Leprosy
| Leprosy (Hansen's Disease ) Classification and external resources |
||
 |
||
|---|---|---|
| A 24-year-old man infected with leprosy. | ||
| ICD-10 | A30. | |
| ICD-9 | 030 | |
| OMIM | 246300 | |
| DiseasesDB | 8478 | |
| MedlinePlus | 001347 | |
| eMedicine | med/1281 derm/223 neuro/187 | |
| MeSH | C01.252.410.040.552.386 | |
Leprosy (from the Greek lepi (λέπι), meaning scales on a fish), or Hansen's disease, is a chronic disease caused by the bacteria Mycobacterium leprae and Mycobacterium lepromatosis.[1][2] Leprosy is primarily a granulomatous disease of the peripheral nerves and mucosa of the upper respiratory tract; skin lesions are the primary external symptom.[3] Left untreated, leprosy can be progressive, causing permanent damage to the skin, nerves, limbs and eyes. Contrary to popular belief, leprosy does not actually cause body parts to simply fall off.[4]
Historically, leprosy has affected mankind since at least 600 BC, and was well-recognized in the civilizations of ancient China, Egypt and India.[5] In 1995, the World Health Organization (WHO) estimated that between two and three million people were permanently disabled because of leprosy.[6] Although the forced quarantine or segregation of patients is unnecessary—and can be considered unethical—a few leper colonies still remain around the world, in countries such as India, Japan, Egypt, Nepal and Vietnam. It is now commonly believed that many of the people who were segregated into these communities were presumed to have leprosy, when they actually had syphilis. Leprosy is not highly infectious, as approximately 95% of people are immune and sufferers are no longer infectious after only a couple of days on treatment. They would not have spread leprosy through a community; whereas syphilis, which has similar symptoms, is more contagious. One of the first signs of leprosy is the unexpected loss of eyelashes.
The age-old social stigma associated with the advanced form of leprosy lingers in many areas, and remains a major obstacle to self-reporting and early treatment. Effective treatment for leprosy appeared in the late 1930s with the introduction of dapsone and its derivatives. However, leprosy bacilli resistant to dapsone gradually evolved and became widespread, and it was not until the introduction of multidrug therapy (MDT) in the early 1980s that the disease could be diagnosed and treated successfully within the community.
Contents |
Characteristics

The clinical symptoms of leprosy vary but primarily affect the skin, nerves, and mucous membranes.[7] Patients with this chronic infectious disease are classified as having paucibacillary Hansen's disease (tuberculoid leprosy), multibacillary Hansen's disease (lepromatous leprosy), or borderline leprosy.
Classification
There is some confusion over classification because the WHO (World Health Organization) replaced an older, more complicated classification system with a simpler system that identifies two subtypes of leprosy: paucibacillary and multibacillary. The older system included six categories: Indeterminate Leprosy, Borderline Tuberculoid Leprosy, Midborderline Leprosy, Borderline Lepromatous Leprosy, Lepromatous Leprosy, and Tuberculoid Leprosy.
Paucibacillary leprosy encompasses indeterminate, tuberculoid, and borderline tuberculoid leprosy. It is characterized by one or more hypopigmented skin macules and anaesthetic patches, where skin sensations are lost because of damaged peripheral nerves that have been attacked by the human host's immune cells.
Multibacillary leprosy includes midborderline, borderline lepromatous, and lepromatous leprosy. It is associated with symmetric skin lesions, nodules, plaques, thickened dermis, and frequent involvement of the nasal mucosa resulting in nasal congestion and epistaxis (nose bleeds) but typically detectable nerve damage is late.
Borderline leprosy is of intermediate severity and is the most common form. Skin lesions resemble tuberculoid leprosy but are more numerous and irregular; large patches may affect a whole limb, and peripheral nerve involvement with weakness and loss of sensation is common. This type is unstable and may become more like lepromatous leprosy or may undergo a reversal reaction, becoming more like the tuberculoid form.
Cause

Mycobacterium leprae and Mycobacterium lepromatosis are the causative agents of leprosy. M. lepromatosis is only the causitive agent in diffuse lepromatous leprosy, which can be lethal.[3][2]
An intracellular, acid-fast bacterium, M. leprae is aerobic and rod-shaped, and is surrounded by the waxy cell membrane coating characteristic of Mycobacterium species.[8]
Due to extensive loss of genes necessary for independent growth, M. leprae and M. lepromatosis are unculturable in the laboratory, a factor which leads to difficulty in definitively identifying the organism under a strict interpretation of Koch's postulates.[9][2] The use of non-culture-based techniques such as molecular genetics has allowed for alternative establishment of causation.
