Methicillin-resistant Staphylococcus aureus
| Methicillin-resistant Staphylococcus aureus | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
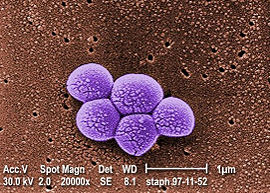
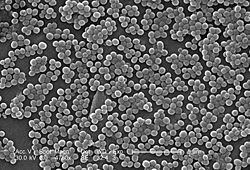 Electron micrograph of MRSA
|
||||||||||||||||
| Scientific classification | ||||||||||||||||
|
||||||||||||||||
| Binomial name | ||||||||||||||||
| Staphylococcus aureus Rosenbach 1884 |
Methicillin-resistant Staphylococcus aureus (MRSA, often pronounced "mersa") is a bacterium responsible for difficult-to-treat infections in humans. It may also be referred to as multiple-resistant Staphylococcus aureus or oxacillin-resistant Staphylococcus aureus (ORSA). MRSA is by definition a strain of Staphylococcus aureus that is resistant to a large group of antibiotics called the beta-lactams, which include the penicillins and the cephalosporins.
The organism is often sub-categorized as Community-Associated MRSA (CA-MRSA) or Health Care-Associated MRSA (HA-MRSA) although this distinction is complex. Some have defined CA-MRSA by criteria related to patients suffering from an MRSA infection while other authors have defined CA-MRSA by genetic characteristics of the bacteria themselves. CA-MRSA strains were first reported in the late 1990s; these cases were defined by a lack of exposure to the health care setting. In the next several years, it became clear that CA-MRSA infections were caused by strains of MRSA that differed from the older and better studied healthcare-associated strains.[1] The new CA-MRSA strains have rapidly spread in the United States to become the most common cause of cultured skin infections among individuals seeking medical care for these infections at emergency rooms in cities. These strains also commonly cause skin infections in athletes, jail and prison detainees, and soldiers.
MRSA is a resistant variation of the common bacterium Staphylococcus aureus. It has evolved an ability to survive treatment with beta-lactamase resistant beta-lactam antibiotics, including methicillin, dicloxacillin, nafcillin, and oxacillin. MRSA is especially troublesome in hospital-associated (nosocomial) infections. In hospitals, patients with open wounds, invasive devices, and weakened immune systems are at greater risk for infection than the general public. Hospital staff who do not follow proper sanitary procedures may transfer bacteria from patient to patient. Visitors to patients with MRSA infections or MRSA colonization are advised to follow hospital isolation protocol by using the provided gloves, gowns, and masks if indicated. Visitors who do not follow such protocols are capable of spreading the bacteria to cafeterias, bathrooms, and elevators.
Contents |
Discovery and history
MRSA/Methicillin Resistant Staphylococcus aureus was discovered in 1961 in the United Kingdom.It made its first major appearance in the United States in 1981 becoming prevalent among intravenous drug users. MRSA is often referred to in the press as a "superbug."
In the past decade or so the number of MRSA infections in the United States has increased significantly. A 2007 report in Emerging Infectious Diseases, a publication of the Centers for Disease Control and Prevention (CDC), estimated that the number of MRSA infections treated in hospitals doubled nationwide, from approximately 127,000 in 1999 to 278,000 in 2005, while at the same time deaths increased from 11,000 to more than 17,000.[2] Another study led by the CDC and published in the October 17, 2007 issue of the Journal of the American Medical Association estimated that MRSA would have been responsible for 94,360 serious infections and associated with 18,650 hospital stay-related deaths in the United States in 2005.[3][4] These figures suggest that MRSA infections are responsible for more deaths in the U.S. each year than AIDS.[5]
The UK Office for National Statistics reported 1,629 MRSA-related deaths in England and Wales during 2005, indicating a MRSA-related mortality rate half the rate of that in the United States for 2005, even though the figures from the British source were explained to be high because of "improved levels of reporting, possibly brought about by the continued high public profile of the disease"[6] during the time of the 2005 United Kingdom General Election. MRSA is thought to have caused 1,652 deaths in 2006 in UK up from 51 in 1993.[7]
It has been argued that the observed increased mortality among MRSA-infected patients may be the result of the increased underlying morbidity of these patients. Several studies, however, including one by Blot and colleagues, that have adjusted for underlying disease still found MRSA bacteremia to have a higher attributable mortality than methicillin-susceptible Staphylococcus aureus (MSSA) bacteremia.[8]
While the statistics suggest a national epidemic growing out of control, it has been difficult to quantify the degree of morbidity and mortality attributable to MRSA. A population-based study of the incidence of MRSA infections in San Francisco during 2004-5 demonstrated that nearly 1 in 300 residents suffered from such an infection in the course of a year and that greater than 85% of these infections occurred outside of the health care setting.[9] A 2004 study showed that patients in the United States with S. aureus infection had, on average, three times the length of hospital stay (14.3 vs. 4.5 days), incurred three times the total cost ($48,824 vs $14,141), and experienced five times the risk of in-hospital death (11.2% vs 2.3%) than patients without this infection.[10] In a meta-analysis of 31 studies, Cosgrove et al,[11] concluded that MRSA bacteremia is associated with increased mortality as compared with MSSA bacteremia (odds ratio = 1.93; 95% CI = 1.93±0.39).[12] In addition, Wyllie et al. report a death rate of 34% within 30 days among patients infected with MRSA, a rate similar to the death rate of 27% seen among MSSA-infected patients.[13]
Clinical presentation and concerns
S. aureus most commonly colonizes the anterior nares (the nostrils), although the respiratory tract, opened wounds, intravenous catheters, and urinary tract are also potential sites for infection. Healthy individuals may carry MRSA asymptomatically for periods ranging from a few weeks to many years. Patients with compromised immune systems are at a significantly greater risk of symptomatic secondary infection.
