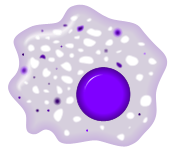
Macrophage

Macrophages (Greek: big eaters, from makros "large" + phagein "eat"; abbr. MΦ) are cells within the tissues that originate from specific white blood cells called monocytes. Human macrophages are about 21 microns in diameter.[1] Monocytes and macrophages are phagocytes, acting in both non-specific defense (or innate immunity) as well as to help initiate specific defense mechanisms (or cell-mediated immunity) of vertebrate animals. Their role is to phagocytose (engulf and then digest) cellular debris and pathogens either as stationary or mobile cells, and to stimulate lymphocytes and other immune cells to respond to the pathogen.
Contents |
Life cycle
When a monocyte enters damaged tissue through the endothelium of a blood vessel (a process known as the leukocyte extravasation), it undergoes a series of changes to become a macrophage. Monocytes are attracted to a damaged site by chemical substances through chemotaxis, triggered by a range of stimuli including damaged cells, pathogens and cytokines released by macrophages already at the site. At some sites such as the testis, macrophages have been shown to populate the organ through proliferation.
Unlike short-lived neutrophils, macrophages survive longer in the body up to a maximum of several months.
Function

a. Ingestion through phagocytosis, a phagosome is formed
b. The fusion of lysosomes with the phagosome creates a phagolysosome; the pathogen is broken down by enzymes
c. Waste material is expelled or assimilated (the latter not pictured)
Parts:
1. Pathogens
2. Phagosome
3. Lysosomes
4. Waste material
5. Cytoplasm
6. Cell membrane
Phagocytosis
One important role of the macrophage is the removal of necrotic cellular debris in the lungs. Removing dead cell material is important in chronic inflammation as the early stages of inflammation are dominated by neutrophil granulocytes, which are ingested by macrophages if they come of age (see CD-31 for a description of this process.)
The removal of necrotic tissue is to a greater extent handled by fixed macrophages, which will stay at strategic locations such as the lungs, liver, neural tissue, bone, spleen and connective tissue, ingesting foreign materials such as pathogens, recruiting additional macrophages if needed.
When a macrophage ingests a pathogen, the pathogen becomes trapped in a phagosome, which then fuses with a lysosome. Within the phagolysosome, enzymes and toxic peroxides digest the pathogen. However, some bacteria, such as Mycobacterium tuberculosis, have become resistant to these methods of digestion. Macrophages can digest more than 100 bacteria before they finally die due to their own digestive compounds.
Role in specific immunity
Macrophages are versatile cells that play many roles. As scavengers, they rid the body of worn-out cells and other debris. They are foremost among the cells that "present" antigen; a crucial role in initiating an immune response. As secretory cells, monocytes and macrophages are vital to the regulation of immune responses and the development of inflammation; they produce an amazing array of powerful chemical substances (monokines) including enzymes, complement proteins, and regulatory factors such as interleukin-1. At the same time, they carry receptors for lymphokines that allow them to be "activated" into single-minded pursuit of microbes and tumour cells.
After digesting a pathogen, a macrophage will present the antigen (a molecule, most often a protein found on the surface of the pathogen, used by the immune system for identification) of the pathogen to the corresponding helper T cell. The presentation is done by integrating it into the cell membrane and displaying it attached to a MHC class II molecule, indicating to other white blood cells that the macrophage is not a pathogen, despite having antigens on its surface.
Eventually the antigen presentation results in the production of antibodies that attach to the antigens of pathogens, making them easier for macrophages to adhere to with their cell membrane and phagocytose. In some cases, pathogens are very resistant to adhesion by the macrophages. Coating an antigen with antibodies could be compared to coating something with Velcro to make it stick to fuzzy surfaces.
The antigen presentation on the surface of infected macrophages (in the context of MHC class II) in a lymph node stimulates TH1 (type 1 helper T cells) to proliferate (mainly due to IL-12 secretion from the macrophage). When a B-cell in the lymph node recognizes the same unprocessed surface antigen on the bacterium with its surface bound antibody, the antigen is endocytosed and processed. The processed antigen is then presented in MHCII on the surface of the B-cell. TH1 receptor that has proliferated recognizes the antigen-MHCII complex (with co-stimulatory factors- CD40 and CD40L) and causes the B-cell to produce antibodies that help opsonisation of the antigen so that the bacteria can be better cleared by phagocytes.