Pathophysiology
The exact mechanism of transmission of leprosy is not known: prolonged close contact and transmission by nasal droplet have both been proposed, and, while the latter fits the pattern of disease, both remain unproven.[10] The only other animals besides humans known to contract leprosy are the armadillo, chimpanzee, sooty mangabey, and cynomolgus macaque.[11] The bacterium can also be grown in the laboratory by injection into the footpads of mice.[12] There is evidence that not all people who are infected with M. leprae develop leprosy, and genetic factors have long been thought to play a role, due to the observation of clustering of leprosy around certain families, and the failure to understand why certain individuals develop lepromatous leprosy while others develop other types of leprosy.[13] It is estimated that due to genetic factors, only 5 percent of the population is susceptible to leprosy.[14] This is mostly because the body is naturally immune to the bacteria, and those persons who do become infected are experiencing a severe allergic reaction to the disease. However, the role of genetic factors is not entirely clear in determining this clinical expression. In addition, malnutrition and prolonged exposure to infected persons may play a role in development of the overt disease.
The incubation period for the bacteria can last anywhere from two to ten years.
The most widely held belief is that the disease is transmitted by contact between infected persons and healthy persons.[15] In general, closeness of contact is related to the dose of infection, which in turn is related to the occurrence of disease. Of the various situations that promote close contact, contact within the household is the only one that is easily identified, although the actual incidence among contacts and the relative risk for them appear to vary considerably in different studies. In incidence studies, infection rates for contacts of lepromatous leprosy have varied from 6.2 per 1000 per year in Cebu, Philippines[16] to 55.8 per 1000 per year in a part of Southern India.[17]
Two exit routes of M. leprae from the human body often described are the skin and the nasal mucosa, although their relative importance is not clear. It is true that lepromatous cases show large numbers of organisms deep down in the dermis. However, whether they reach the skin surface in sufficient numbers is doubtful. Although there are reports of acid-fast bacilli being found in the desquamating epithelium (sloughing of superficial layer of skin) of the skin, Weddell et al had reported in 1963 that they could not find any acid-fast bacilli in the epidermis, even after examining a very large number of specimens from patients and contacts.[18] In a recent study, Job et al found fairly large numbers of M. leprae in the superficial keratin layer of the skin of lepromatous leprosy patients, suggesting that the organism could exit along with the sebaceous secretions.[19]
The importance of the nasal mucosa was recognized as early as 1898 by Schäffer, particularly that of the ulcerated mucosa.[20] The quantity of bacilli from nasal mucosal lesions in lepromatous leprosy was demonstrated by Shepard as large, with counts ranging from 10,000 to 10,000,000.[21] Pedley reported that the majority of lepromatous patients showed leprosy bacilli in their nasal secretions as collected through blowing the nose.[22] Davey and Rees indicated that nasal secretions from lepromatous patients could yield as much as 10 million viable organisms per day.[23]
The entry route of M. leprae into the human body is also not definitely known. The two seriously considered are the skin and the upper respiratory tract. While older research dealt with the skin route, recent research has increasingly favored the respiratory route. Rees and McDougall succeeded in the experimental transmission of leprosy through aerosols containing M. leprae in immune-suppressed mice, suggesting a similar possibility in humans.[24] Successful results have also been reported on experiments with nude mice when M. leprae were introduced into the nasal cavity by topical application.[25] In summary, entry through the respiratory route appears the most probable route, although other routes, particularly broken skin, cannot be ruled out. The CDC notes the following assertion about the transmission of the disease: "Although the mode of transmission of Hansen's disease remains uncertain, most investigators think that M. leprae is usually spread from person to person in respiratory droplets."[26]
In leprosy both the reference points for measuring the incubation period and the times of infection and onset of disease are difficult to define; the former because of the lack of adequate immunological tools and the latter because of the disease's slow onset. Even so, several investigators have attempted to measure the incubation period for leprosy. The minimum incubation period reported is as short as a few weeks and this is based on the very occasional occurrence of leprosy among young infants.[27] The maximum incubation period reported is as long as 30 years, or over, as observed among war veterans known to have been exposed for short periods in endemic areas but otherwise living in non-endemic areas. It is generally agreed that the average incubation period is between 3 and 5 years.
Treatment

Until the development of dapsone, rifampicin, and clofazimine in the 1940s, there was no effective cure for leprosy. However, dapsone is only weakly bactericidal against M. leprae and it was considered necessary for patients to take the drug indefinitely. Moreover, when dapsone was used alone, the M. leprae population quickly evolved antibiotic resistance; by the 1960s, the world's only known anti-leprosy drug became virtually useless.
The search for more effective anti-leprosy drugs than dapsone led to the use of clofazimine and rifampicin in the 1960s and 1970s.[28] Later, Indian scientist Shantaram Yawalkar and his colleagues formulated a combined therapy using rifampicin and dapsone, intended to mitigate bacterial resistance.[29] Multidrug therapy (MDT) and combining all three drugs was first recommended by a WHO Expert Committee in 1981. These three anti-leprosy drugs are still used in the standard MDT regimens. None of them are used alone because of the risk of developing resistance.
