Hormone
Hormones (from Greek ὁρμή - "impetus") are chemicals released by cells that affect cells in other parts of the body. Only a small amount of hormone is required to alter cell metabolism. It is also a chemical messenger that transports a signal from one cell to another. All multicellular organisms produce hormones; plant hormones are also called phytohormones. Hormones in animals are often transported in the blood. Cells respond to a hormone when they express a specific receptor for that hormone. The hormone binds to the receptor protein, resulting in the activation of a signal transduction mechanism that ultimately leads to cell type-specific responses.
Endocrine hormone molecules are secreted (released) directly into the bloodstream, while exocrine hormones (or ectohormones) are secreted directly into a duct, and from the duct they either flow into the bloodstream or they flow from cell to cell by diffusion in a process known as paracrine signalling.
Contents |
Hierarchical nature of hormonal control
Hormonal regulation of some physiological activities involves a hierarchy of cell types acting on each other either to stimulate or to modulate the release and action of a particular hormone. The secretion of hormones from successive levels of endocrine cells is stimulated by chemical signals originating from cells higher up the hierarchical system. The master coordinator of hormonal activity in mammals is the hypothalamus, which acts on input that it receives from the central nervous system.[1]
Other hormone secretion occurs in response to local conditions, such as the rate of secretion of parathyroid hormone by the parathyroid cells in response to fluctuations of ionized calcium levels in extracellular fluid.
Hormone signaling
Hormonal signaling across this hierarchy involves the following:
- Biosynthesis of a particular hormone in a particular tissue
- Storage and secretion of the hormone
- Transport of the hormone to the target cell(s)
- Recognition of the hormone by an associated cell membrane or intracellular receptor protein.
- Relay and amplification of the received hormonal signal via a signal transduction process: This then leads to a cellular response. The reaction of the target cells may then be recognized by the original hormone-producing cells, leading to a down-regulation in hormone production. This is an example of a homeostatic negative feedback loop.
- Degradation of the hormone.
As can be inferred from the hierarchical diagram, hormone biosynthetic cells are typically of a specialized cell type, residing within a particular endocrine gland (e.g., the thyroid gland, the ovaries, or the testes). Hormones may exit their cell of origin via exocytosis or another means of membrane transport. However, the hierarchical model is an oversimplification of the hormonal signaling process. Cellular recipients of a particular hormonal signal may be one of several cell types that reside within a number of different tissues, as is the case for insulin, which triggers a diverse range of systemic physiological effects. Different tissue types may also respond differently to the same hormonal signal. Because of this, hormonal signaling is elaborate and hard to dissect.
Interactions with receptors
Most hormones initiate a cellular response by initially combining with either a specific intracellular or cell membrane associated receptor protein. A cell may have several different receptors that recognize the same hormone and activate different signal transduction pathways, or alternatively different hormones and their receptors may invoke the same biochemical pathway.
For many hormones, including most protein hormones, the receptor is membrane associated and embedded in the plasma membrane at the surface of the cell. The interaction of hormone and receptor typically triggers a cascade of secondary effects within the cytoplasm of the cell, often involving phosphorylation or dephosphorylation of various other cytoplasmic proteins, changes in ion channel permeability, or increased concentrations of intracellular molecules that may act as secondary messengers (e.g. cyclic AMP). Some protein hormones also interact with intracellular receptors located in the cytoplasm or nucleus by an intracrine mechanism.
For hormones such as steroid or thyroid hormones, their receptors are located intracellularly within the cytoplasm of their target cell. In order to bind their receptors these hormones must cross the cell membrane. The combined hormone-receptor complex then moves across the nuclear membrane into the nucleus of the cell, where it binds to specific DNA sequences, effectively amplifying or suppressing the action of certain genes, and affecting protein synthesis.[2] However, it has been shown that not all steroid receptors are located intracellularly, some are plasma membrane associated.[3]
An important consideration, dictating the level at which cellular signal transduction pathways are activated in response to a hormonal signal is the effective concentration of hormone-receptor complexes that are formed. Hormone-receptor complex concentrations are effectively determined by three factors:
- The number of hormone molecules available for complex formation
- The number of receptor molecules available for complex formation and
- The binding affinity between hormone and receptor.
