxygen permitted the lungs to recover and delayed the onset of pulmonary toxicity.[26]
Behnke et al. in 1935 were the first to observe visual field contraction (tunnel vision) on dives between 1.0 bar (100 kPa) and 4.1 bar (410 kPa).[88][89] During World War II, Donald and Yarbrough et al. performed over 2,000 experiments on oxygen toxicity to support the initial use of closed circuit oxygen rebreathers.[17][18][76][37] Naval divers in the early years of oxygen rebreather diving developed a mythology about a monster called "Oxygen Pete", who lurked in the bottom of the Admiralty Experimental Diving Unit "wet pot" (a water-filled hyperbaric chamber) to catch unwary divers. They called having an oxygen toxicity attack "getting a Pete".[90][91]
In the decade following World War II, Lambertsen et al. made further discoveries on the effects of oxygen at pressure as well as methods of prevention.[92][93] Their work on intermittent exposures for extension of oxygen tolerance and on a model for prediction of pulmonary oxygen toxicity based on pulmonary function are key documents in the development of operational oxygen procedures.[61][94] Lambertsen's work showing the effect of carbon dioxide in decreasing time to onset of CNS symptoms has influenced work from current exposure guidelines to future breathing apparatus design.[19][20][21]
Retinopathy of prematurity (ROP) was not observed prior to World War II, but with the availability of supplemental oxygen in the decade following, it rapidly became one of the principal causes of infant blindness in developed countries. By 1960 the use of oxygen had become identified as a risk factor and its administration restricted. The resulting fall in ROP was accompanied by a rise in infant mortality and hypoxia-related complications. Since then, more sophisticated monitoring and diagnosis has established protocols for oxygen use which aim to balance between hypoxic conditions and problems of ROP.[83]
Bronchopulmonary dysplasia (BPD) was first described by Northway in 1967, who outlined the conditions that would lead to the diagnosis.[95] This was later expanded by Bancalari and in 1988 by Shennan, who suggested the need for supplemental oxygen at 36 weeks could predict long-term outcomes.[96] Nevertheless, Palta et al in 1998 concluded that radiographic evidence was the most accurate predictor of long-term effects.[97]
Bitterman et al. in 1986 and 1995 showed that darkness and caffeine will delay the onset of changes to brain electrical activity in rats.[22][23] In the years since, research on CNS toxicity has centered around methods of prevention and safe extension of tolerance.[98] These include topics such as circadian rhythm, drugs, age, and gender that have been shown to contribute to CNS oxygen toxicity sensitivity.[99][100][101][102] In 1988, Hamilton et al. wrote procedures for the National Oceanic and Atmospheric Administration (NOAA) to establish oxygen exposure limits for habitat operations.[1][62][63][64] Even today, models for the prediction of pulmonary oxygen toxicity do not explain all the results of exposure to high partial pressures of oxygen.[103]
Society and culture
Recreational divers who use breathing mixtures with oxygen fractions greater than air have to be trained in the potential dangers of oxygen toxicity and how to prevent them.[19] In order to buy nitrox, a diver has to show evidence of a nitrox qualification.[104]
Since the late 1990s the recreational use of oxygen has been promoted by oxygen bars, where customers breathe air enriched to less than 50% oxygen. Claims have been made that this reduces stress, increases energy, and lessens the effects of hangovers and headaches, despite the lack of any scientific evidence to support them.[105] There are also devices on sale that offer "oxygen massage" and "oxygen detoxification" with claims of removing body toxins and reducing body fat.[106] The American Lung Association has stated "there is no evidence that oxygen at the low flow levels used in bars can be dangerous to a normal person's health", but the U.S. Center for Drug Evaluation and Research (CDER) cautions that people with heart or lung disease need their supplementary oxygen carefully regulated and should not use oxygen bars.[105]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 Brubakk, Alf O.; Neuman, Tom S. (2003). Bennett and Elliott's physiology and medicine of diving, 5th Rev ed. Edinburgh; New York: Saunders, 800 pages. ISBN 0702025712. OCLC 51607923.
- ↑ Acott, Chris (1999). "Oxygen toxicity: A brief history of oxygen in diving". South Pacific Underwater Medicine Society journal 29 (3). ISSN 0813-1988. OCLC 16986801. http://archive.rubicon-foundation.org/6014. Retrieved on 2008-04-29.
- ↑ Beehler, C.C. (December 1964). "Oxygen and the eye". Survey of ophthalmology 45: 549–60. PMID 14232720.
- ↑ Goldstein, J.R.; Mengel, C.E. (January 1969). "Hemolysis in mice exposed to varying levels of hyperoxia". Aerospace medicine 40 (1): 12–3. PMID 5782651.