Because this treatment is quite expensive, it was not quickly adopted in most endemic countries. In 1985 leprosy was still considered a public health problem in 122 countries. The 44th World Health Assembly (WHA), held in Geneva in 1991 passed a resolution to eliminate leprosy as a public health problem by the year 2000 — defined as reducing the global prevalence of the disease to less than 1 case per 100,000. At the Assembly, the World Health Organization (WHO) was given the mandate to develop an elimination strategy by its member states, based on increasing the geographical coverage of MDT and patients’ accessibility to the treatment.
The WHO Study Group's report on the Chemotherapy of Leprosy in 1993 recommended two types of standard MDT regimen be adopted.[30] The first was a 24-month treatment for multibacillary (MB or lepromatous) cases using rifampicin, clofazimine, and dapsone. The second was a six-month treatment for paucibacillary (PB or tuberculoid) cases, using rifampicin and dapsone. At the First International Conference on the Elimination of Leprosy as a Public Health Problem, held in Hanoi the next year, the global strategy was endorsed and funds provided to WHO for the procurement and supply of MDT to all endemic countries.

Between 1995 and 1999, WHO, with the aid of the Nippon Foundation (Chairman Yōhei Sasakawa, World Health Organization Goodwill Ambassador for Leprosy Elimination), supplied all endemic countries with free MDT in blister packs, channelled through Ministries of Health. This free provision was extended in 2000 with a donation by the MDT manufacturer Novartis, which will run until at least the end of 2010. At the national level, non-government organizations (NGOs) affiliated to the national programme will continue to be provided with an appropriate free supply of this WHO supplied MDT by the government.
MDT remains highly effective and patients are no longer infectious after the first monthly dose.[5] It is safe and easy to use under field conditions due to its presentation in calendar blister packs.[5] Relapse rates remain low, and there is no known resistance to the combined drugs.[5] The Seventh WHO Expert Committee on Leprosy,[31] reporting in 1997, concluded that the MB duration of treatment—then standing at 24 months—could safely be shortened to 12 months "without significantly compromising its efficacy."
Persistent obstacles to the elimination of the disease include improving detection, educating patients and the population about its cause, and fighting social taboos about a disease for which patients have historically been considered "unclean" or "cursed by God" as outcasts. Where taboos are strong, patients may be forced to hide their condition (and avoid seeking treatment) to avoid discrimination. The lack of awareness about Hansen's disease can lead people to falsely believe that the disease is highly contagious and incurable.
The ALERT hospital and research facility in Ethiopia provides training to medical personnel from around the world in the treatment of leprosy, as well as treating many local patients. Surgical techniques, such as for the restoration of control of movement of thumbs, have been developed there.
Prevention
A single dose of rifampicin is able to reduce the rate of leprosy in contacts by 57% to 75%.[32][33]
BCG is able to offer a variable amount of protection against leprosy as well as against tuberculosis.[34][35]
Epidemiology
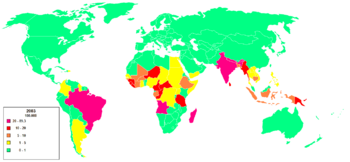
Worldwide, two to three million people are estimated to be permanently disabled because of Leprosy.[6] India has the greatest number of cases, with Brazil second and Burma third.
In 1999, the world incidence of Hansen's disease was estimated to be 640,000. In 2000, 738,284 cases were identified. In 1999, 108 cases occurred in the United States. In 2000, the World Health Organization (WHO) listed 91 countries in which Hansen's disease is endemic. India, Myanmar and Nepal contained 70% of cases. In 2002, 763,917 new cases were detected worldwide, and in that year the WHO listed Brazil, Madagascar, Mozambique, Tanzania and Nepal as having 90% of Hansen's disease cases.
According to recent figures from the WHO, new cases detected worldwide have decreased by approximately 107,000 cases (or 21%) from 2003 to 2004. This decreasing trend has been consistent for the past three years. In addition, the global registered prevalence of HD was 286,063 cases; 407,791 new cases were detected during 2004.
In the United States, Hansen's disease is tracked by the Centers for Disease Control and Prevention (CDC), with a total of 92 cases being reported in 2002.[36] Although the number of cases worldwide continues to fall, pockets of high prevalence continue in certain areas such as Brazil, South Asia (India, Nepal), some parts of Africa (Tanzania, Madagascar, Mozambique) and the western Pacific.
Risk groups
At highest risk are those living in endemic areas with poor conditions such as inadequate bedding, contaminated water and insufficient diet, or other diseases (such as HIV) that compromise immune function. Recent research suggests that there is a defect in cell-mediated immunity that causes susceptibility to the disease. Less than ten percent of the world's population is actually capable of acquiring the disease . The region of DNA responsible for this variability is also involved in Parkinson disease, giving rise to current speculation that the two disorders may be linked in some way at the biochemical level. In addition, men are twice as likely to contract leprosy as women. According to The Leprosy Mission Canada, most people – about 95% of the population – are naturally immune.