The number of hormone molecules available for complex formation is usually the key factor in determining the level at which signal transduction pathways are activated. The number of hormone molecules available being determined by the concentration of circulating hormone, which is in turn influenced by the level and rate at which they are secreted by biosynthetic cells. The number of receptors at the cell surface of the receiving cell can also be varied as can the affinity between the hormone and its receptor.
Physiology of hormones
Most cells are capable of producing one or more molecules, which act as signaling molecules to other cells, altering their growth, function, or metabolism. The classical hormones produced by cells in the endocrine glands mentioned so far in this article are cellular products, specialized to serve as regulators at the overall organism level. However they may also exert their effects solely within the tissue in which they are produced and originally released.
The rate of hormone biosynthesis and secretion is often regulated by a homeostatic negative feedback control mechanism. Such a mechanism depends on factors which influence the metabolism and excretion of hormones. Thus, higher hormone concentration alone can not trigger the negative feedback mechanism. Negative feedback must be triggered by overproduction of an "effect" of the hormone.
Hormone secretion can be stimulated and inhibited by:
- Other hormones (stimulating- or releasing-hormones)
- Plasma concentrations of ions or nutrients, as well as binding globulins
- Neurons and mental activity
- Environmental changes, e.g., of light or temperature
One special group of hormones is the tropic hormones that stimulate the hormone production of other endocrine glands. For example, thyroid-stimulating hormone (TSH) causes growth and increased activity of another endocrine gland, the thyroid, which increases output of thyroid hormones.
A recently-identified class of hormones is that of the "hunger hormones" - ghrelin, orexin and PYY 3-36 - and "satiety hormones" - e.g., leptin, obestatin, nesfatin-1.
In order to release active hormones quickly into the circulation, hormone biosynthetic cells may produce and store biologically inactive hormones in the form of pre- or prohormones. These can then be quickly converted into their active hormone form in response to a particular stimulus.
Hormone effects
Hormone effects vary widely, but can include:
- stimulation or inhibition of growth,
- In puberty hormones can affect mood and mind
- induction or suppression of apoptosis (programmed cell death)
- activation or inhibition of the immune system
- regulating metabolism
- preparation for a new activity (e.g., fighting, fleeing, mating)
- preparation for a new phase of life (e.g., puberty, caring for offspring, menopause)
- controlling the reproductive cycle
In many cases, one hormone may regulate the production and release of other hormones
Many of the responses to hormone signals can be described as serving to regulate metabolic activity of an organ or tissue.
Chemical classes of hormones
Vertebrate hormones fall into three chemical classes:
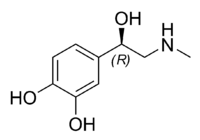
- Amine-derived hormones are derivatives of the amino acids tyrosine and tryptophan. Examples are catecholamines and thyroxine.
- Peptide hormones consist of chains of amino acids. Examples of small peptide hormones are TRH and vasopressin. Peptides composed of scores or hundreds of amino acids are referred to as proteins. Examples of protein hormones include insulin and growth hormone. More complex protein hormones bear carbohydrate side chains and are called glycoprotein hormones. Luteinizing hormone, follicle-stimulating hormone and thyroid-stimulating hormone are glycoprotein hormones.
- Lipid and phospholipid-derived hormones derive from lipids such as linoleic acid and arachidonic acid and phospholipids. The main classes are the steroid hormones that derive from cholesterol and the eicosanoids. Examples of steroid hormones are testosterone and cortisol. Sterol hormones such as calcitriol are a homologous system. The adrenal cortex and the gonads are primary sources of steroid hormones. Examples of eicosanoids are the widely studied prostaglandins.
Pharmacology
Many hormones and their analogues are used as medication. The most commonly-prescribed hormones are estrogens and progestagens (as methods of hormonal contraception and as HRT), thyroxine (as levothyroxine, for hypothyroidism) and steroids (for autoimmune diseases and several respiratory disorders). Insulin is used by many diabetics. Local preparations for use in otolaryngology often contain pharmacologic equivalents of adrenaline, while steroid and vitamin D creams are used extensively in dermatological practice.