- ↑ Larkin, E.C.; Adams. J.D.; Williams, W.T.; Duncan, D.M. (August 1972). "Hematologic responses to hypobaric hyperoxia". The American journal of physiology 223 (2): 431–7. PMID 4403030. http://ajplegacy.physiology.org/cgi/pmidlookup?view=long&pmid=4403030. Retrieved on 2008-09-28.
- ↑ Schaffner, Fenton; Felig, Philip (December 1965). "Changes in hepatic structure in rats produced by breathing pure oxygen". The Journal of cell biology 27 (3): 505–17. doi:. PMID 5885427. PMC: 2106769. http://www.jcb.org/cgi/pmidlookup?view=long&pmid=5885427. Retrieved on 2008-09-28.
- ↑ Caulfield, J.B.; Shelton, R.W.; Burke, J.F. (August 1972). "Cytotoxic effects of oxygen on striated muscle". Archives of pathology 94 (2): 127–32. PMID 5046798.
- ↑ Bean, J.W.; Johnson, P.C. (December 1954). "Adrenocortical response to single and repeated exposure to oxygen at high pressure". The American journal of physiology 179 (3): 410–4. PMID 13228600. http://ajplegacy.physiology.org/cgi/pmidlookup?view=long&pmid=13228600. Retrieved on 2008-09-28.
- ↑ Edstrom, J.E.; Rockert, H. (1962). "The effect of oxygen at high pressure on the histology of the central nervous system and sympathetic and endocrine cells". Acta physiologica Scandinavica 55: 255–63. PMID 13889254.
- ↑ Gersh, I.; Wagner, C.E. (1945). "Metabolic factors in oxygen posoning". The American journal of physiology 144: 270–277. http://ajplegacy.physiology.org/cgi/reprint/144/2/270. Retrieved on 2008-10-08.
- ↑ Hess, R.T.; Menzel, D.B. (June 1971). "Effect of dietary antioxidant level and oxygen exposure on the fine structure of the proximal convoluted tubules". Aerospace medicine 42 (6): 646–9. PMID 5155150.
- ↑ Clark, John M. (December 1974). "The toxicity of oxygen". The American review of respiratory disease 110 (6 Pt 2): 40–50. PMID 4613232.
- ↑ 13.0 13.1 13.2 13.3 Patel, Dharmeshkumar N; Goel, Ashish; Agarwal, S.B.; Garg, Praveenkumar; Lakhani, Krishna K. (July 2003). "Oxygen toxicity" (PDF). Journal, Indian Academy of Clinical Medicine 4 (3): 234–7. http://medind.nic.in/jac/t03/i3/jact03i3p234.pdf. Retrieved on 2008-09-28.
- ↑ 14.0 14.1 Clark, John M.; Lambertsen, Christian J. (1970). "Pulmonary Oxygen Tolerance in Man and Derivation of Pulmonary Oxygen Tolerance Curves" 157–62. Pennsylvania University, Philadelphia School of Medicine. Retrieved on 2008-10-19.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. 2006. http://www.supsalv.org/00c3_publications.asp?destPage=00c3&pageID=3.9. Retrieved on 2008-04-24.
- ↑ 16.0 16.1 16.2 16.3 16.4 Bitterman, N. (2004). "CNS oxygen toxicity". Undersea and Hyperbaric Medicine 31 (1): 63–72. PMID 15233161. http://archive.rubicon-foundation.org/3991. Retrieved on 2008-04-29.
- ↑ 17.0 17.1 Donald, Kenneth W. (1947). "Oxygen and the diver: Part I". British medical journal 1(4506): 667–672.
- ↑ 18.0 18.1 Donald, Kenneth W. (1947). "Oxygen and the diver: Part II". British medical journal 1(4506): 712–717.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 Lang, Michael A. (ed.) (2001). DAN nitrox workshop proceedings. Durham, NC: Divers Alert Network. pp. 197. http://archive.rubicon-foundation.org/4855. Retrieved on 2008-09-20.
- ↑ 20.0 20.1 Richardson, Drew; Menduno, Michael; Shreeves, Karl (eds) (1996). "Proceedings of rebreather forum 2.0.". Diving Science and Technology Workshop.: 286. http://archive.rubicon-foundation.org/7555. Retrieved on 2008-09-20.
- ↑ 21.0 21.1 21.2 21.3 Richardson, Drew; Shreeves, Karl (1996). "The PADI enriched air diver course and DSAT oxygen exposure limits.". South Pacific Underwater Medicine Society journal 26 (3). ISSN 0813-1988. OCLC 16986801. http://archive.rubicon-foundation.org/6310. Retrieved on 2008-05-02.