Disease burden
Although annual incidence—the number of new leprosy cases occurring each year—is important as a measure of transmission, it is difficult to measure in leprosy due to its long incubation period, delays in diagnosis after onset of the disease and the lack of laboratory tools to detect leprosy in its very early stages. - - Instead, the registered prevalence is used. Registered prevalence is a useful proxy indicator of the disease burden as it reflects the number of active leprosy cases diagnosed with the disease and receiving treatment with MDT at a given point in time. The prevalence rate is defined as the number of cases registered for MDT treatment among the population in which the cases have occurred, again at a given point in time.[37]
New case detection is another indicator of the disease that is usually reported by countries on an annual basis. It includes cases diagnosed with onset of disease in the year in question (true incidence) and a large proportion of cases with onset in previous years (termed a backlog prevalence of undetected cases). The new case detection rate (NCDR) is defined by the number of newly detected cases, previously untreated, during a year divided by the population in which the cases have occurred.
Endemic countries also report the number of new cases with established disabilities at the time of detection, as an indicator of the backlog prevalence. However, determination of the time of onset of the disease is generally unreliable, is very labour-intensive and is seldom done in recording these statistics.
Global situation
| Table 1: Prevalence at beginning of 2006, and trends in new case detection 2001-2005, excluding Europe | ||||||
| Region | Registered prevalence
(rate/1,000,000 pop.) |
New case detection during the year | ||||
|---|---|---|---|---|---|---|
| Start of 2006 | 2001 | 2002 | 2003 | 2004 | 2005 | |
| Africa | 40,830 (0.56) | 39,612 | 48,248 | 47,006 | 46,918 | 42,814 |
| Americas | 32,904 (0.39) | 42,830 | 39,939 | 52,435 | 52,662 | 41,780 |
| South-East Asia | 133,422 (0.81) | 668,658 | 520,632 | 405,147 | 298,603 | 201,635 |
| Eastern Mediterranean | 4,024 (0.09) | 4,758 | 4,665 | 3,940 | 3,392 | 3,133 |
| Western Pacific | 8,646 (0.05) | 7,404 | 7,154 | 6,190 | 6,216 | 7,137 |
| Totals | NA | 763,262 | 620,638 | 514,718 | 407,791 | 296,499 |
| Table 2: Prevalence and detection, countries still to reach elimination | ||||||
| Countries | Registered prevalence
(rate/10,000 pop.) |
New case detection
(rate/100,000 pop.) |
||||
|---|---|---|---|---|---|---|
| Start of 2004 | Start of 2005 | Start of 2006 | During 2003 | During 2004 | During 2005 | |
| 79,908 (4.6) | 30,693 (1.7) | 27,313 (1.5) | 49,206 (28.6) | 49,384 (26.9) | 38,410 (20.6) | |
| 6,810 (3.4) | 4,692 (2.4) | 4,889 (2.5) | 5,907 (29.4) | 4,266 (22.0) | 5,371 (27.1) | |
| 7,549 (3.1) | 4,699 (1.8) | 4,921 (1.8) | 8,046 (32.9) | 6,958 (26.2) | 6,150 (22.7) | |
| 5,420 (1.6) | 4,777 (1.3) | 4,190 (1.1) | 5,279 (15.4) | 5,190 (13.8) | 4,237 (11.1) | |
| Totals | NA | NA | NA | NA | NA | NA |
As reported to WHO by 115 countries and territories in 2006, and published in the Weekly Epidemiological Record the global registered prevalence of leprosy at the beginning of the year was 219,826 cases.[38] New case detection during the previous year (2005 - the last year for which full country information is available) was 296,499. The reason for the annual detection being higher than the prevalence at the end of the year can be explained by the fact that a proportion of new cases complete their treatment within the year and therefore no longer remain on the registers. The global detection of new cases continues to show a sharp decline, falling by 110,000 cases (27%) during 2005 compared with the previous year.
Table 1 shows that global annual detection has been declining since 2001. The African region reported an 8.7% decline in the number of new cases compared with 2004. The comparable figure for the Americas was 20.1%, for South-East Asia 32% and for the Eastern Mediterranean it was 7.6%. The Western Pacific area, however, showed a 14.8% increase during the same period.
Table 2 shows the leprosy situation in the four major countries which have yet to achieve the goal of elimination at the national level. It should be noted that: a) Elimination is defined as a prevalence of less than 1 case per 10,000 population; b) Madagascar reached elimination at the national level in September 2006; c) Nepal detection reported from mid-November 2004 to mid-November 2005; and d) D.R. Congo officially reported to WHO in 2008 that it had reached elimination by the end of 2007, at the national level.
