Isotretinoin
 |
|
 |
|
|
Isotretinoin
|
|
| Systematic (IUPAC) name | |
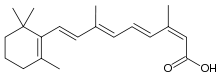
| (2Z,4E,6E,8E)-3,7-dimethyl-9-(2,6,6-trimethyl-1- cyclohexenyl)nona-2,4,6,8-tetraenoic acid |
|
| Identifiers | |
| CAS number | |
| ATC code | D10 |
| PubChem | |
| DrugBank | |
| ChemSpider | |
| Chemical data | |
| Formula | C20H28O2 |
| Mol. mass | 300.44 g/mol |
| Pharmacokinetic data | |
| Bioavailability | Variable |
| Protein binding | 99.9% |
| Metabolism | Hepatic |
| Half life | 10–20 hours |
| Excretion | Renal and fecal |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral, topical |
Isotretinoin (INN) (pronounced /aɪsoʊtrɨˈtɪnoʊɨn/ or /ˌaɪsoʊtrɨˈtɪnoʊɨn/[1]) is a medication used for the treatment of severe acne. It is sometimes used as a chemotherapy medication for prevention and treatment of certain skin cancers. In some cases, it is used to treat Harlequin type ichthyosis, a usualy lethal skin deformation in which sufferers develop armor plated-like skin and usually die soon after birth. It is a retinoid, meaning it derives from vitamin A and is found in small quantities naturally in the body. Oral isotretinoin is marketed under various trade names, most commonly Accutane (Roche), Amnesteem (Mylan), Claravis (Barr), Decutan (Actavis), Isotane (Pacific Pharmaceuticals), Sotret (Ranbaxy), Oratane (Genepharm Australasia) or Roaccutane (Roche), Izotek (BlauFarma); while topical isotretinoin is most commonly marketed under the trade names Isotrex or Isotrexin (Stiefel).
Contents |
History
Prior to the development of isotretinoin, the mainstay treatment of moderate to severe or persistent acne was oral antibiotics such as the tetracyclines and erythromycin. While these drugs have proven efficacy, they worked against only one contributing factor of acne – the Propionibacterium acnes bacteria. The antibiotics gradually became less effective over time as more resistant strains of the bacterium became prominent.
An early, effective treatment of acne was high doses of the fat-soluble vitamin A. At these dose levels (sometimes 500,000 IU per day) effects such as reduced production of sebum and dry hair could be noticed . However the vitamin also had many other prominent side effects which inhibited its widespread use .
The development of the retinoic acid derivative isotretinoin (13-cis-retinoic acid), and its release in 1982 by Hoffmann-La Roche, was a great step forward in the treatment of acne. The synthetic compound provided better therapeutic benefit than vitamin A, while also producing fewer adhfgjkverse effects. In February 2002, Roche's patents for isotretinoin expired and there are now many other companies selling cheaper generic versions of the drug.
Because of a 1984 study funded by Roche, high dosages of the drug became mainstream in treatment. Lower dosages were found to be effective in treatment by independent research (see dosage section of this article), but Roche's dosage recommendations still continue to be used.
From the time of its introduction the drug was known to have teratogenic potential, and pregnancies with the drug were strongly discouraged. When they occurred, they were found to have approximately 30% rates of congenital malformation, versus a 3-5% baseline risk.[2] Beginning in 1998, prescriptions of the drug came under scrutiny, as fewer than half of prescribers were testing for pregnancy, usually relying on less sensitive urine tests.[3] On the grounds that pregnancies by women taking the drug had been underreported by the manufacturer between 1982 and 2000, and that once generic manufacturers entered the market risk management was no longer centralized, the FDA instituted restrictions on prescribing and dispensing the drug, first with the "System to Manage Accutane Related Teratogenicity" (SMART) in 2000, and subsequently the iPLEDGE program in 2006. A retrospective cohort study recently found that pregnancy rates were quite high during the period (1 per 30 women per year), but 84% of pregnancies were ended by induced abortion.[2]
In countries that do not restrict distribution of isotretinoin, pharmacists recommend 5mg or 10mg daily, since at lower dosages the adverse side effects are diminished. Isotretinoin in topical form is also prescribed.