A "pharmacologic dose" of a hormone is a medical usage referring to an amount of a hormone far greater than naturally occurs in a healthy body. The effects of pharmacologic doses of hormones may be different from responses to naturally-occurring amounts and may be therapeutically useful. An example is the ability of pharmacologic doses of glucocorticoid to suppress inflammation.
Important human hormones
Spelling is not uniform for many hormones. Current North American and international usage is estrogen, gonadotropin, while British usage retains the Greek diphthong in oestrogen and favors the earlier spelling gonadotrophin (from trophē ‘nourishment, sustenance’ rather than tropē ‘turning, change’.
| Structure | Name | Abbrev- iation |
Tissue | Cells | Mechanism | Target Tissue | Effect |
| amine - tryptophan | Melatonin (N-acetyl-5-methoxytryptamine) | pineal gland | pinealocyte | antioxidant and causes drowsiness | |||
| amine - tryptophan | Serotonin | 5-HT | CNS, GI tract | enterochromaffin cell | Controls mood, appetite, and sleep | ||
| amine - tyrosine | Thyroxine (or tetraiodothyronine) (a thyroid hormone) | T4 | thyroid gland | thyroid epithelial cell | direct | less active form of thyroid hormone: increase the basal metabolic rate & sensitivity to catecholamines,
affect protein synthesis |
|
| amine - tyrosine | Triiodothyronine (a thyroid hormone) | T3 | thyroid gland | thyroid epithelial cell | direct | potent form of thyroid hormone: increase the basal metabolic rate & sensitivity to catecholamines,
affect protein synthesis |
|
| amine - tyrosine (cat) | Epinephrine (or adrenaline) | EPI | adrenal medulla | chromaffin cell | Fight-or-flight response:
Boosts the supply of oxygen and glucose to the brain and muscles (by increasing heart rate and stroke volume, vasodilation, increasing catalysis of glycogen in liver, breakdown of lipids in fat cells. dilate the pupils Suppress non-emergency bodily processes (e.g. digestion) Suppress immune system |
||
| amine - tyrosine (cat) | Norepinephrine (or noradrenaline) | NRE | adrenal medulla | chromaffin cell | Fight-or-flight response:
Boosts the supply of oxygen and glucose to the brain and muscles (by increasing heart rate and stroke volume, vasoconstriction and increased blood pressure, breakdown of lipids in fat cells. Increase skeletal muscle readiness. |
||
| amine - tyrosine (cat) | Dopamine (or prolactin inhibiting hormone | DPM, PIH or DA | kidney, hypothalamus | Chromaffin cells in kidney Dopamine neurons of the arcuate nucleus in hypothalamus |
Increase heart rate and blood pressure Inhibit release of prolactin and TRH from anterior pituitary |
||
| peptide | Antimullerian hormone (or mullerian inhibiting factor or hormone) | AMH | testes | Sertoli cell | Inhibit release of prolactin and TRH from anterior pituitary | ||
| peptide | Adiponectin | Acrp30 | adipose tissue | ||||
| peptide | Adrenocorticotropic hormone (or corticotropin) | ACTH | anterior pituitary | corticotrope | cAMP | synthesis of corticosteroids (glucocorticoids and androgens) in adrenocortical cells | |
| peptide | Angiotensinogen and angiotensin | AGT | liver | IP3 | vasoconstriction
release of aldosterone from adrenal cortex dipsogen. |
||
| peptide | Antidiuretic hormone (or vasopressin, arginine vasopressin) | ADH | posterior pituitary | Parvocellular neurosecretory neurons in hypothalamus Magnocellular neurosecretory cells in posterior pituitary |
varies | retention of water in kidneys moderate vasoconstriction Release ACTH in anterior pituitary |
|
| peptide | Atrial-natriuretic peptide (or atriopeptin) | ANP | heart | cGMP | |||
| peptide | Calcitonin | CT | thyroid gland | parafollicular cell | cAMP | Construct bone, reduce blood Ca2+ | |
| peptide | Cholecystokinin | CCK | duodenum | Release of digestive enzymes from pancreas
Release of bile from gallbladder hunger suppressant |
|||
| peptide | Corticotropin-releasing hormone | CRH | hypothalamus | cAMP | Release ACTH from anterior pituitary | ||
| peptide | Erythropoietin | EPO | kidney | Extraglomerular mesangial cells | Stimulate erythrocyte production | ||
| peptide | Follicle-stimulating hormone | FSH | anterior pituitary | gonadotrope | cAMP | In female: stimulates maturation of Graafian follicles in ovary.