History
The Oxford Illustrated Companion to Medicine holds that the mention of leprosy, as well as ritualistic cures for it, were already described in the Hindu religious book Atharva-veda.[39] Writing in the Encyclopedia Britannica 2008, Kearns & Nash state that the first mention of leprosy is described in the Indian medical treatise Sushruta Samhita (6th century BC).[40] The Cambridge Encyclopedia of Human Paleopathology (1998) holds that: "The Sushruta Samhita from India describes the condition quite well and even offers therapeutic suggestions as early as about 600 BC"[41] The surgeon Sushruta flourished in the Indian city of Kashi by the 6th century BC,[42] and the medical treatise Sushruta Samhita—attributed to him—made its appearance during the 1st millennium BC.[40] The earliest surviving excavated written material which contains the works of Sushruta is the Bower Manuscript—dated to the 4th century AD, almost a millennium after the original work.[43]
In regards to ancient China, Katrina C. D. McLeod and Robin D. S. Yates identify the State of Qin's Feng zhen shi 封診式 (Models for sealing and investigating), dated 266-246 BC, as offering the earliest known unambiguous description of the symptoms of low-resistance leprosy, even though it was termed then under li 癘, a general Chinese word for skin disorder.[44] This 3rd century BC Chinese text on bamboo slip, found in an excavation of 1975 at Shuihudi, Yunmeng, Hubei province, not only described the destruction of the "pillar of the nose", but also the "swelling of the eyebrows, loss of hair, absorption of nasal cartilage, affliction of knees and elbows, difficult and hoarse respiration, as well as anaesthesia."[44]
In the West, the earliest known description of leprosy there was made by the Roman encyclopedist Aulus Cornelius Celsus (25 BC – 37 AD) in his De Medicina; he called leprosy "elephantiasis".[44] The Roman author Pliny the Elder (23–79 AD) mentioned the same disease.[44] Although "sara't" of Leviticus (Old Testament) is translated as "lepra" in the 5th century AD Vulgate, the original term sara't found in Leviticus was not the elephantiasis described by Celsus and Pliny; in fact, sara't was used to describe a disease which could affect houses and clothing.[44] Katrina C. D. McLeod and Robin D. S. Yates state that sara't "denotes a condition of ritual impurity or a temporary form of skin disease."[44] In the Muslim world, the Persian polymath Avicenna (c. 980–1037) was the first outside of China to describe the destruction of the nasal septum in those suffering from leprosy.[44]
Numerous leprosaria, or leper hospitals, sprang up in the Middle Ages; Matthew Paris estimated that in the early thirteenth century there were 19,000 across Europe.[45] The first recorded Leper colony was in Harbledown. These institutions were run along monastic lines and, while lepers were encouraged to live in these monastic-type establishments, this was for their own health as well as quarantine. Indeed, some medieval sources indicate belief that those suffering from leprosy were considered to be going through Purgatory on Earth, and for this reason their suffering was considered holier than the ordinary person's. More frequently, lepers were seen to exist in a place between life and death: they were still alive, yet many chose or were forced to ritually separate themselves from mundane existence.[46]
Radegund was noted for washing the feet of lepers. Orderic Vitalis writes of a monk, Ralf, who was so overcome by the plight of lepers that he prayed to catch leprosy himself (which he eventually did). The leper would carry a clapper and bell to warn of his approach, and this was as much to attract attention for charity as to warn people that a diseased person was near.

Mycobacterium leprae, the causative agent of leprosy, was discovered by G. H. Armauer Hansen in Norway in 1873, making it the first bacterium to be identified as causing disease in humans.[47][48] He worked at St. Jørgens Hospital in Bergen, founded early in the fifteenth century. St. Jørgens is today a museum, Lepramuseet, probably the best preserved leprosy hospital in Northern Europe.[49]
Historically, individuals with Hansen's disease have been known as lepers, however, this term is falling into disuse as a result of the diminishing number of leprosy patients and the pejorative connotations of the term. The term most widely accepted among professionals is "people affected by Hansen's disease."
Historically, the term Tzaraath from the Hebrew Bible was, erroneously, commonly translated as leprosy, although the symptoms of Tzaraath were not entirely consistent with leprosy and rather referred to a variety of disorders other than Hansen's disease.[50]
In particular, tinea capitis (fungal scalp infection) and related infections on other body parts caused by the dermatophyte fungus Trichophyton violaceum are abundant throughout the Middle East and North Africa today and might also have been common in biblical times. Similarly, the related agent of the disfiguring skin disease favus, Trichophyton schoenleinii, appears to have been common throughout Eurasia and Africa before the advent of modern medicine. Persons with severe favus and similar fungal diseases (and potentially also with severe psoriasis and other diseases not caused by microorganisms) tended to be classed as having leprosy as late as the 17th century in Europe.[51] This is clearly shown in the painting Governors of the Home for Lepers at Haarlem 1667 by Jan de Bray (Frans Hals Museum, Haarlem, the Netherlands), where a young Dutchman with a vivid scalp infection, almost certainly caused by a fungus, is shown being cared for by three officials of a charitable home intended for leprosy sufferers. The use of the word "leprosy" before the mid-19th century, when microscopic examination of skin for medical diagnosis was first developed, can seldom be correlated reliably with Hansen's disease as we understand it today.