Isotretinoin is available over the internet from countries where it can be dispensed without a prescription. It is an ongoing problem for governments where a prescription is required, as it is mailed illegally across borders.
Pharmacodynamics
Isotretinoin's exact mechanism of action is unknown. However it is known that, like other retinoids, the drug alters DNA transcription.[4] This effect decreases the size and output of sebaceous glands, making the cells that are sloughed off into the sebaceous glands less sticky, and therefore less able to form comedones. Isotretinoin noticeably reduces the production of sebum and shrinks the sebaceous glands. It stabilizes keratinization and prevents comedones from forming. This combined impact on several of the contributory factors in acne distinguishes isotretinoin from alternative remedies such as antibiotics and accounts for its greater efficacy in severe, nodulocystic cases.
Pharmacokinetics
Isotretinoin, when administered orally, is best absorbed when taken after a high fat meal, as it has a high level of lipophilicity. In a crossover study, it was found that the peak plasma concentration more than doubled when taken after a high fat meal versus a fasted condition. Isotretinoin is primarily (99.9%) bound to plasma proteins, mostly albumin. At least three metabolites have been detected in human plasma after oral administration of isotretinoin. These are 4-oxo-isotretinoin, retinoic acid and 4-oxo-retinoic acid. Isotretinoin also oxidises, irreversibly, to 4-oxo-isotretinoin. The metabolites of isotretinoin are excreted through both urine and feces. The mean elimination half-life is 21 hours, with a standard deviation from this mean of 8.2 hours.
Clinical use
Currently, isotretinoin continues to be used only after other acne treatments fail to produce results. Treatment of acne begins with topical medications (e.g. benzoyl peroxide, adapalene, etc), followed by oral antibiotics (or a combination) and finally isotretinoin therapy. This is because other treatments, while less effective than isotretinoin, are thought to be associated with fewer adverse effects and lower cost. The higher cost is due to the medical supervision required in taking a toxic dosage. The cost of the medicine is also a factor (example: taking 5, 10, or even 20mg daily is far less expensive than taking 80mg daily).
Indications
Isotretinoin is indicated for the treatment of severe cystic acne vulgaris.[5][6] It is also effective for hidradenitis suppurativa and some cases of severe acne rosacea.[6] It can also be used to help treat harlequin ichthyosis, and is used in xeroderma pigmentosum cases to relieve keratoses.
Although extremely rare, isotretinoin has been used as a treatment for Fibrodysplasia Ossificans Progressiva.
Prescribing restrictions
In the United Kingdom, this drug may only be prescribed by, or under the supervision of, a consultant dermatologist.[7] Because severe, cystic acne has the potential to cause permanent scarring over a short period, restrictions on isotretinoin's more immediate availability have proved contentious.[8] Similar restrictions are common in most Australian states – in New South Wales and Victoria, for instance, the prescriber must be a Fellow of the Australasian College of Dermatologists (FACD).[9]
In New Zealand, isotretinoin can be prescribed by any doctor but is subsidised only if prescribed by a skin specialist/dermatologist. As New Zealand General Practitioner visits are subsidised it is usually cheaper for the patient to buy their isotretinoin with a GP prescription than to pay to see a dermatologist.
Since 1 March 2006, the dispensing of isotretinoin in the United States has been controlled by a FDA-mandated website called iPLEDGE – dermatologists are required to register their patients before prescribing and pharmacists are required to check the website before dispensing the drug. The patient must visit the iPLEDGE website or call the hotline number in order to log in with his or her ID code to answer the iPLEDGE questionaire. The prescription may not be dispensed until all three parties have complied. A physician may not prescribe more than a 30-day supply. A new prescription may not be written for at least 30 days. Pharmacies are also under similar restriction. There is also a 7-day window in which the medication must be picked up at the pharmacy. If the original prescription is lost, or pick-up window is missed, the patient must re-qualify to have another prescription written. Doctors and pharmacists must also verify written prescriptions in an online system before patients may fill the prescription.