- ↑ 22.0 22.1 Bitterman, N.; Melamed, Y.; Perlman, I.; (March 1986). "CNS oxygen toxicity in the rat: role of ambient illumination". Undersea Biomedical Research 13 (1): 19–25. PMID 3705247. http://archive.rubicon-foundation.org/3044. Retrieved on 2008-09-20.
- ↑ 23.0 23.1 Bitterman, N.; Schaal, S.; (October 1995). "Caffeine attenuates CNS oxygen toxicity in rats". Brain Research 696 (1-2): 250–3. doi:. PMID 8574677. http://linkinghub.elsevier.com/retrieve/pii/0006-8993(95)00820-G. Retrieved on 2008-09-20.
- ↑ 24.0 24.1 Clark, John M.; Lambertsen, Christian J. (June 1971). "Pulmonary oxygen toxicity: a review". Pharmacological reviews 23 (2): 37–133. PMID 4948324. http://pharmrev.aspetjournals.org/cgi/pmidlookup?view=long&pmid=4948324. Retrieved on 2008-10-10.
- ↑ 25.0 25.1 25.2 Clark, John M.; Lambertsen, Christian J. (May 1971). "Rate of development of pulmonary O2 toxicity in man during O2 breathing at 2.0 Ata". Journal of applied physiology 30 (5): 739–52. PMID 4929472. http://jap.physiology.org/cgi/pmidlookup?view=long&pmid=4929472. Retrieved on 2008-10-10.
- ↑ 26.0 26.1 26.2 Smith, J.Lorrain (22 March 1899). "The pathological effects due to increase of oxygen tension in the air breathed". Journal of Physiology (London: The Physiological Society and Blackwell Publishing) 24 (1): 19–35. PMID 16992479. http://www.jphysiol.org/cgi/pmidlookup?view=long&pmid=16992479. Note: 1 atmosphere (atm) is 1.013 bars.
- ↑ Fielder, Alistair R. (1993). Fielder, Alistair R.; Best, Anthony; Bax, Martin C. O. ed.. The Management of Visual Impairment in Childhood. London: Mac Keith Press : Distributed by Cambridge University Press. pp. 33. ISBN 0521451507. http://books.google.co.uk/books?id=jeLd0aHdrMAC&pg=PA32&lpg=PA32#PPA33,M1. Retrieved on 2008-10-22.
- ↑ 28.0 28.1 Smerz, R.W. (2004). "Incidence of oxygen toxicity during the treatment of dysbarism". Undersea and Hyperbaric Medicine 31 (2): 199–202. PMID 15485081. http://archive.rubicon-foundation.org/4010. Retrieved on 2008-04-30.
- ↑ Hampson, Neal B.; Simonson, Steven G.; Kramer, C.C.; Piantadosi, Claude A. (December 1996). "Central nervous system oxygen toxicity during hyperbaric treatment of patients with carbon monoxide poisoning". Undersea and Hyperbaric Medicine 23 (4): 215–9. PMID 8989851. http://archive.rubicon-foundation.org/2232. Retrieved on 2008-04-29.
- ↑ Demchenko, Ivan T.; Welty-Wolf, Karen E.; Allen, Barry W.; Piantadosi, Claude A. (July 2007). "Similar but not the same: normobaric and hyperbaric pulmonary oxygen toxicity, the role of nitric oxide". The American journal of physiology Lung Cell Mol. Physiol. 293 (1): L229–38. doi:. PMID 17416738. http://ajplung.physiology.org/cgi/pmidlookup?view=long&pmid=17416738. Retrieved on 2008-09-18.
- ↑ 31.0 31.1 Bancalari, Eduardo; Claure, Nelson; Sosenko, Ilene R.S. (February 2003). "Bronchopulmonary dysplasia: changes in pathogenesis, epidemiology and definition". Seminars in Neonatology (London: Elsevier Science) 8 (1): 63–71. doi:. ISSN 1084-2756. PMID 12667831. http://linkinghub.elsevier.com/retrieve/pii/S1084275602001926. Retrieved on 2008-04-30.
- ↑ Tin, W.; Gupta, S. (March 2007). "Optimum oxygen therapy in preterm babies". Archives of disease in childhood. Fetal and neonatal edition 92 (2): F143–7. doi:. PMID 17337663. http://fn.bmj.com/cgi/pmidlookup?view=long&pmid=17337663. Retrieved on 2008-04-30.
