Leukemia
| Leukaemia Classification and external resources |
|
 |
|
|---|---|
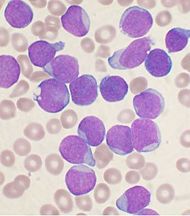
| A Wright's stained bone marrow aspirate smear of patient with precursor B-cell acute lymphoblastic leukemia. | |
| ICD-10 | C91.-C95. |
| ICD-9 | 208.9 |
| ICD-O: | 9800-9940 |
| DiseasesDB | 7431 |
| MeSH | D007938 |
Leukemia or leukaemia (Greek leukos λευκός, "white"; aima αίμα, "blood") is a cancer of the blood or bone marrow and is characterized by an abnormal proliferation (production by multiplication) of blood cells, usually white blood cells (leukocytes). Leukemia is a broad term covering a spectrum of diseases. In turn, it is part of the even broader group of diseases called hematological neoplasms.
Contents |
Classification
Leukemia is clinically and pathologically subdivided into several large groups. The first division is between its acute and chronic forms:
- Acute leukemia is characterized by the rapid increase of immature blood cells. This crowding makes the bone marrow unable to produce healthy blood cells. Acute forms of leukemia can occur in children and young adults. (In fact, it is a more common cause of death for children in the US than any other type of malignant disease). Immediate treatment is required in acute leukemias due to the rapid progression and accumulation of the malignant cells, which then spill over into the bloodstream and spread to other organs of the body. Central nervous system (CNS) involvement is uncommon, although the disease can occasionally cause cranial nerve palsies.
- Chronic leukemia is distinguished by the excessive build up of relatively mature, but still abnormal, blood cells. Typically taking months or years to progress, the cells are produced at a much higher rate than normal cells, resulting in many abnormal white blood cells in the blood. Chronic leukemia mostly occurs in older people, but can theoretically occur in any age group. Whereas acute leukemia must be treated immediately, chronic forms are sometimes monitored for some time before treatment to ensure maximum effectiveness of therapy.
Additionally, the diseases are subdivided according to which kind of blood cell is affected. This split divides leukemias into lymphoblastic or lymphocytic leukemias and myeloid or myelogenous leukemias:
- In lymphoblastic or lymphocytic leukemias, the cancerous change takes place in a type of marrow cell that normally goes on to form lymphocytes.
- In myeloid or myelogenous leukemias, the cancerous change takes place in a type of marrow cell that normally goes on to form red cells, some types of white cells, and platelets.
Combining these two classifications provides a total of four main categories:
| Cell type | Acute | Chronic |
|---|---|---|
| Lymphocytic leukemia (or "lymphoblastic") |
Acute lymphoblastic leukemia (ALL) | Chronic lymphocytic leukemia (CLL) |
| Myelogenous leukemia (also "myeloid" or "nonlymphocytic") |
Acute myelogenous leukemia (AML) | Chronic myelogenous leukemia (CML) |
Within these main categories, there are typically several subcategories. Finally, hairy cell leukemia is usually considered to be outside of this classification scheme.
- Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in young children. This disease also affects adults, especially those age 65 and older. Standard treatments involve chemotherapy and radiation. The survival rates vary by age: 85% in children and 50% in adults.[1]
- Chronic lymphocytic leukemia (CLL) most often affects adults over the age of 55. It sometimes occurs in younger adults, but it almost never affects children. Two-thirds of affected people are men. The five-year survival rate is 75%.[2] It is incurable, but there are many effective treatments.
- Acute myelogenous leukemia (AML) occurs more commonly in adults than in children, and more commonly in men than women. AML is treated with chemotherapy. The five-year survival rate is 40%.[3]
- Chronic myelogenous leukemia (CML) occurs mainly in adults. A very small number of children also develop this disease. Treatment is with imatinib (Gleevec) or other drugs. The five-year survival rate is 90%.[4][5]
- Hairy cell leukemia (HCL) is sometimes considered a subset of CLL, but does not fit neatly into this pattern. About 80% of affected people are adult men. There are no reported cases in young children. HCL is incurable, but easily treatable. Survival is 96% to 100% at ten years.[6]
Symptoms
Damage to the bone marrow, by way of displacing the normal bone marrow cells with higher numbers of immature white blood cells, results in a lack of blood platelets, which are important in the blood clotting process. This means people with leukemia may become bruised, bleed excessively, or develop pinprick bleeds (petechiae).
White blood cells, which are involved in fighting pathogens, may be suppressed or dysfunctional. This could cause the patient's immune system to be unable to fight off a simple infection or to start attacking other body cells.
Finally, the red blood cell deficiency leads to anemia, which may cause dyspnea. All symptoms can be attributed to other diseases.