In Mexico, Colombia and probably other Latin American countries, this drug is of restricted use, and an official identification and patient signature is required by the pharmacies.
Dosage
The dose of isotretinoin a patient receives is dependent on their weight and the severity of the condition. High dose treatments are administered between 0.5 mg/kg/day to 2 mg/kg/day (usually at 0.5 to 1 mg/kg/day[10], divided into two doses), for a total treatment of 4–6 months. A second course may be used two months following the cessation of the initial course if severe acne recurs. Efficacy appears to be related to the cumulative dose of isotretinoin taken, with a total cumulative dose of 120–150 mg/kg used as a guideline.[5][6] High dose treatments should only be used as a last resort due to adverse side effects.
Other studies show that lower dosage treatments are just as effective.[11][12] In these experiments, subjects used 20mg/day, which is 0.25 mg/kg/day for an 80 kg (176 pounds) person.
More experiments and studies showing the success of low dosage treatments with diminished or non-existent side effects:
http://www.uspharmacist.com/oldformat.asp?url=newlook/files/Feat/apr00iso.cfm&pub_id=8&article_id=508
http://www.blackwell-synergy.com/doi/abs/10.1111/j.1365-4362.1994.tb01500.x
http://www.blackwell-synergy.com/doi/abs/10.1111/j.1468-3083.1998.tb00763.x
http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowFulltext&ProduktNr=223854&Ausgabe=227284&ArtikelNr=45270
Preparations
Isotretinoin is marketed under many brand names by various manufacturers. It is typically available as 5 mg, 10 mg, 20 mg, 30mg and (in the USA) 40 mg capsules. Some brands of oral isotretinoin include: Accure (Alphapharm), Accutane and Roaccutane (Roche), Aknenormin (Hermal), Amnesteem (Mylan), Ciscutan (Pelpharma), Claravis (Barr), Clarus (Prepharm), Isohexal (Hexal Australia), Isotane (Pacific Pharmaceuticals), Isotroin (Cipla), Oratane (Douglas Pharmaceuticals), and Sotret (Ranbaxy).
It is also available as a 0.05% topical preparation, marketed by Stiefel under the trade name Isotrex or Isotrexin (with erythromycin).
Adverse effects
Increasingly higher dosages will result in higher toxicity, resembling vitamin A toxicity. Adverse drug reactions associated with isotretinoin therapy include:[5]
- Common: Mild acne flare, dryness of skin, lips and mucous membranes, infection of the cuticles, cheilitis, itch, skin fragility, skin peeling, rash, flushing, photosensitivity, nose bleeds, dry eyes, eye irritation, conjunctivitis, reduced tolerance to contact lenses, hyperlipidaemia, raised liver enzymes, headaches, hair thinning (This could start or continue after treatment), myalgia and/or arthralgia, back pain.
- Infrequent: severe acne flare, raised blood glucose level, increased erythrocyte sedimentation rate, fatigue.
- Rare: impaired night vision; cataracts; optic neuritis; menstrual disturbances; inflammatory bowel disease; pancreatitis; hepatitis; corneal opacities; papilloedema; idiopathic intracranial hypertension; skeletal hyperostosis; extraosseous calcification; psychosis; and it is believed that severe depression can occur, although there is no conclusive evidence for this.
The following adverse effects have been reported to persist, even after discontinuing therapy: alopecia (hair loss), arthralgias, decreased night vision, inflammatory bowel disease, degenerative disc disease, keloids, bone disease. High dosages of isotretinoin have been reported to cause rosacea (a disease of severe facial skin redness and irritation).
Erectile dysfunction in the form of difficulty in maintaining erection was reported in several patients in a clinical study. The impotence may have been caused by the psychiatric side effects of isotretinoin.[13] Despite this, sexual dysfunction is not acknowledged as a side-effect in the official literature accompanying the medication.