Macrophages provide yet another line of defense against tumor cells and somatic cells infected with fungus or parasites. Once a T cell has recognized its particular antigen on the surface of an aberrant cell, the T cell becomes an activated effector cell, chemical mediators known as lymphokines that stimulate macrophages into a more aggressive form. These activated macrophages can then engulf and digest affected cells much more readily.[2] The macrophage does not generate a response specific for an antigen, but attacks the cells present in the local area in which it was activated.[2]
Fixed macrophages
A majority of macrophages are stationed at strategic points where microbial invasion or accumulation of dust is likely to occur. Each type of macrophage, determined by its location, has a specific name:
| Name of cell | Location |
| Dust cells/Alveolar macrophages | pulmonary alveolus of lungs |
| Histiocytes | connective tissue |
| Kupffer cells | liver |
| Microglia | neural tissue |
| Epithelioid cells | granulomas |
| Osteoclasts | bone |
| Sinusoidal lining cells | spleen |
| Mesangial cells | kidney |
Investigations concerning Kupffer cells are hampered because in humans Kupffer cells are only accessible for immunohistochemical analysis from biopsies or autopsies. From rats and mice they are difficult to isolate and after purification only approximately 5 million cells can be obtained from one mouse.
Macrophages can express paracrine functions within organs that are specific to the function of that organ. In the testis for example, macrophages have been shown to be able to interact with Leydig cells by secreting 25-hydroxycholesterol, an oxysterol that can be converted to testosterone by neighbouring Leydig cells. Also, testicular macrophages may participate in creating an immune privileged environment in the testis, and in mediating infertility during inflammation of the testis.
Involvement in symptoms of diseases
Due to their role in phagocytosis, macrophages are involved in many diseases of the immune system. For example, they participate in the formation of granulomas, inflammatory lesions that may be caused by a large number of diseases.
Some disorders, mostly rare, of ineffective phagocytosis and macrophage function have been described.
Macrophages are the predominant cells involved in creating the progressive plaque lesions of atherosclerosis. [3]
Macrophages also play a role in Human Immunodeficiency Virus (HIV) infection. Like T cells, macrophages can be infected with HIV, and even become a reservoir of ongoing virus replication throughout the body.
Macrophages are believed to help cancer cells proliferate as well. They are attracted to oxygen-starved (hypoxic) tumour cells and promote chronic inflammation. Inflammatory compounds such as Tumor necrosis factor (TNF) released by the macrophage activates the gene switch nuclear factor-kappa B. NF-kB then enters the nucleus of a tumour cell and turns on production of proteins that stop apoptosis and promote cell proliferation and inflammation. [4]
Media
Related cells
- Tingible body macrophages are found in the germinal centers of lymph nodes.
- Dendritic cells (including Langerhans cells).
- A lipid-laden macrophage is called a foam cell.
- A Multinucleated giant cells is a type of a macrophage seen in certain types of inflammatory diseases such as Mycoplasmal infections.
References
- ↑ Krombach F, Münzing S, Allmeling AM, Gerlach JT, Behr J, Dörger M (September 1997). "Cell size of alveolar macrophages: an interspecies comparison". Environ. Health Perspect. 105 Suppl 5: 1261–3. PMID 9400735.
- ↑ 2.0 2.1 "The human immune system: The lymphocyte story". New Scientist (1605): 1. March 1988. http://www.newscientist.com/channel/health/hiv/mg11716050.100. Retrieved on 2007-09-13.
- ↑ Lucas AD, Greaves DR (November 2001). "Atherosclerosis: role of chemokines and macrophages". Expert Rev Mol Med 3 (25): 1–18. doi:. PMID 14585150.
- ↑ Gary Stix (July 2007). "A Malignant Flame". Scientific American: 46–9. http://www.sciam.com/article.cfm?id=a-malignant-flame.
See also
- Oxoferin or WF 10 (TCDO)
- Immunomodulator
External links
- HIV and the Macrophage A book on the role of macrophages in AIDS pathogenesis
- Histology at BU 00704loa
- The role of macrophages in HIV pathogenesis
|
||||||||||||||