- ↑ 33.0 33.1 Thiel, Manfred; Chouker, Alexander; Ohta, Akio; et al (June 2005). "Oxygenation inhibits the physiological tissue-protecting mechanism and thereby exacerbates acute inflammatory lung injury". PLoS biology 3 (6): e174. doi:. PMID 15857155. http://biology.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pbio.0030174. Retrieved on 2008-04-30.
- ↑ Byrd, Ryland P. (July 2006). "Complications of mechanical ventilation". WebMD. Retrieved on 2008-10-20.
- ↑ Wittner, M.; Rosenbaum, R.M. (1966). "Pathophysiology of pulmonary oxygen toxicity". Proceedings of the Third International Conference on Hyperbaric Medicine: 179-188, NAS/NRC, 1404, Washington DC. - and others as discussed by Clark, John M. and Lambertsen, Christian J. (1970) Pulmonary oxygen tolerance in man and derivation of pulmonary oxygen tolerance curves pages 256-260.
- ↑ 36.0 36.1 Nichols, C.W.; Lambertsen Christian (July 1969). "Effects of high oxygen pressures on the eye". New England Journal of Medicine 281 (1): 25–30. PMID 4891642.
- ↑ 37.0 37.1 37.2 Yarbrough, O.D.; Welham, W.; Brinton, E.S.; Behnke, Alfred R. (1947). "Symptoms of Oxygen Poisoning and Limits of Tolerance at Rest and at Work". U.S. Naval experimental diving unit technical report NEDU-47-01. http://archive.rubicon-foundation.org/3316. Retrieved on 2008-04-29.
- ↑ Anderson, B.; Farmer, Joseph C. (1978). "Hyperoxic myopia". Trans Am Ophthalmol Soc 76: 116–24. PMID 754368.
- ↑ Ricci, B.; Lepore, D.; Iossa, M.; Santo, A.; D'Urso, M.; Maggiano, N. (1990). "Effect of light on oxygen-induced retinopathy in the rat model. Light and OIR in the rat". Documenta ophthalmologica 74 (4): 287–301. doi:. PMID 1701697.
- ↑ 40.0 40.1 40.2 Drack, A.V. (May 1998). "Preventing blindness in premature infants". New England Journal of Medicine 338 (22): 1620–1. doi:. PMID 9603802. http://content.nejm.org/cgi/content/full/338/22/1619. Retrieved on 2008-09-19.
- ↑ 41.0 41.1 Butler, Frank K.; White, E.; Twa, M. (1999). "Hyperoxic myopia in a closed-circuit mixed-gas scuba diver". Undersea and Hyperbaric Medicine 26 (1): 41–5. PMID 10353183. http://archive.rubicon-foundation.org/2312. Retrieved on 2008-04-29.
- ↑ Shykoff, Barbara E. (2005). "Repeated Six-Hour Dives 1.35 ATM Oxygen Partial Pressure". US Naval Experimental Diving Unit Technical Report (Panama City, FL, USA) NEDU-TR-05-20. http://archive.rubicon-foundation.org/3492. Retrieved on 2008-09-19.
- ↑ Shykoff, Barbara E. (2008). "Pulmonary effects of submerged oxygen breathing in resting divers: repeated exposures to 140 kPa". Undersea and Hyperbaric Medicine 35 (2): 131–43. PMID 18500077.
- ↑ Anderson, B.; Shelton, D.L. (1987). "Axial length in hyperoxic myopia". In: Bove, Alfred A.; Bachrach, Arthur J.; Greenbaum, Leon (eds.) Underwater and hyperbaric physiology IX. Ninth international symposium of the Undersea and Hyperbaric Medical Society: 607–11.
- ↑ Schaal, S.; Beiran, I.; Rubinstein, I.; Miller, B.; Dovrat, A. (November 2005). "Oxygen effect on ocular lens" (in Hebrew). Harefuah 144 (11): 777–80, 822. PMID 16358652.
- ↑ Fridovich, I (01 April 1998). "Oxygen toxicity: a radical explanation". Journal of Experimental Biology 201 (8): 1203–1209. PMID 9510531. http://jeb.biologists.org/cgi/reprint/201/8/1203.
- ↑ Bowen, R.. "Free Radicals and Reactive Oxygen". Colorado State University. Retrieved on 2008-09-26.
- ↑ Piantadosi, Claude A. (September 2008). "Carbon monoxide, reactive oxygen signaling, and oxidative stress". Free radical biology and medicine 45 (5): 562–9. doi:. PMID 18549826. http://linkinghub.elsevier.com/retrieve/pii/S0891-5849(08)00305-5. Retrieved on 2008-09-26.
- ↑ Thom, Steven R. (June 1992). "Inert gas enhancement of superoxide radical production". Archives of biochemistry and biophysics 295 (2): 391–6. doi:. PMID 1316738.