While vitamin E supplements have been advocated by some to reduce the toxicity of high-dose retinoids without reducing drug efficacy, test results have proven this to be false (though no indication of what form of vitamin E was used).[14]
Patients with degenerative conditions, such as Muscular Dystrophy, should not take isotretinoin as it may exacerbate and/or accelerate the underlying condition. This may be due to a suspected effect similar to accelerated aging on the skin and tissues of the body, including muscle fibers.
Patients receiving isotretinoin therapy are not permitted to donate blood during and for at least one month after discontinuation of isotretinoin therapy due to reported birth defects to unborn children.
Patients that get a tattoo while on this medication might get scarring on the tattoed area, and also rejection of the ink .
Teratogenicity (Birth Defects)
Isotretinoin is a teratogen and is highly likely to cause birth defects if taken during pregnancy. A few of the more common birth defects that this drug can cause are hearing and visual impairment, missing earlobes, facial dysmorphism, and mental retardation. Isotretinoin is classified as FDA Pregnancy Category X and ADEC Category X, and use is contraindicated in pregnancy.[6]
The manufacturer recommends that pregnancy be excluded in female patients two weeks prior to commencement of isotretinoin, and that they should use effective contraception (sometimes two simultaneous forms are recommended) at least one month prior to commencement, during, and for at least one month following isotretinoin therapy.[15]
In the U.S. more than 2,000 women have become pregnant while taking the drug between 1982 and 2003, with most pregnancies ending in abortion or miscarriage. About 160 babies with birth defects were born. Consequently, the iPLEDGE program was introduced by the U.S. Food and Drug Administration on 12 August 2005 in an attempt to ensure that female patients receiving isotretinoin do not become pregnant – as of 1 March 2006, only prescribers registered and activated in iPLEDGE are able to prescribe isotretinoin, and only patients registered and qualified in iPLEDGE will be able to have isotretinoin dispensed.
Depression
Several studies have suggested a possible link between isotretinoin and clinical depression.[16][17] However, no conclusive evidence has been produced. Despite this, the argument that isotretinoin caused depression and suicide has won a few lawsuits, and is partially responsible for the strict control of the drug, especially in the United States. Various case reports of depression, suicidal ideation, suicide attempt, and suicide in patients treated with isotretinoin have been reported to the U.S. FDA Adverse Events Reporting System, with 431 cases reported between 1982 and May 2001 – of these 37 patients had committed suicide.[18] While analyses have suggested an association between isotretinoin therapy and depression, no causal relationship has been established and further studies are required.[19][20]
Studies have shown that patients with acne, the population group eligible to receive isotretinoin therapy, have an increased risk of clinical depression compared with the general population.[21][22] Chee Hong describes Isotretinoin-related depression as "an idiosyncratic side-effect", claiming, often anxiety can bring on acne and depression, creating more anxiety.[23] Correspondingly, treatment of severe acne with isotretinoin has been shown to reduce anxiety and depression, for tests have shown acne to be a main depressant in most tested patients' lives.[24][25]
One study utilising positron emission tomography (PET) showed functional brain imaging changes in patients treated with isotretinoin, however the clinical relevance of this finding is unclear.[26]
U.S. Representative Bart Stupak (D-MI) is known for his distrust of Accutane. He believes unadvertised psychological side effects from the drug drove his teenage son, Bartholomew Thomas "B.J" Stupak Jr., to commit suicide in 2000.