MRSA can be detected by swabbing the nostrils of patients and isolating the bacteria found inside. Combined with extra sanitary measures for those in contact with infected patients, screening patients admitted to hospitals has been found to be effective in minimizing the spread of MRSA at the Veterans Affairs hospital in Pittsburgh[14] and in hospitals in Denmark, Finland, and the Netherlands.[15]
The initial presentation of MRSA is small red bumps that resemble pimples, spider bites, or boils that may be accompanied by fever and occasionally rashes. Within a few days the bumps become larger, painful and eventually open into deep, pus-filled boils.[16] About 75 percent of CA-MRSA infections are localized to skin and soft tissue and usually can be treated effectively; however CA-MRSA strains display enhanced virulence, spreading more rapidly and causing illness much more severe than traditional HA-MRSA infections, and they can affect vital organs and lead to widespread infection (sepsis), toxic shock syndrome and necrotizing ("flesh-eating") pneumonia. This is thought to be due to toxins carried by CA-MRSA strains, such as PVL and PSM. It is not known why some healthy people develop CA-MRSA skin infections that are treatable whereas others infected with the same strain develop severe infections or die.[17]
CA-MRSA often results in abscess formation that requires incision and drainage. Before the spread of MRSA into the community, abscesses were not considered contagious because it was assumed that infection required violation of skin integrity and the introduction of staphylococci from normal skin colonization. However, newly emerging CA-MRSA is transmissible (similar, but with very important differences) from Hospital-Associated MRSA. CA-MRSA is less likely than other forms of MRSA to cause cellulitis.
Both CA-MRSA and HA-MRSA are resistant to traditional anti-staphylococcal beta-lactam antibiotics, such as cephalexin. CA-MRSA has a greater spectrum of antimicrobial susceptibility, including to sulfa drugs, tetracyclines, and clindamycin. HA-MRSA is resistant even to these antibiotics and often is susceptible only to vancomycin. Newer drugs, such as linezolid (belonging to the newer oxazolidinones class), may be effective against both CA-MRSA and HA-MRSA.
Vancomycin and teicoplanin are glycopeptide antibiotics used to treat MRSA infections.[18] Teicoplanin is a structural congener of vancomycin that has a similar activity spectrum but a longer half-life (t½).[19] Because the oral absorption of vancomycin and teicoplanin is very low, these agents must be administered intravenously to control systemic infections.[20] Treatment of MRSA infection with vancomycin can be complicated, due to its inconvenient route of administration. Moreover, many clinicians believe that the efficacy of vancomycin against MRSA is inferior to that of anti-staphylococcal beta-lactam antibiotics against MSSA.[21][22]
Several newly discovered strains of MRSA show antibiotic resistance even to vancomycin and teicoplanin. These new evolutions of the MRSA bacterium have been dubbed vancomycin intermediate-resistant Staphylococcus aureus (VISA).[23][24] Linezolid, quinupristin/dalfopristin, daptomycin, and tigecycline are used to treat more severe infections that do not respond to glycopeptides such as vancomycin.[25] MRSA infections can be treated with oral agents, including linezolid, rifampicin+fusidic acid, rifampicin+fluoroquinolone, pristinamycin, co-trimoxazole (trimethoprim-sulfamethoxazole), doxycycline or minocycline, and clindamycin.[26]
On May 18, 2006, a report in Nature identified a new antibiotic, called platensimycin, that had demonstrated successful use against MRSA.[27][28]
An entirely different and promising approach is phage therapy (e.g., at the Eliava Institute in Georgia[29]), which has a reported efficacy against up to 95% of tested Staphylococcus isolates.[30]
It has been reported that maggot therapy to treat MRSA infection has been successful. Studies in diabetic patients reported significantly shorter treatment times than those achieved with standard treatments.[31][32][33]
At-risk populations
At risk populations include:
- People with weak immune systems such as AIDS patients
- Athletes participating in contact sports
- Young Children
- The elderly
- Persons staying in a health care facility for an extended period of time
- Prisoners or anyone living in confined space with other people.