- ↑ Ghio, Andrew J.; Nozik-Grayck, Eva; Turi, Jennifer; Jaspers, Ilona; Mercatante, Danielle R.; Kole, Ryszard; Piantadosi, Claude A. (December 2003). "Superoxide-dependent iron uptake: a new role for anion exchange protein 2". American journal of respiratory cell and molecular biology 29 (6): 653–60. doi:. PMID 12791678. http://ajrcmb.atsjournals.org/cgi/pmidlookup?view=long&pmid=12791678. Retrieved on 2008-09-26.
- ↑ Oury, T.D.; Ho, Y.S.; Piantadosi, Claude A.; Crapo, J.D. (October 1992). "Extracellular superoxide dismutase, nitric oxide, and central nervous system O2 toxicity". Proceedings of the National Academy of Sciences of the United States of America 89 (20): 9715–9. doi:. PMID 1329105. PMC: 50203. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=1329105. Retrieved on 2008-09-26.
- ↑ Thom, Steven R.; Marquis, R.E. (November 1987). "Free radical reactions and the inhibitory and lethal actions of high-pressure gases". Undersea Biomedical Research 14 (6): 485–501. PMID 2825395. http://archive.rubicon-foundation.org/2459. Retrieved on 2008-09-26.
- ↑ Djurhuus, R.; Svardal, A.M.; Thorsen, E. (1999). "Glutathione in the cellular defense of human lung cells exposed to hyperoxia and high pressure". Undersea and Hyperbaric Medicine 26 (2): 75–85. PMID 10372426. http://archive.rubicon-foundation.org/2315. Retrieved on 2008-09-26.
- ↑ Freiberger, John J.; Coulombe, Kathy; Suliman, Hagir; Carraway, Martha-sue; Piantadosi, Claude A. (2004). "Superoxide dismutase responds to hyperoxia in rat hippocampus". Undersea and Hyperbaric Medicine 31 (2): 227–32. PMID 15485085. http://archive.rubicon-foundation.org/4014. Retrieved on 2008-09-26.
- ↑ Kim, Y.S.; Kim, S.U. (May 1991). "Oligodendroglial cell death induced by oxygen radicals and its protection by catalase". Journal of neuroscience research 29 (1): 100–6. doi:. PMID 1886163.
- ↑ "How is bronchopulmonary dysplasia diagnosed?". U.S. Department of Health & Human Services. Retrieved on 2008-09-28.
- ↑ 57.0 57.1 57.2 Regillo, Carl D.; Brown, Gary C.; Flynn, Harry W. (1998). Vitreoretinal Disease: The Essentials. New York: Thieme, 693 pages. ISBN 0865777616. OCLC 39170393. http://books.google.co.uk/books?id=QUTuvcB68DEC.
- ↑ Butler, Frank K.; Thalmann, Edward D. (June 1986). "Central nervous system oxygen toxicity in closed circuit scuba divers II". Undersea Biomedical Research 13 (2): 193–223. PMID 3727183. http://archive.rubicon-foundation.org/3045. Retrieved on 2008-04-29.
- ↑ Butler, Frank K. (2004). "Closed-circuit oxygen diving in the U.S. Navy". Undersea and Hyperbaric Medicine 31 (1): 3–20. PMID 15233156. http://archive.rubicon-foundation.org/3986. Retrieved on 2008-04-29.
- ↑ Baker, Erik C.. "Oxygen toxicity calculations" (PDF) 1–2. Retrieved on 2008-10-19.
- ↑ 61.0 61.1 Clark, John M. (2004). "Extension of oxygen tolerance by interrupted exposure". Undersea and Hyperbaric Medicine 31 (2): 195–8. PMID 15485080. http://archive.rubicon-foundation.org/4009. Retrieved on 2008-04-29.
- ↑ 62.0 62.1 Hamilton R W., Kenyon David J., Peterson R. E., Butler G. J., Beers D. M. (1988). "Repex habitat diving procedures: Repetitive vertical excursions, oxygen limits, and surfacing techniques.". NOAA Office of Undersea Research (Rockville, MD) Technical Report 88-1A. http://archive.rubicon-foundation.org/4865. Retrieved on 2008-04-29.
- ↑ 63.0 63.1 Hamilton, Robert W.; Kenyon, David J.; Peterson, R.E. (1988). "Repex habitat diving procedures: Repetitive vertical excursions, oxygen limits, and surfacing techniques.". NOAA Office of Undersea Research (Rockville, MD) Technical Report 88-1B. http://archive.rubicon-foundation.org/4866. Retrieved on 2008-04-29.