Some other related symptoms:
The word leukemia, which means 'white blood', is derived from the disease's namesake high white blood cell counts that most leukemia patients have before treatment. The high number of white blood cells are apparent when a blood sample is viewed under a microscope. Frequently, these extra white blood cells are immature or dysfunctional. The excessive number of cells can also interfere with the level of other cells, causing a harmful imbalance in the blood count.
Some leukemia patients do not have high white blood cell counts visible during a regular blood count. This less-common condition is called aleukemia. The bone marrow still contains cancerous white blood cells which disrupt the normal production of blood cells. However, the leukemic cells are staying in the marrow instead of entering the bloodstream, where they would be visible in a blood test. For an aleukemic patient, the white blood cell counts in the bloodstream can be normal or low. Aleukemia can occur in any of the four major types of leukemia, and is particularly common in hairy cell leukemia.
Numbers
Nearly 44,000 people are diagnosed with leukemia every year in the United States, with an average of 22,000 deaths every year.
Causes and risk factors
There is no single known cause for all of the different types of leukemia. The different leukemias likely have different causes, and very little is certain about what causes them. Researchers have strong suspicions about four possible causes:
- natural or artificial ionizing radiation
- certain kinds of chemicals
- some viruses
- genetic predispositions
Leukemia, like other cancers, results from somatic mutations in the DNA which activate oncogenes or deactivate tumor suppressor genes, and disrupt the regulation of cell death, differentiation or division. These mutations may occur spontaneously or as a result of exposure to radiation or carcinogenic substances and are likely to be influenced by genetic factors. Cohort and case-control studies have linked exposure to petrochemicals, such as benzene, and hair dyes to the development of some forms of leukemia.
Viruses have also been linked to some forms of leukemia. For example, certain cases of ALL are associated with viral infections by either the human immunodeficiency virus or human T-lymphotropic virus (HTLV-1 and -2, causing adult T-cell leukemia/lymphoma). However, one report suggests exposure to certain germs may offer children limited protection against leukemia.
Fanconi anemia is also a risk factor for developing acute myelogenous leukemia.
Until the cause or causes of leukemia are found, there is no way to prevent the disease. Even when the causes become known, they may not be readily controllable, such as naturally occurring background radiation, and therefore not especially helpful for prevention purposes.
Treatment options for leukemia by type
Acute lymphoblastic leukemia (ALL)
- Further information: Acute lymphoblastic leukemia#Treatment
Management of ALL focuses on control of bone marrow and systemic (whole-body) disease. Additionally, treatment must prevent leukemic cells from spreading to other sites, particularly the central nervous system (CNS) e.g. monthly lumbar punctures. In general, ALL treatment is divided into several phases:
- Induction chemotherapy to bring about bone marrow remission. For adults, standard induction plans include prednisone, vincristine, and an anthracycline drug; other drug plans may include L-asparaginase or cyclophosphamide. For children with low-risk ALL, standard therapy usually consists of three drugs (prednisone, L-asparaginase, and vincristine) for the first month of treatment.
- Consolidation therapy or intensification therapy to eliminate any remaining leukemia cells. There are many different approaches to consolidation, but it is typically a high-dose, multi-drug treatment that is undertaken for a few months. Patients with low- to average-risk ALL receive therapy with antimetabolite drugs such as methotrexate and 6-mercaptopurine (6-MP). High-risk patients receive higher drug doses of these drugs, plus additional drugs.
- CNS prophylaxis (preventive therapy) to stop the cancer from spreading to the brain and nervous system in high-risk patients. Standard prophylaxis may include radiation of the head and/or drugs delivered directly into the spine.
- Maintenance treatments with chemotherapeutic drugs to prevent disease recurrence once remission has been achieved. Maintenance therapy usually involves lower drug doses, and may continue for up to three years.
- Alternatively, allogeneic bone marrow transplantation may be appropriate for high-risk or relapsed patients.
Chronic lymphocytic leukemia (CLL)
- Further information: Chronic lymphocytic leukemia#Treatment
Decision to treat
Hematologists base CLL treatment upon both the stage and symptoms of the individual patient. A large group of CLL patients have low-grade disease, which does not benefit from treatment. Individuals with CLL-related complications or more advanced disease often benefit from treatment. In general, the indications for treatment are:
- falling hemoglobin or platelet count
- progression to a later stage of disease
- painful, disease-related overgrowth of lymph nodes or spleen
- an increase in the rate of lymphocyte production
Typical treatment approach
CLL is probably incurable by present treatments. The primary chemotherapeutic plan is combination chemotherapy with chlorambucil or cyclophosphamide, plus a corticosteroid such as prednisone or prednisolone. The use of a corticosteroid has the additional benefit of suppressing some related autoimmune diseases, such as immunohemolytic anemia or immune-mediated thrombocytopenia. In resistant cases, single-agent treatments with nucleoside drugs such as fludarabine, pentostatin, or cladribine may be successful. Younger patients may consider allogeneic or autologous bone marrow transplantation.