Inmates in prisons and Jails
In confined environments, like jails and prisons, with the rotating in and out of a new population that is typically in poor health, there have been a growing number of challenges reported first in the U.S. and then in Canada. The earliest reports were made by the U.S. Centers for Disease Control and Prevention (CDC) in state prisons. Subsequently reports of a massive rise in skin and soft tissue infections were reported by the CDC in the Los Angeles County Jail system in 2001, and this has continued. Pan et al. reported on the changing epidemiology of MRSA skin infection in the San Francisco County Jail, noting the MRSA accounted for >70% of S. aureus infection in the jail by 2002. Lowy and colleagues reported on frequent MRSA skin infections in New York State Prisons. Two reports on inmates in Maryland have demonstrated frequent colonization with MRSA. In the news media hundreds of reports of MRSA outbreaks in incarcerations facilities appeared between 2000 and 2008. For example, in February 2008, The Tulsa County Jail in the U.S. State of Oklahoma started treating an average of twelve Staphylococcus cases per month.[34] A report on skin and soft tissue infections in the Cook County Jail in Chicago in 2004-5 demonstrated that MRSA was the most common cause of these infections among cultured lesions and furthermore that few risk factors were more strongly associated with MRSA infections than infections caused by methicillin-susceptible S. aureus. In response to these and many other reports on MRSA infections among incarcerated and recently incarcerated persons, the Federal Bureau of Prisons has released Guidelines for the management and control of the infections although few studies provide an evidence base for these guidelines.
Cystic fibrosis patients
Cystic fibrosis patients are at particular risk for pulmonary colonization of MRSA, both because of their difficulty clearing mucus and their frequent hospital visits, which can increase exposure to MRSA. These factors substantially increase the rate of life-threatening MRSA pneumonia in this group. The risk of cross-colonization has led to the increased use of isolation protocols among these patients. In a hospital setting, patients who have received fluoroquinolones are more likely to become colonized with MRSA;[35] this is probably because many circulating strains of MRSA are fluoroquinolone resistant, which means that MRSA is able to colonize patients whose normal skin flora have been cleared of non-resistant S. aureus by fluoroquinolones.
Hospital patients
MRSA infections occur mostly in hospitals and healthcare facilities, with a higher incident rate in nursing homes or long-term care facilities. Healthcare provider to patient transfer is common, especially when healthcare providers move from patient to patient without performing necessary handwashing techniques between patients. However, it should be noted that MRSA can cause infections outside of hospitals as well.
Prevention and infection-control strategies
Screening programs
Patient screening upon hospital admission, with nasal cultures, prevents the cohabitation of MRSA carriers with non-carriers, and exposure to infected surfaces. In the United States and Canada, the Centers for Disease Control and Prevention issued guidelines on October 19, 2006, citing the need for additional research, but declined to recommend such screening.[36][37]
A report in the journal "Pediatrics" says 2.4% of healthy children may be carrying the staph infection "MRSA" in their nasal passage.[38]
Surface sanitizing


Alcohol has been proven to be an effective surface sanitizer against MRSA however as the alcohol evaporates it becomes less effective and is unable to actively protect surfaces from future contamination. Quaternary ammonium can be used in conjunction with alcohol to extend the longevity of the sanitizing action.[39] The prevention of nosocomial infections involves routine and terminal cleaning. Non-flammable Alcohol Vapor in Carbon Dioxide systems (NAV-CO2) do not corrode metals or plastics used in medical environments and do not contribute to antibacterial resistance.