- ↑ 64.0 64.1 Hamilton, Robert W. (1997). "Tolerating oxygen exposure". South Pacific Underwater Medicine Society journal 27 (1). ISSN 0813-1988. OCLC 16986801. http://archive.rubicon-foundation.org/6038. Retrieved on 2008-04-29.
- ↑ Patel, Dharmeshkumar N; Goel, Ashish; Agarwal, S.B.; Garg, Praveenkumar; Lakhani, Krishna K. (July 2003). "Oxygen toxicity" (PDF). Journal, Indian Academy of Clinical Medicine 4 (3): 235. http://medind.nic.in/jac/t03/i3/jact03i3p234.pdf. Retrieved on 2008-09-28.
- ↑ 66.0 66.1 Webb, James T.; Olson, R.M.; Krutz, R.W.; Dixon, G.; Barnicott, P.T. (May 1989). "Human tolerance to 100% oxygen at 9.5 psia during five daily simulated 8-hour EVA exposures". Aviation Space and Environmental Medicine 60 (5): 415–21. PMID 2730484.
- ↑ Schatte, C.L. (1977). "Dietary selenium and vitamin E as a possible prophylactic to pulmonary oxygen poisoning". Proceedings of the Sixth International Congress on Hyperbaric Medicine, University of Aberdeen, Aberdeen, Scotland (Aberdeen: Aberdeen University Press): 84–91. ISBN 0-08-024918-3. OCLC 16428246.
- ↑ Boadi, W.Y.; Thaire, L.; Kerem, D.; Yannai, S. (February 1991). "Effects of dietary supplementation with vitamin E, riboflavin and selenium on central nervous system oxygen toxicity". Pharmacology & toxicology 68 (2): 77–82. ISSN 0901-9928. PMID 1852722.
- ↑ Piantadosi, Claude A.. (2006). In: The Mysterious Malady: Toward an understanding of decompression injuries [DVD]. Global Underwater Explorers. Retrieved on 2008-09-19.
- ↑ Stone, W.L.; Henderson, R.A.; Howard, G.H.; Hollis, A.L.; Payne, P.H.; Scott, R.L. (1989). "The role of antioxidant nutrients in preventing hyperbaric oxygen damage to the retina". Free radical biology & medicine 6 (5): 505–12. doi:. PMID 2744583.
- ↑ Thalmann, E.D. (2003-12-02). "OXTOX: If You Dive Nitrox You Should Know About OXTOX". Divers Alert Network. Retrieved on 2008-10-20. - Section "What do you do if oxygen toxicity or a convulsion happens?"
- ↑ "NIH MedlinePlus: Bronchopulmonary dysplasia". U.S. National Library of Medicine. Retrieved on 2008-10-02.
- ↑ Lambertsen, Christian J. (1965). "Effects of oxygen at high partial pressure". In: Fenn, W.O.; Rahn, H. (eds.) Handbook of Physiology: Respiration (American Physiological Society) Sec.3 Vol.2: 1027–46.
- ↑ "National Institutes of Health: What is bronchopulmonary dysplasia?". U.S. Department of Health & Human Services. Retrieved on 2008-10-02.
- ↑ Spear, Michael L. - reviewer, (June 2008). "Bronchopulmonary dysplasia (BPD)". Nemours Foundation. Retrieved on 2008-10-03.
- ↑ 76.0 76.1 Donald, Kenneth W. (1992). Oxygen and the diver.. UK: Harley Swan. pp. 237. ISBN 1854211765.
- ↑ Gerth, Wayne A. (February 2006). "Decompression sickness and oxygen toxicity in U.S. Navy surface-supplied He-O2 diving". Proceedings of Advanced Scientific Diving Workshop (Smithsonian Institution). ISBN 20060725. http://archive.rubicon-foundation.org/4654. Retrieved on 2008-10-02.
- ↑ Walters, K.C.; Gould, M.T.; Bachrach, E.A.; Butler, Frank K. (2000). "Screening for oxygen sensitivity in U.S. Navy combat swimmers". Undersea and Hyperbaric Medicine 27 (1): 21–6. PMID 10813436. http://archive.rubicon-foundation.org/2358. Retrieved on 2008-10-02.
- ↑ Butler, Frank K.; Knafelc, M.E. (March 1986). "Screening for oxygen intolerance in U.S. Navy divers". Undersea Biomedical Research 13 (1): 91–8. PMID 3705251. http://archive.rubicon-foundation.org/3046. Retrieved on 2008-10-02.
- ↑ Welslau, W; Almeling, M (1996). Incidence of oxygen intoxication to central nerve system from Hyperbaric Oxygen Therapy. In: Marroni, A; Oriani, G; Wattel, F (eds.) Proceedings of the International Joint Meeting on Underwater and Hyperbaric Medicine.. Milan. pp. 211–6.