Psychological effects
In addition to possible anxiety, several studies have shown that male patients taking isotretinoin show increased sensitivity to testosterone, and related psychological effects such as unusual irritability, over-inflated self-confidence and increased sexual desire. It should be noted that none of these symptoms have been known to last more than one month after the end of the treatment. Am J Psychiatry 2007;122(5):996-67. PMID 16363402
Crohn's Disease and Ulcerative colitis
Several scientific studies have posited that isotretinoin is a probable cause of Crohn's Disease and Ulcerative colitis in some individuals. Three cases in the United States have gone to trial thus far, with all three resulting in multi-million dollar judgments against the makers of isotretinoin; there are an additional 425 cases pending. [1] [27] [28] [29] [2]
Drug interactions
The concurrent use of isotretinoin with tetracycline antibiotics or vitamin A supplementation is not recommended. Concurrent use of isotretinoin with tetracyclines significantly increases the risk of idiopathic intracranial hypertension. Concurrent intake of Vitamin A supplementation increases the risk of vitamin A toxicity.[6]
Concurrent use of isotretinoin with methotrexate increases the risk of hepatotoxicity and may increase methotrexate levels. The combination is used with caution and close monitoring of adverse effects and liver function tests.[5]
See also
- Tazarotene
- Hypervitaminosis A syndrome
References
- ↑ isotretinoin - Definitions from Dictionary.com
- ↑ 2.0 2.1 Bérard A, Azoulay L, Koren G, Blais L, Perreault S, Oraichi D (2007). "Isotretinoin, pregnancies, abortions and birth defects: a population-based perspective". British journal of clinical pharmacology 63 (2): 196–205. doi:. PMID 17214828.
- ↑ Holmes SC, Bankowska U, Mackie RM (1998). "The prescription of isotretinoin to women: is every precaution taken?". Br. J. Dermatol. 138 (3): 450–5. doi:. PMID 9580798.
- ↑ DrugBank database - Isotretinoin (APRD00140), 12 November 2006, University of Alberta, accessed January 2007
- ↑ 5.0 5.1 5.2 5.3 Rossi S (2006). Australian medicines handbook 2006. Adelaide, S. Aust: Australian Medicines Handbook Pty Ltd. ISBN 0-9757919-2-3.
- ↑ 6.0 6.1 6.2 6.3 6.4 Klasco RK, editor. Drugdex system, vol. 128. Greenwood Village (CO): Thomson Micromedex; 2006.
- ↑ Joint Formulary Committee. British National Formulary. 47th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain. ISBN 0-85369-584-9
- ↑ James M (Jun 1996). "Isotretinoin for severe acne". Lancet 347 (9017): 1749–50. PMID 8656912.
- ↑ Pharmaceutical Services Branch. Guide to poisons and therapeutic goods legislation for medical practitioners and dentists. Sydney: NSW Department of Health; 2006.
- ↑ United States Pharmacopeia Staff. Consumer Reports Complete Drug Reference. Yonkers, NY: Consumer Reports Books, 1995. Pg 998.
- ↑ Amichai B, Shemer A, Grunwald M (2006). "Low-dose isotretinoin in the treatment of acne vulgaris". J Am Acad Dermatol 54 (4): 644–6. doi:. PMID 16546586. Summary of study results
- ↑ Seukeran D, Cunliffe W (1998). "Acne vulgaris in the elderly: the response to low-dose isotretinoin". Br J Dermatol 139 (1): 99–101. doi:. PMID 9764156.
- ↑ Tirado Sánchez A; León Dorantes G. (Nov-Dec 2005). "[Erectile dysfunction during isotretinoin therapy]". Actas urologicas españolas. 29 (10): 974–6. PMID 16447596.
- ↑ Kus S, Gün D, Demirçay Z, Sur H (Mar 2005). "Vitamin E does not reduce the side-effects of isotretinoin in the treatment of acne vulgaris". Int J Dermatol. 44 (3): 248–51. doi:. PMID 15807739.
- ↑ Roche Products Pty Ltd. Roaccutane (Australian Approved Product Information). Dee Why (NSW): Roche; 2005.
- ↑ O'Donnell J (2003). "Overview of existing research and information linking isotretinoin (accutane), depression, psychosis, and suicide". Am J Ther 10 (2): 148–59. PMID 12629595. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=1075-2765&volume=10&issue=2&spage=148.