In healthcare environments, MRSA can survive on surfaces and fabrics, including privacy curtains or garments worn by care providers. Complete surface sanitation is necessary to eliminate MRSA in areas where patients are recovering from invasive procedures. Testing patients for MRSA upon admission, isolating MRSA-positive patients, decolonization of MRSA-positive patients, and terminal cleaning of patients' rooms and all other clinical areas they occupy is the current best practice protocol for nosocomial MRSA.
Polysan (with TEFLEX) is a non-toxic, odourless, alcohol free, polymeric water-soluble disinfectant that is also effective as a surface sanitizer against MRSA. Unlike alcohol it drys on the surface and creates a polymer boundary that continuies to kill for up to seven days.
Hand washing
At the end of August 2004, after a successful pilot scheme to tackle MRSA, the UK National Health Service announced its Clean Your Hands campaign. Wards were required to ensure that alcohol-based hand rubs are placed near all beds so that staff can hand wash more regularly. It is thought that if this cuts infection by just 1%, the plan will pay for itself many times over.
Although alcohol-based rubs are somewhat effective, a more effective strategy is to wash hands with an anti-microbial cleanser with persistent killing action, such as Polysan or Chlorhexidine.
A June 2008 report, centered on a survey by the Association for Professionals in Infection Control and Epimedmiology, concluded that poor hygiene habits remain the principal barrier to significant reductions in the spread of MRSA.
Decolonization
After the drainage of boils or other treatment for MRSA, patients can shower at home using chlorhexidine (Hibiclens) or hexachlorophene (Phisohex) antiseptic soap from head to toe, and apply mupirocin (Bactroban) 2% ointment inside each nostril twice daily for 7 days, using a cotton-tipped swab. Doctors may also prescribe strong antibiotics such as clindamycin or levofloxacin. Household members are recommended to follow the same decolonization protocol.
More information
Mathematical models describe one way in which a loss of infection control can occur after measures for screening and isolation seem to be effective for years, as happened in the UK. In the "search and destroy" strategy that was employed by all UK hospitals until the mid 1990s, all patients with MRSA were immediately isolated, and all staff were screened for MRSA and were prevented from working until they had completed a course of eradication therapy that was proven to work. Loss of control occurs because colonised patients are discharged back into the community and then readmitted: when the number of colonised patients in the community reaches a certain threshold, the "search and destroy" strategy is overwhelmed.[40] One of the few countries not to have been overwhelmed by MRSA is the Netherlands: an important part of the success of the Dutch strategy may have been to attempt eradication of carriage upon discharge from hospital.[41]
Current US guidance does not require workers in general workplaces (not healthcare facilities) with MRSA infections to be routinely excluded from going to work.[42]
Unless directed by a healthcare provider, exclusion from work should be reserved for those with wound drainage that cannot be covered and contained with a clean, dry bandage and for those who cannot maintain good hygiene practices.[42] Workers with active infections should be excluded from activities where skin-to-skin contact is likely to occur until their infections are healed. Healthcare workers should follow the Centers for Disease Control and Prevention's Guidelines for Infection Control in Health Care Personnel.[43]
To prevent the spread of staph or MRSA in the workplace, employers should ensure the availability of adequate facilities and supplies that encourage workers to practice good hygiene; that surface sanitizing in the workplace is followed; and that contaminated equipment are sanitized with Environmental Protection Agency (EPA)-registered disinfectants.[42]
Reports reflect a nationwide epidemic of MRSA in the US — one that has significantly increased over the past seven years. A 2007 report in Emerging Infectious Diseases, a publication of the Centers for Disease Control and Prevention, estimated that the number of MRSA infections treated in hospitals doubled nationwide, from approximately 127,000 in 1999 to 278,000 in 2005, while at the same time deaths increased from 11,000 to more than 17,000.[2]
Worldwide, an estimated 2 billion people carry some form of S. aureus; of these, up to 53 million (2.7% of carriers) are thought to carry MRSA.[44] In the United States, 95 million carry S. aureus in their noses; of these, 2.5 million (2.6% of carriers) carry MRSA.[45] A population review conducted in three U.S. communities showed the annual incidence of CA-MRSA during 2001–2002 to be 18–25.7/100,000; most CA-MRSA isolates were associated with clinically relevant infections, and 23% of patients required hospitalization.[46]
In the United States, there have been increasing numbers of reports of outbreaks of MRSA colonization and infection through skin contact in locker rooms and gymnasiums, even among healthy populations. A study published in the New England Journal of Medicine[47] linked MRSA to the abrasions caused by artificial turf. Three studies by the Texas State Department of Health found that the infection rate among football players was 16 times the national average. In December 2007, a high school football player died from MRSA-infected turf burns.[48] MRSA has also been found in the public school systems throughout the country.[49]