- ↑ Hampson Neal, Atik D (2003). "Central nervous system oxygen toxicity during routine hyperbaric oxygen therapy". Undersea & hyperbaric medicine : journal of the Undersea and Hyperbaric Medical Society, Inc 30 (2): 147–53. PMID 12964858. http://archive.rubicon-foundation.org/3967. Retrieved on 2008-10-20.
- ↑ Yildiz, S,; Ay, H.; Qyrdedi, T. (2004). "Central nervous system oxygen toxicity during routine hyperbaric oxygen therapy". Undersea and Hyperbaric Medicine 31 (2): 189–90. PMID 15485078. http://archive.rubicon-foundation.org/4007. Retrieved on 2008-10-03.
- ↑ 83.0 83.1 Gilbert, Clare (1997). "Retinopathy of prematurity: epidemiology". Journal of Community Eye Health (London: International Centre for Eye Health) 10 (22): 22–24. http://www.cehjournal.org/0953-6833/10/jceh_10_22_022.html. Retrieved on 2008-10-04.
- ↑ Bert, Paul (originally published 1878). "Barometric pressure: Researches in experimental physiology". Translated by: Hitchcock, M.A. And Hitchcock, F.A. College Book Company; 1943. Full text. Retrieved on 2008-10-18.
- ↑ British Sub-aqua Club (1985). Sport diving : the British Sub-Aqua Club diving manual. London: Stanley Paul. pp. 110. ISBN 0091638313. OCLC 12807848.
- ↑ Bornstein, A. (1910). "Versuche über die Prophylaxe der Pressluftkrankheit". Pflügers Archiv European Journal of Physiology 4: 1272–1300.
- ↑ Bornstein, A.; Stroink, M. (1912). "Ueber Sauerstoff vergiftung". Deutsche medizinische Wochenschrift 38: 1495–1497.
- ↑ Behnke, Alfred R.; Johnson, F.S.; Poppen, J.R.; Motley, E.P. (1935). "The effect of oxygen on man at pressures from 1 to 4 atmospheres". The American journal of physiology 110: 565–572. http://ajplegacy.physiology.org/cgi/reprint/110/3/565. Retrieved on 2008-04-29. Note: 1 atmosphere (atm) is 1.013 bars.
- ↑ Behnke, Alfred R.; Forbes, H.S.; Motley, E.P. (1935). "Circulatory and visual effects of oxygen at 3 atmospheres pressure". The American journal of physiology 114: 436–442. http://ajplegacy.physiology.org/cgi/reprint/114/2/436. Retrieved on 2008-04-29. Note: 1 atmosphere (atm) is 1.013 bars.
- ↑ Taylor, Larry "Harris" (1993). "Oxygen Enriched Air: A New Breathing Mix?". IANTD Journal. Retrieved on 2008-09-05.
- ↑ Davis, Robert H. (1955). Deep Diving and Submarine Operations (6th ed.). Tolworth, Surbiton, Surrey: Siebe Gorman & Company Ltd, 693 pages. pp. 291.
- ↑ Lambertsen, Christian J.; Clark, John M.; Gelfand, R. (2000). "The Oxygen research program, University of Pennsylvania: Physiologic interactions of oxygen and carbon dioxide effects and relations to hyperoxic toxicity, therapy, and decompression. Summation: 1940 to 1999". Environmental Biomedical Stress Data Center, Institute for Environmental Medicine, University of Pennsylvania Medical Center (Philadelphia, PA) EBSDC-IFEM Report No. 3-1-2000.
- ↑ Vann, Richard D. (2004). "Lambertsen and O2: Beginnings of operational physiology". Undersea and Hyperbaric Medicine 31 (1): 21–31. PMID 15233157. http://archive.rubicon-foundation.org/3987. Retrieved on 2008-04-29.
- ↑ Clark, John M.; Lambertsen, Christian J. (1970). Pulmonary oxygen tolerance in man and derivation of pulmonary oxygen tolerance curves. IFEM Report No. 1-70. Philadelphia, PA. http://archive.rubicon-foundation.org/3863. Retrieved on 2008-04-29.
- ↑ Northway, W.H.; Rosan, R.C.; Porter, D.Y. (February 1967). "Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia". The New England journal of medicine 276 (7): 357–68. PMID 5334613.
- ↑ Shennan, A.T.; Dunn, M.S.; Ohlsson, A.; Lennox, K.; Hoskins, E.M.; (October 1988). "Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period". Pediatrics 82 (4): 527–32. PMID 3174313.