- ↑ Bremner JD (2003). "Does isotretinoin cause depression and suicide?". Psychopharmacol Bull 37 (1): 64–78. PMID 14561949. http://www.medworksmedia.com/psychopharmbulletin/pdf/12/064-078_PB%20W3_Bremner_fin.pdf.
- ↑ Wysowski DK, Pitts M, Beitz J (Oct 2001). "An analysis of reports of depression and suicide in patients treated with isotretinoin". J Am Acad Dermatol. 45 (4): 515–9. doi:. PMID 11568740.
- ↑ Ng CH, Schweitzer I (Feb 2003). "The association between depression and isotretinoin use in acne". Aust N Z J Psychiatry 37 (1): 78–84. PMID 12534661. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0004-8674&date=2003&volume=37&issue=1&spage=78.
- ↑ Hull PR, D'Arcy C (2003). "Isotretinoin use and subsequent depression and suicide: presenting the evidence". Am J Clin Dermatol 4 (7): 493–505. PMID 12814338.
- ↑ Gupta MA, Gupta AK (Nov 1998). "Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis". Br J Dermatol. 139 (5): 846–50. PMID 9892952. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0007-0963&date=1998&volume=139&issue=5&spage=846.
- ↑ Niemeier V, Kupfer J, Demmelbauer-Ebner M, Stangier U, Effendy I, Gieler U (1998). "Coping with acne vulgaris. Evaluation of the chronic skin disorder questionnaire in patients with acne". Dermatology (Basel) 196 (1): 108–15. PMID 9557243. http://content.karger.com/produktedb/produkte.asp?typ=fulltext&file=drm96108.
- ↑ Ng CH, Schweitzer I (Feb 2003). "The association between depression and isotretinoin use in acne". Aust N Z J Psychiatry 37 (1): 78–84. doi:. PMID 12534661. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0004-8674&date=2003&volume=37&issue=1&spage=78.
- ↑ Rubinow DR, Peck GL, Squillace KM, Gantt GG (Jul 1987). "Reduced anxiety and depression in cystic acne patients after successful treatment with oral isotretinoin". J Am Acad Dermatol. 17 (1): 25–32. PMID 2956296.
- ↑ Chia CY, Lane W, Chibnall J, Allen A, Siegfried E (May 2005). "Isotretinoin therapy and mood changes in adolescents with moderate to severe acne: a cohort study". Arch Dermatol 141 (5): 557–60. doi:. PMID 15897376.
- ↑ Bremner JD, Fani N, Ashraf A, et al (May 2005). "Functional brain imaging alterations in acne patients treated with isotretinoin". Am J Psychiatry 162 (5): 983–91. doi:. PMID 15863802.
- ↑ Reddy D, Siegel CA, Sands BE, Kane S (Jul 2006). "Possible association between isotretinoin and inflammatory bowel disease". Am J Gastroenterol. 101 (7): 1569–73. doi:. PMID 16863562.
- ↑ Borobio E, Arín A, Valcayo A, Iñarrairaegui M, Nantes O, Prieto C (2004). "[Isotretinoin and ulcerous colitis]" (in Spanish; Castilian). An Sist Sanit Navar 27 (2): 241–3. PMID 15381956.
- ↑ Reniers DE, Howard JM (Oct 2001). "Isotretinoin-induced inflammatory bowel disease in an adolescent". Ann Pharmacother 35 (10): 1214–6. PMID 11675849. http://www.theannals.com/cgi/pmidlookup?view=long&pmid=11675849.
External links
- Hoffmann-La Roche (Makers of (Ro) accutane)
- FDA's Accutane Information Page
- FDA distributed "Accutane Medication Guide"
- Drugs.com Isotretinoin Information
- Dermatology Vol 9: issue 5: Night blindness, vitamin A deficiency, and isotretinoin psychotoxicity
- DermNet treatments/isotretinoin
- Practical Guide to Accutane Side Effects, vitminA.org
|
|||||||||||||||||||||||