MRSA is also becoming a problem in pediatric settings,[50] including hospital nurseries.[51] A 2007 study found that 4.6% of patients in U.S. health care facilities were infected or colonized with MRSA.[52] One 2008 study concluded that men living in predominately gay ZIP codes in San Francisco are 13 times more likely to be infected by one strain of MRSA than their heterosexual neighbors.[53]
MRSA progresses substantially within 24-48 hours of initial topical symptoms. After 72 hours, MRSA can take hold of human tissue and become resistant to treatment. MRSA causes as many as 20% of Staphylococcus aureus infections in populations that use intravenous drugs. These out-of-hospital strains, or CA-MRSA, are more easily treated, though more virulent, than HA-MRSA. CA-MRSA apparently did not evolve de novo in the community but represents a hybrid between MRSA that spread from the hospital environment and strains that were once easily treatable in the community. Most of the hybrid strains also acquired a factor that increases their virulence, resulting in the development of deep-tissue infections from minor scrapes and cuts, as well as many cases of fatal pneumonia.[54]
As of early 2005, the number of deaths in the United Kingdom attributed to MRSA has been estimated by various sources to lie in the area of 3,000 per year.[55] Staphylococcus bacteria account for almost half of all UK hospital infections. The issue of MRSA infections in hospitals has recently been a major political issue in the UK, playing a significant role in the debates over health policy in the United Kingdom general election held in 2005.
On January 6, 2008, half of 64 non-Chinese cases of Methicillin-resistant Staphylococus aureus (MRSA) infections in Hong Kong in 2007 were Filipino domestic helpers. Ho Pak-leung, professor of microbiology, University of Hong Kong traced the cause from high use of antibiotics. In 2007, there were 166 community cases in Hong Kong compared with 8,000 hospital-acquired MRSA (155 recorded cases — 91 involved Chinese locals, 33 Filipinos, 5 each for Americans and Indians, and 2 each from Nepal, Australia, Denmark and England).[56]
Strains
In the UK, the most common strains of MRSA are EMRSA15 and EMRSA16.[57] EMRSA16 is the best described epidemiologically; it originated in Kettering, England, and the full genomic sequence of this strain has been published.[58] EMRSA16 has been found to be identical to the ST36:USA200 strain, which circulates in the United States, and to carry the SCCmec type II, enterotoxin A and toxic shock syndrome toxin 1 genes.[59] Under the new international typing system, this strain is now called MRSA252. It is not entirely certain why this strain has become so successful, whereas previous strains have failed to persist. One explanation is the characteristic pattern of antibiotic susceptibility. Both the EMRSA15 and EMRSA16 strains are resistant to erythromycin and ciprofloxacin. It is known that Staphylococcus aureus can survive intracellularly,[60] and these are precisely the antibiotics that best penetrate intracellularly; it may be that these strains of S. aureus are therefore able to exploit an intracellular niche.
In the United States, most cases of CA-MRSA are caused by a CC8 strain designated ST8:USA300, which carries SCCmec type IV, Panton-Valentine leukocidin, PSM-alpha and enterotoxins Q and K,[59] and ST1:USA400.[61] Other community-associated strains of MRSA are ST8:USA500 and ST59:USA1000. In many nations of the world, MRSA strains with different predominant genetic background types have come to predominate among CA-MRSA strains; USA300 easily tops the list in the U. S. and is becoming more common in Canada after its first appearance there in 2004. For example, in Australia ST93 strains are common, while in continental Europe ST80 strains predominate (Tristan et al., Emerging Infectious Diseases, 2006). In Taiwan, ST59 strains, some of which are resistant to many non-beta-lactam antibiotics, have arisen as common causes of skin and soft tissue infections in the community. In a remote region of Alaska, unlike most of the continental U. S., USA300 was found rarely in a study of MRSA strains from outbreaks in 1996 and 2000 as well as in surveillance from 2004-6 (David et al., Emerg Infect Dis 2008).
Laboratory diagnosis

Diagnostic microbiology laboratories and reference laboratories are key for identifying outbreaks of MRSA. New rapid techniques for the identification and characterization of MRSA have been developed. These techniques include Real-time PCR and Quantitative PCR and are increasingly being employed in clinical laboratories for the rapid detection and identification of MRSA strains.[62][63]
See also
- Contamination control
- Antibiotic resistance
- Drug resistance
- Drug resistant diseases
- Vancomycin-resistant Staphylococcus aureus
- MDR-TB
- XDR-TB
- Vancomycin-resistant enterococcus (VRE)
- Clostridium difficile (CDF)
References
- ↑ Okuma K, Iwakawa K, Turnidge J, et al (2002). "Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community". J Clin Microbiol 40 (11): 4289–94. doi:. PMID 12409412.