The word "leprosy" derives from the ancient Greek words lepros, a scale, and lepein, to peel.[52] The word came into the English language via Latin and Old French. The first attested English use is in the Ancrene Wisse, a 13th-century manual for nuns ("Moyseses hond..bisemde o þe spitel uuel & þuhte lepruse." The Middle English Dictionary, s.v., "leprous"). A roughly contemporaneous use is attested in the Anglo-Norman Dialogues of Saint Gregory, "Esmondez i sont li lieprous" (Anglo-Norman Dictionary, s.v., "leprus").
Famous lepers
- Blessed Damien of Moloka'i was a Roman Catholic missionary who became a leper when he spent the rest of his life serving in the leper colony at Moloka'i.
- King Baldwin IV of Jerusalem.
- Possibly Robert I de Brus, King of Scots.
- Vietnamese poet Han Mac Tu
- Otani Yoshitsugu, a Japanese Daimyo.
References
- ↑ Sasaki S, Takeshita F, Okuda K, Ishii N (2001). "Mycobacterium leprae and leprosy: a compendium". Microbiol Immunol 45 (11): 729–36. PMID 11791665. http://www.jstage.jst.go.jp/article/mandi/45/11/729/_pdf.
- ↑ 2.0 2.1 2.2 http://www.sciencedaily.com/releases/2008/11/081124141047.htm
- ↑ 3.0 3.1 Kenneth J. Ryan, C. George Ray, editors. (2004). Ryan KJ, Ray CG. ed.. Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. 451–3. ISBN 0838585299. OCLC 52358530 61405904.
- ↑ "Lifting the stigma of leprosy: a new vaccine offers hope against an ancient disease". Time 119 (19): 87. May 1982. PMID 10255067. http://www.time.com/time/magazine/article/0,9171,925377,00.html.
- ↑ 5.0 5.1 5.2 5.3 "Leprosy". WHO. Retrieved on 2007-08-22.
- ↑ 6.0 6.1 WHO (1995). "Leprosy disabilities: magnitude of the problem". Weekly Epidemiological Record 70 (38): 269–75. PMID 7577430.
- ↑ Naafs B, Silva E, Vilani-Moreno F, Marcos E, Nogueira M, Opromolla D (2001). "Factors influencing the development of leprosy: an overview". Int J Lepr Other Mycobact Dis 69 (1): 26–33. PMID 11480313.
- ↑ McMurray DN (1996). Mycobacteria and Nocardia. in: Baron's Medical Microbiology (Baron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1. OCLC 33838234. http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=mmed.section.1833.
- ↑ Bhattacharya S, Vijayalakshmi N, Parija SC (2002). "Uncultivable bacteria: Implications and recent trends towards identification". Indian journal of medical microbiology 20 (4): 174–7. PMID 17657065. http://www.ijmm.org/article.asp?issn=0255-0857;year=2002;volume=20;issue=4;spage=174;epage=177;aulast=Bhattacharya.
- ↑ Reich CV (1987). "Leprosy: cause, transmission, and a new theory of pathogenesis". Rev. Infect. Dis. 9 (3): 590–4. PMID 3299638.
- ↑ Rojas-Espinosa O, Løvik M (2001). "Mycobacterium leprae and Mycobacterium lepraemurium infections in domestic and wild animals". Rev. - Off. Int. Epizoot. 20 (1): 219–51. PMID 11288514.
- ↑ Hastings RC, Gillis TP, Krahenbuhl JL, Franzblau SG (1988). "Leprosy". Clin. Microbiol. Rev. 1 (3): 330–48. PMID 3058299. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=3058299.
- ↑ Alcaïs A, Mira M, Casanova JL, Schurr E, Abel L (2005). "Genetic dissection of immunity in leprosy". Curr. Opin. Immunol. 17 (1): 44–8. doi:. PMID 15653309.
- ↑ "AR Dept of Health debunks leprosy fears" (2008-02-08). Retrieved on 2008-04-08.
- ↑ Kaur H, Van Brakel W (2002). "Dehabilitation of leprosy-affected people—a study on leprosy-affected beggars". Leprosy review 73 (4): 346–55. PMID 12549842.
- ↑ Doull JA, Guinto RA, Rodriguez RS, et al. (1942). "The incidence of leprosy in Cordova and Talisay, Cebu, Philippines". International Journal of Leprosy 10: 107–131.
- ↑ Noordeen S, Neelan P (1978). "Extended studies on chemoprophylaxis against leprosy". Indian J Med Res 67: 515–27. PMID 355134.
- ↑ Weddell G, Palmer E (1963). "The pathogenesis of leprosy. An experimental approach". Leprosy Review 34: 57–61. PMID 13999438.
- ↑ Job C, Jayakumar J, Aschhoff M (1999). ""Large numbers" of Mycobacterium leprae are discharged from the intact skin of lepromatous patients; a preliminary report". Int J Lepr Other Mycobact Dis 67 (2): 164–7. PMID 10472371.
- ↑ Arch Dermato Syphilis 1898; 44:159–174
- ↑ Shepard C (1960). "Acid-fast bacilli in nasal excretions in leprosy, and results of inoculation of mice". Am J Hyg 71: 147–57. PMID 14445823.