Acute myelogenous leukemia (AML)
- Further information: Acute myeloid leukemia#Treatment
Many different anti-cancer drugs are effective for the treatment of AML. Treatments vary somewhat according to the age of the patient and according to the specific subtype of AML. Overall, the strategy is to control bone marrow and systemic (whole-body) disease, while offering specific treatment for the central nervous system (CNS), if involved.
In general, most oncologists rely on combinations of drugs for the initial, induction phase of chemotherapy. Such combination chemotherapy usually offers the benefits of early remission and a lower risk of disease resistance. Consolidation and maintenance treatments are intended to prevent disease recurrence. Consolidation treatment often entails a repetition of induction chemotherapy or the intensification chemotherapy with additional drugs. By contrast, maintenance treatment involves drug doses that are lower than those administered during the induction phase.
Chronic myelogenous leukemia (CML)
- Further information: Chronic myelogenous leukemia#Treatment
There are many possible treatments for CML, but the standard of care for newly diagnosed patients is imatinib (Gleevec) therapy.[7] Compared to most anti-cancer drugs, it has relatively few side effects and can be taken orally at home. With this drug, more than 90% of patients will be able to keep the disease in check for at least five years,[7] so that CML becomes a chronic, manageable condition.
In a more advanced, uncontrolled state, when the patient cannot tolerate imatinib, or if the patient wishes to attempt a permanent cure, then an allogeneic bone marrow transplantation may be performed. This procedure involves high-dose chemotherapy and radiation followed by infusion of bone marrow from a compatible donor. Approximately 30% of patients die from this procedure.[7]
Hairy cell leukemia (HCL)
- Further information: Hairy cell leukemia#Treatment
Decision to treat
Patients with hairy cell leukemia who are symptom-free typically do not receive immediate treatment. Treatment is generally considered necessary when the patient shows signs and symptoms such as low blood cell counts (e.g., infection-fighting neutrophil count below 1.0 K/µL), frequent infections, unexplained bruises, anemia, or fatigue that is significant enough to disrupt the patient's everyday life.
Typical treatment approach
Patients who need treatment usually receive either one week of cladribine, given daily by intravenous infusion or a simple injection under the skin, or six months of pentostatin, given every four weeks by intravenous infusion. In most cases, one round of treatment will produce a prolonged remission.
Other treatments include rituximab infusion or self-injection with Interferon-alpha. In limited cases, the patient may benefit from splenectomy (removal of the spleen). These treatments are not typically given as the first treatment because their success rates are lower than cladribine or pentostatin.
Research
Significant research into the causes, diagnosis, treatment, and prognosis of leukemia is being done. Hundreds of clinical trials are being planned or conducted at any given time. Studies may focus on effective means of treatment, better ways of treating the disease, improving the quality of life for patients, or appropriate care in remission or after cures.
Epidemiology
As of 1998, it is estimated that each year, approximately 30,800 individuals will be diagnosed with leukemia in the United States and 21,700 individuals will die of the disease.[8] This represents about 2% of all forms of cancer.
See also
- Antileukemic drugs
- Hematologic diseases
References
- ↑ Harrison's Principles of Internal Medicine, 16th Edition, Chapter 97. Malignancies of Lymphoid Cells. Clinical Features, Treatment, and Prognosis of Specific Lymphoid Malignancies.
- ↑ Finding Cancer Statistics » Cancer Stat Fact Sheets »Chronic Lymphocytic Leukemia National Cancer Institute
- ↑ Colvin GA, Elfenbein GJ (2003). "The latest treatment advances for acute myelogenous leukemia". Med Health R I 86 (8): 243–6. PMID 14582219.
- ↑ Patients with Chronic Myelogenous Leukemia Continue to Do Well on Imatinib at 5-Year Follow-Up Medscape Medical News 2006
- ↑ Updated Results of Tyrosine Kinase Inhibitors in CML ASCO 2006 Conference Summaries
- ↑ Else M, Ruchlemer R, Osuji N, et al (2005). "Long remissions in hairy cell leukemia with purine analogs: a report of 219 patients with a median follow-up of 12.5 years". Cancer 104 (11): 2442–8. doi:. PMID 16245328.
- ↑ 7.0 7.1 7.2 Fausel C (October 2007). "Targeted chronic myeloid leukemia therapy: seeking a cure". J Manag Care Pharm 13 (8 Suppl A): 8–12. PMID 17970609. http://www.amcp.org/data/jmcp/pages%208-12.pdf.
- ↑ "Trends in leukemia incidence and survival in the United States (1973-1998)".
External links
Images of leukemias
- UVA Healthsystem -- Images of acute leukemias by stage
Research organizations
- The Therapeutic Advances in Childhood Leukemia (TACL) Consortium -- US research group
- "Chromosomes, Leukaemias, Solid Tumors, Hereditary Cancers" in AtlasGeneticsOncology. For beginners.
|
||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||