- ↑ 2.0 2.1 Klein E, Smith DL, Laxminarayan R (2007). "Hospitalizations and Deaths Caused by Methicillin-Resistant Staphylococcus aureus, United States, 1999–2005". Emerg Infect Dis 13 (12): 1840–6.
- ↑ Klevens et al (2007), "Invasive Methicillin-Resistant Staphylococcus aureus Infections in the United States". JAMA. Retrieved on 2007-10-31.
- ↑ Centers for Disease Control and Prevention (October 17, 2007), "MRSA: Methicillin-resistant Staphylococcus aureus in Healthcare Settings
- ↑ Stein R (October 17, 2007), "Drug-resistant staph germ's toll is higher than thought". Washington Post. Retrieved on 2007-10-19.
- ↑ UK Office for National Statistics Online (February 22, 2007), "MRSA Deaths continue to rise in 2005"
- ↑ Hospitals struck by new killer bugAn article by Manchester free newspaper 'Metro', May 7, 2008
- ↑ Blot S, Vandewoude K, Hoste E, Colardyn F (2002). "Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus". Arch Intern Med 162 (19): 2229–35. doi:. PMID 12390067.
- ↑ Liu et al., A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004-2005. Clin Infect Dis. 2008 Jun 1;46(11):1637-46)
- ↑ Noskin GA, Rubin RJ,Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, Lapetina E, Gemmen E (2005). "The Burden of Staphylococcus aureus Infections on Hospitals in the United States: An Analysis of the 2000 and 2001 Nationwide Inpatient Sample Database". Arch Intern Med 165: 1756–1761. doi:. PMID 16087824.
- ↑ Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y (2005). "The impact of Methicillin Resistance in Staphylococcus aureus Bacteremia on Patient Outcomes: Mortality, Length of Stay, and Hospital Charges" (– Scholar search). Infection Control and Hospital Epidemiology 26: 166–174. doi:. http://www.journals.uchicago.edu/ICHE/journal/issues/v26n2/9885/9885.html.
- ↑ Hardy KJ, Hawkey PM, Gao F, Oppenheim BA (2004). "Methicillin resistant Staphylococcus aureus in the critically ill". British Journal of Anaesthesia 92: 121–30. doi:. PMID 14665563.
- ↑ Wyllie D, Crook D, Peto T (2006). "Mortality after Staphylococcus aureus bacteraemia in two hospitals in Oxfordshire, 1997–2003: cohort study". BMJ 333 (7562): 281. doi:. PMID 16798756. http://bmj.bmjjournals.com/cgi/content/abstract/333/7562/281.
- ↑ "Science Daily".
- ↑ McCaughey B (PDF), Unnecessary Deaths: The Human and Financial Costs of Hospital Infections (2nd. ed.), http://www.tufts.edu/med/apua/Patients/ridbooklet.pdf, retrieved on 2007-08-05
- ↑ "Symptoms". Mayo Clinic.
- ↑ "MRSA Toxin Acquitted: Study Clears Suspected Key to Severe Bacterial Illness". NIH news release. National Institute of Health (2006-11-06).
- ↑ Schentag JJ, Hyatt JM, Carr JR, Paladino JA, Birmingham MC, Zimmer GS, Cumbo TJ (1998). "Genesis of methicillin-resistant Staphylococcus aureus (MRSA), how treatment of MRSA infections has selected for vancomycin-resistant Enterococcus faecium, and the importance of antibiotic management and infection control". Clin. Infect. Dis. 26 (5): 1204–14. doi:. PMID 9597254.
- ↑ Rybak MJ, Lerner SA, Levine DP, Albrecht LM, McNeil PL, Thompson GA, Kenny MT, Yuh L (1991). "Teicoplanin pharmacokinetics in intravenous drug abusers being treated for bacterial endocarditis". Antimicrob. Agents Chemother. 35 (4): 696–700. PMID 1829880.
- ↑ Janknegt R (1997). "The treatment of staphylococcal infections with special reference to pharmacokinetic, pharmacodynamic, and pharmacoeconomic considerations". Pharmacy world & science : PWS 19 (3): 133–41. doi:. PMID 9259029.
- ↑ Chang FY, Peacock JE Jr, Musher DM, et al. (2003). "Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study.". Medicine (Baltimore) 82 (5): 333–9. doi:. PMID 14530782.