- ↑ Pedley J (1973). "The nasal mucus in leprosy". Lepr Rev 44 (1): 33–5. PMID 4584261.
- ↑ Davey T, Rees R (1974). "The nasal dicharge in leprosy: clinical and bacteriological aspects". Lepr Rev 45 (2): 121–34. PMID 4608620.
- ↑ Rees R, McDougall A (1977). "Airborne infection with Mycobacterium leprae in mice". J Med Microbiol 10 (1): 63–8. PMID 320339.
- ↑ Chehl S, Job C, Hastings R (1985). "Transmission of leprosy in nude mice". Am J Trop Med Hyg 34 (6): 1161–6. PMID 3914846.
- ↑ CDC Disease Info hansens_t Hansen's Disease (Leprosy)
- ↑ Montestruc E, Berdonneau R (1954). "2 New cases of leprosy in infants in Martinique" (in French). Bull Soc Pathol Exot Filiales 47 (6): 781–3. PMID 14378912.
- ↑ Rees RJ, Pearson JM, Waters MF (1970). "Experimental and clinical studies on rifampicin in treatment of leprosy". Br Med J 688 (1): 89–92. PMID 4903972.
- ↑ Yawalkar SJ, McDougall AC, Languillon J, Ghosh S, Hajra SK, Opromolla DV, Tonello CJ (1982). "Once-monthly rifampicin plus daily dapsone in initial treatment of lepromatous leprosy". Lancet 8283 (1): 1199–1202. doi:. PMID 6122970.
- ↑ "Chemotherapy of Leprosy". WHO Technical Report Series 847. WHO (1994). Retrieved on 2007-03-24.
- ↑ "Seventh WHO Expert Committee on Leprosy". WHO Technical Report Series 874. WHO (1998). Retrieved on 2007-03-24.
- ↑ Moet FJ, Pahan D, Oskam L, Richardus JH (2008). "Effectiveness of single dose rifampicin in preventing leprosy in close contacts of patients with newly diagnosed leprosy: cluster randomised controlled trial". BMJ 336: 761. doi:. PMID 18332051.
- ↑ Bakker MI, Hatta M, Kwenang A, et al. (2005). "Prevention of leprosy using rifampicin as chemoprophylaxis". Am J Trop Med Hyg 72: 443–8. PMID 15827283. http://www.ajtmh.org/cgi/content/abstract/72/4/443?ijkey=4b15a78b876fd990dfd877ee89b22399c026501c&keytype2=tf_ipsecsha.
- ↑ Fine PE, Smith PG (1996). "Vaccination against leprosy—the view from 1996". Lepr Rev 67 (4): 249–52. PMID 9033195.
- ↑ Karonga prevention trial group (1996). "Randomized controlled trial of single BCG, repeated BCG, or combined BCG and killed Mycobacterium leprae vaccine for prevention of leprosy and tuberculosis in Malawi". Lancet 348: 17–24. doi:. PMID 8691924.
- ↑ CDC Leprosy Fact Sheet.
- ↑ "Epidemiology of leprosy in relation to control. Report of a WHO Study Group". World Health Organ Tech Rep Ser (Geneva: World Health Organization) 716: 1–60. 1985. ISBN 9241207167. OCLC 12095109. PMID 3925646.
- ↑ "Global leprosy situation, 2006" (PDF). Weekly Epidemiological Record 81 (32): 309–16. August 2006. PMID 16903018. http://www.who.int/lep/resources/wer8132.pdf.
- ↑ Lock etc., page 420
- ↑ 40.0 40.1 Kearns & Nash (2008)
- ↑ Aufderheide, A. C.; Rodriguez-Martin, C. & Langsjoen, O. (1998). The Cambridge Encyclopedia of Human Paleopathology. Cambridge University Press. ISBN 0521552036. Page 148.
- ↑ Dwivedi & Dwivedi (2007)
- ↑ Kutumbian, P. (2005). Ancient Indian Medicine. Orient Longman. ISBN 8125015213. pages XXXII-XXXIII.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 44.6 McLeod, Katrina C. D. and Robin D. S. Yates (June 1981). "Forms of Ch'in Law: An Annotated Translation of The Feng-chen shih". Harvard Journal of Asiatic Studies 41 (1): 111–63. Pages 152–3 & footnote 147. doi:.
- ↑
 "Leprosy". Catholic Encyclopedia. (1913). New York: Robert Appleton Company.
"Leprosy". Catholic Encyclopedia. (1913). New York: Robert Appleton Company. - ↑ Brody, Saul Nathaniel (1974). The Disease of the Soul: Leprosy in Medieval Literature. Ithaca: Cornell Press.
- ↑ Hansen GHA (1874). "Undersøgelser Angående Spedalskhedens Årsager (Investigations concerning the etiology of leprosy)" (in Norwegian). Norsk Mag. Laegervidenskaben 4: 1–88.