- ↑ Palta, M.; Sadek, M.; Barnet, J.H.; et al (January 1998). "Evaluation of criteria for chronic lung disease in surviving very low birth weight infants. Newborn Lung Project". The Journal of pediatrics 132 (1): 57–63. doi:. PMID 9470001. http://linkinghub.elsevier.com/retrieve/pii/S0022347698000249.
- ↑ Natoli, M.J.; Vann, R.D. (1996). Factors Affecting CNS Oxygen Toxicity in Humans. Report to the U.S. Office of Naval Research. Durham, NC: Duke University. http://archive.rubicon-foundation.org/21. Retrieved on 2008-04-29.
- ↑ Hof, D.G.; Dexter, J.D.; Mengel, C.E. (December 1971). "Effect of circadian rhythm on CNS oxygen toxicity". Aerospace medicine 42 (12): 1293–6. PMID 5130131.
- ↑ Torley, L.W.; Weiss, H.S. (September 1975). "Effects of age and magnesium ions on oxygen toxicity in the neonate chicken". Undersea Biomedical Research 2 (3): 223–7. PMID 15622741. http://archive.rubicon-foundation.org/2432. Retrieved on 2008-09-20.
- ↑ Troy, S.S.; Ford, D.H. (1972). "Hormonal protection of rats breathing oxygen at high pressure". Acta Neurologica Scandinavica 48 (2): 231–42. PMID 5061633.
- ↑ Hart, George B.; Strauss, Michael B. (2007). "Gender differences in human skeletal muscle and subcutaneous tissue gases under ambient and hyperbaric oxygen conditions". Undersea and Hyperbaric Medicine 34 (3): 147–61. PMID 17672171. http://archive.rubicon-foundation.org/7346. Retrieved on 2008-09-20.
- ↑ Shykoff, Barbara E. (2007). "Performance of various models in predicting vital capacity changes caused by breathing high oxygen partial pressures.". U.S. Naval Experimental Diving Unit Technical Report (Panama City, FL: Navy Experimental Diving Unit) NEDU-TR-07-13. http://archive.rubicon-foundation.org/6867. Retrieved on 2008-06-06.
- ↑ British Sub-Aqua Club (2006). "The Ocean Diver Nitrox Workshop" (PDF) 3. British Sub-Aqua Club. Retrieved on 2008-10-21.
- ↑ 105.0 105.1 Bren, Linda (November 2002). "Oxygen Bars: Is a Breath of Fresh Air Worth It?". FDA Consumer magazine. Retrieved on 2008-10-21.
- ↑ O2Planet (2006). "O2 Planet - Exercise and Fitness Equipment". O2Planet LLC. Retrieved on 2008-10-21.
Bibliography
- Brubakk, Alf O.; Neuman, Tom S. (2003). Bennett and Elliott's physiology and medicine of diving, 5th Rev ed. Edinburgh; New York: Saunders, 800 pages. ISBN 0702025712. OCLC 51607923.
- Donald, Kenneth W. (1992). Oxygen and the diver. UK: Harley Swan, 237 pages. ISBN 1854211765. OCLC 26894235.
- Lippmann, John; Bugg, Stan (1993). The Diving Emergency Handbook. Teddington, UK: Underwater World Publications. ISBN 0-946020-18-3. OCLC 52056845.
- Regillo, Carl D.; Brown, Gary C.; Flynn, Harry W. (1998). Vitreoretinal Disease: The Essentials. New York: Thieme, 693 pages. ISBN 0865777616. OCLC 39170393. http://books.google.co.uk/books?id=QUTuvcB68DEC.
External links
General
The following external site is a compendium of resources:
- Rubicon Research Repository. - Online collection of the oxygen toxicity research
Specialised
The following external sites contain resources specific to particular topics:
- Baker, Erik C (pdf). Oxygen toxicity calculations. decompression.org. ftp://ftp.decompression.org/pub/Baker/Oxygen%20Toxicity%20Calculations.pdf. Retrieved on 2008-09-18. - An explanation of calculations for the "Oxygen clock" with programming examples.
- Toxing diver rescue at YouTube. - A method of rescuing a diver sufficing from oxygen toxicity.
- 2008 Divers Alert Network Technical Diving Conference. - Video of "Oxygen Toxicity" lecture by Dr. Richard Vann (free download, mp4, 86MB).
- Physiology at MCG 4/4ch7/s4ch7_7. - Wide and detailed discussion of the effects of breathing oxygen on the respiratory system.
- Rajiah, Prabhakar (June 2006). "Bronchopulmonary Dysplasia". eMedicine. Retrieved on 2008-10-12. - Concise clinical overview with extensive references.
|
||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||