- ↑ Siegman-Igra Y, Reich P, Orni-Wasserlauf R, Schwartz D, Giladi M. (2005). "The role of vancomycin in the persistence or recurrence of Staphylococcus aureus bacteraemia". Scand J Infect Dis 37 (8): 572–8. doi:. PMID 16138425.
- ↑ Sieradzki K, Tomasz A (1997). "Inhibition of cell wall turnover and autolysis by vancomycin in a highly vancomycin-resistant mutant of Staphylococcus aureus". J. Bacteriol. 179 (8): 2557–66. PMID 9098053.
- ↑ Schito GC (2006). "The importance of the development of antibiotic resistance in Staphylococcus aureus". Clin Microbiol Infect 12 Suppl 1: 3–8. PMID 16445718}.
- ↑ Mongkolrattanothai K, Boyle S, Kahana MD, Daum RS (2003). "Severe Staphylococcus aureus infections caused by clonally related community-associated methicillin-susceptible and methicillin-resistant isolates". Clin. Infect. Dis. 37 (8): 1050–8. doi:. PMID 14523769.
- ↑ Birmingham MC, Rayner CR, Meagher AK, Flavin SM, Batts DH, Schentag JJ (2003). "Linezolid for the treatment of multidrug-resistant, gram-positive infections: experience from a compassionate-use program". Clin. Infect. Dis. 36 (2): 159–68. doi:. PMID 12522747.
- ↑ Bayston R, Ashraf W, Smith T (2007). "Triclosan resistance in methicillin-resistant Staphylococcus aureus expressed as small colony variants: a novel mode of evasion of susceptibility to antiseptics". J. Antimicrob. Chemother. 59 (5): 848–53. doi:. PMID 17337510.
- ↑ Wang J (May 2006). "Platensimycin is a selective FabF inhibitor with potent antibiotic properties". Nature (441): 358–361. PMID 16710421}.
- ↑ "'Red Army' virus to combat MRSA", BBC News (2007-08-13).
- ↑ Matsuzaki S, Yasuda M, Nishikawa H, Kuroda M, Ujihara T, Shuin T, Shen Y, Jin Z, Fujimoto S, Nasimuzzaman MD, Wakiguchi H, Sugihara S, Sugiura T, Koda S, Muraoka A, Imai S (2003). "Experimental protection of mice against lethal Staphylococcus aureus infection by novel bacteriophage phi MR11". J. Infect. Dis. 187 (4): 613–24. doi:. PMID 12599078.
- ↑ Bowling FL, Salgami EV, Boulton AJ (2007). "Larval therapy: a novel treatment in eliminating methicillin-resistant Staphylococcus aureus from diabetic foot ulcers". Diabetes Care 30 (2): 370–1. doi:. PMID 17259512.
- ↑ "Maggots help cure MRSA patients", BBC News (2007-05-02).
- ↑ "Maggots rid patients of MRSA", EurekAlert!/AAAS (2007-05-03).
- ↑ Ann Coppola, Super-scary superbugs, The Corrections Connection Network News
- ↑ Charbonneau P, Parienti J, Thibon P, Ramakers M, Daubin C, du Cheyron D, Lebouvier G, Le Coutour X, Leclercq R (2006). "Fluoroquinolone use and methicillin-resistant Staphylococcus aureus isolation rates in hospitalized patients: a quasi experimental study". Clin Infect Dis 42 (6): 778–84. doi:. PMID 16477553.
- ↑ "To Catch a Deadly Germ," New York Times opinion
- ↑ CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- ↑ Prevalence of and Risk Factors for Community-Acquired Methicillin-Resistant and Methicillin-Sensitive Staphylococcus aureus Colonization in Children Seen in a Practice-Based R...
- ↑ Angela L. Hollingsworth (PDF), AOAC Use Dilution Test Health Care, http://www.sanisys.com/pdf_epa_salmo.pdf, retrieved on 2003-09-26
- ↑ Cooper BS, Medley GF, Stone SP, et al. (2004). "Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes". Proceedings of the National Academy of Sciences 101 (27): 10223–8. doi:. PMID 15220470.
- ↑ Bootsma MC, Diekmann O, Bonten MJ (2006). "Controlling methicillin-resistant Staphylococcus aureus: quantifying the effects of interventions and rapid diagnostic testing". Proc Natl Acad Sci USA 103 (14): 5620–5. doi:. PMID 16565219.