- ↑ Irgens L (2002). "The discovery of the leprosy bacillus". Tidsskr nor Laegeforen 122 (7): 708–9. PMID 11998735.
- ↑ Bymuseet i Bergen
- ↑ Artscroll Tanakh, Leviticus 13:59, 1996
- ↑ Kane J, Summerbell RC, Sigler L, Krajden S, Land G (1997). Laboratory Handbook of Dermatophytes: A clinical guide and laboratory manual of dermatophytes and other filamentous fungi from skin, hair and nails. Star Publishers (Belmont, CA). ISBN 0898631572. OCLC 37116438.
- ↑ Barnhart RK (1995). Barnhart Concise Dictionary of Etymology. New York: Harper Collins. ISBN 0062700847. OCLC 221898877 223496345 231655185 30399281.
See also
- Dwivedi, Girish & Dwivedi, Shridhar (2007). History of Medicine: Sushruta – the Clinician – Teacher par Excellence. National Informatics Centre (Government of India).
- Dunea, George; Lock, Stephen; Last, John M. (2001). The Oxford illustrated companion to medicine. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-262950-6. OCLC 150308752 180030517 213488544 244006190 43342122 46678589 58460632 59406536 69646604.
- Kearns, Susannah C.J. & Nash, June E. (2008). Leprosy. Encyclopedia Britannica.
Further reading
- Bargès A (1993). "Ségrégation antilépreuse et comportements adaptatifs à Bamako (Mali)" (PDF). Ecologie humaine 11 (2): 7–20. http://halshs.archives-ouvertes.fr/docs/00/25/89/20/PDF/Environnmement_africain_et_maladie-Barges1993.pdf.
- Bargès A (1996). "Entre conformismes et changements, le monde de la lèpre au Mali" (PDF). Paris, Editions Karthala: 280–313. http://halshs.archives-ouvertes.fr/docs/00/26/60/96/PDF/Le_monde_la_lepre_1996(1993).pdf.
- Clark E (1994). "Social Welfare and Mutual Aid in the Medieval Countryside". The Journal of British Studies 33 (4): 394–6. http://links.jstor.org/sici?sici=0021-9371(199410)33%3A4%3C381%3ASWAMAI%3E2.0.CO%3B2-L.
- Icon Health Publications (2004). Leprosy: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References. San Diego: Icon Health Publications. ISBN 0-597-84006-7. OCLC 162128079 191036288.
- Demaitre L (2007). Leprosy in Premodern Medicine: A Malady of the Whole Body. Baltimore, Maryland: The Johns Hopkins University Press. ISBN 978-0-8018-8613-3. OCLC 238882127 70921424.
- Rawcliffe C (2001). "Learning to Love the Leper: aspects of institutional Charity in Anglo Norman England". Anglo Norman Studies 23: 233–52.
- Rawcliffe C (2006). Leprosy in Medieval England. Ipswich: Boydell Press. ISBN 1843832739. OCLC 70765638.
- Talarigo J (2004). The Pearl Diver: (fiction) young woman with leprosy is exiled to leprosy colony in Japan, 1929. Doubleday. ISBN 1-4025-8661-2. OCLC 55066644.
- Tayman J (2006). The Colony: The Harrowing True Story of the Exiles of Molokai. Simon & Schuster. ISBN 0-7432-3300.
- Brennert A (2003). Moloka'i:(fiction) young woman with leprosy is exiled to leprosy colony in Hawaii, 1891. St. Martin's Press. ISBN 0-312-30435-8. OCLC 123959155 56695775.
External links
- Leprosy and Human Rights - event held at Woodrow Wilson International Center for Scholars, March 2008
- National Hansen's Disease Programs (NHDP), U.S. Health Resources and Services Administration
- Hansen's Disease (Leprosy) - Centers for Disease Control and Prevention
- World Health Organization (WHO) leprosy website
- Hope in a Modern-Day Leper Colony Article from a leper colony in India
- American Leprosy Missions
- Rinaldi A (December 2005). "The global campaign to eliminate leprosy". PLoS Med. 2 (12): e341. doi:. PMID 16363908.
- LEPRA - Health in Action UK Based organisation founded in 1924 to treat leprosy and related diseases of poverty.
- History of leprosy
- "Anthropology and History of leprosy" (Histoire & Anthropologie, 15 (1995) 115-122).
- ILA Global Project on the History of Leprosy
- National Hansen's Disease Museum
- BBC News: Slave trade key to leprosy spread
- "Interview with author John Tayman (The Colony)" (MP3 audio: runtime = 00:23:20, 10.7 mb). IT Conversations Tech Nation (2006-02-07). Retrieved on 2007-03-22.
- Research
- Pathology Images of Leprosy and Other Granulomatous diseases Yale Rosen, M.D.
- INFOLEP Leprosy Information Services
- Leprosy Review
- "Medical anthropology, Leprosy and Health Care in French speaking West-Africa" (PDF).
- Photographs of leprosy patients: type leprosy in the diagnosis space for some photographs and then type leproma for another photograph.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||