- ↑ 42.0 42.1 42.2 "NIOSH MRSA and the Workplace". United States National Institute for Occupational Safety and Health. Retrieved on 2007-10-29.
- ↑ CDC (1998). "Guidelines for Infection Control in Health Care Personnel, 1998". Centers for Disease Control and Prevention. Retrieved on December 18, 2007.
- ↑ "MRSA Infections". Keep Kids Healthy.
- ↑ Graham P, Lin S, Larson E (2006). "A U.S. population-based survey of Staphylococcus aureus colonization". Ann Intern Med 144 (5): 318–25. PMID 16520472.
- ↑ Jernigan JA, Arnold K, Heilpern K, Kainer M, Woods C, Hughes JM (2006-05-12). "Methicillin-resistant Staphylococcus aureus as community pathogen". Symposium on Community-Associated Methicillin-resistant Staphylococcus aureus (Atlanta, Georgia, USA). Cited in Emerg Infect Dis, Centers for Disease Control and Prevention. Retrieved on 2007-01-27.
- ↑ "New England Journal of Medicine".
- ↑ "Bloomberg".
- ↑ "SVSD410".
- ↑ MRSA: the problem reaches paediatrics — Archives of Disease in Childhood
- ↑ Community-associated Methicillin-resistant Staphylococcus aureus in Hospital Nursery and Maternity Units — CDC
- ↑ Association for Professionals in Infection Control & Epidemiology (June 25, 2007). "National Prevalence Study of Methicillin-Resistant Staphylococcus aureus (MRSA) in U.S. Healthcare Facilities". Retrieved on 2007-07-14.
- ↑ Diep BA, et al "Emergence of multidrug-resistant, community-associated methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men." Ann Intern Med. 2008; 148:249–257.
- ↑ "Community-Associated meticillin-resistant Staphylococcusaureus: an emerging threat" (PDF). The Lancet.
- ↑ Johnson AP, Pearson A, Duckworth G (2005). "Surveillance and epidemiology of MRSA bacteraemia in the UK". J Antimicrob Chemother 56 (3): 455–62. doi:. PMID 16046464.
- ↑ Inquirer.net, Cases of RP maids with ‘superbug’ infection growing in HK
- ↑ Johnson AP, Aucken HM, Cavendish S, et al. (2001). "Dominance of EMRSA-15 and -16 among MRSA causing nosocomial bacteraemia in the UK: analysis of isolates from the European Antimicrobial Resistance Surveillance System (EARSS)". J Antimicrob Chemother 48 (1): 143–4. doi:. PMID 11418528. http://jac.oxfordjournals.org/cgi/content/full/48/1/143.
- ↑ Holden MTG, Feil EJ, Lindsay JA, et al. (2004). "Complete genomes of two clinical Staphylococcus aureus strains: Evidence for the rapid evolution of virulence and drug resistance". Proc Natl Acad Sci U S A 101: 9786–91. doi:. PMID 15213324.
- ↑ 59.0 59.1 Diep B, Carleton H, Chang R, Sensabaugh G, Perdreau-Remington F (2006). "Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus". J Infect Dis 193 (11): 1495–503. doi:. PMID 16652276.
- ↑ von Eiff C, Becker K, Metze D, et al. (2001). "Intracellular persistence of Staphylococcus aureus small-colony variants within keratinocytes: a cause for antibiotic treatment failure in a patient with Darier's disease". Clin Infect Dis 32 (11): 1643–7. doi:. PMID 11340539.
- ↑ R Wang et al. "Identification of novel cytolytic peptides as key virulence determinants of community-associated MRSA". Nature Medicine DOI: 10.1038/nm1656 (2007).
- ↑ "Rapid Diagnosis and Typing of Staphylococcus aureus". Staphylococcus: Molecular Genetics. Caister Academic Press. 2008. ISBN 978-1-904455-29-5.
- ↑ Mackay IM (editor). (2007). Real-Time PCR in Microbiology: From Diagnosis to Characterization. Caister Academic Press. ISBN 978-1-904455-18-9. http://www.horizonpress.com/rtmic.
External links
- BURDEN of Resistance and Disease in European Nations - An EU-Project to estimate the financial burden of antibiotic resistance in European Hospitals.
- Information and recent articles about MRSA.
- Mayo recommends prevention through proper hand-washing technique
- CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- Questions and Answers about sanitizing methods
- CDC Article on Hospital Associated MRSA
- CDC Article on Community Associated MRSA
- National Institute for Occupational Safety and Health — MRSA and the Workplace
- Clinical images of MRSA and associated diseases