In male: spermatogenesis, enhances production of androgen-binding protein by the Sertoli cells of the testes |
|
| peptide | Gastrin | GRP | stomach, duodenum | G cell | Secretion of gastric acid by parietal cells | ||
| peptide | Ghrelin | stomach | P/D1 cell | Stimulate appetite,
secretion of growth hormone from anterior pituitary gland |
|||
| peptide | Glucagon | GCG | pancreas | alpha cells | cAMP | glycogenolysis and gluconeogenesis in liver
increases blood glucose level |
|
| peptide | Gonadotropin-releasing hormone | GnRH | hypothalamus | IP3 | Release of FSH and LH from anterior pituitary. | ||
| peptide | Growth hormone-releasing hormone | GHRH | hypothalamus | IP3 | Release GH from anterior pituitary | ||
| peptide | Human chorionic gonadotropin | hCG | placenta | syncytiotrophoblast cells | cAMP | promote maintenance of corpus luteum during beginning of pregnancy
Inhibit immune response, towards the human embryo. |
|
| peptide | Human placental lactogen | HPL | placenta | increase production of insulin and IGF-1
increase insulin resistance and carbohydrate intolerance |
|||
| peptide | Growth hormone | GH or hGH | anterior pituitary | somatotropes | stimulates growth and cell reproduction
Release Insulin-like growth factor 1 from liver |
||
| peptide | Inhibin | testes, ovary, fetus | Sertoli cells of testes granulosa cells of ovary trophoblasts in fetus |
anterior pituitary | Inhibit production of FSH | ||
| peptide | Insulin | INS | pancreas | beta cells | tyrosine kinase | Intake of glucose, glycogenesis and glycolysis in liver and muscle from blood
intake of lipids and synthesis of triglycerides in adipocytes Other anabolic effects |
|
| peptide | Insulin-like growth factor (or somatomedin) | IGF | liver | Hepatocytes | tyrosine kinase | insulin-like effects
regulate cell growth and development |
|
| peptide | Leptin | LEP | adipose tissue | decrease of appetite and increase of metabolism. | |||
| peptide | Luteinizing hormone | LH | anterior pituitary | gonadotropes | cAMP | In female: ovulation
In male: stimulates Leydig cell production of testosterone |
|
| peptide | Melanocyte stimulating hormone | MSH or α-MSH | anterior pituitary/pars intermedia | Melanotroph | cAMP | melanogenesis by melanocytes in skin and hair | |
| peptide | Orexin | hypothalamus | wakefulness and increased energy expenditure, increased appetite | ||||
| peptide | Oxytocin | OXT | posterior pituitary | Magnocellular neurosecretory cells | IP3 | release breast milk
Contraction of cervix and vagina Involved in orgasm, trust between people.[4] and circadian homeostasis (body temperature, activity level, wakefulness) [5]. |
|
| peptide | Parathyroid hormone | PTH | parathyroid gland | parathyroid chief cell | cAMP | increase blood Ca2+: *indirectly stimulate osteoclasts
(Slightly) decrease blood phosphate:
|
|
| peptide | Prolactin | PRL | anterior pituitary, uterus | lactotrophs of anterior pituitary Decidual cells of uterus |
milk production in mammary glands sexual gratification after sexual acts |
||
| peptide | Relaxin | RLN | uterus | Decidual cells | Unclear in humans | ||
| peptide | Secretin | SCT | duodenum | S cell | Secretion of bicarbonate from liver, pancreas and duodenal Brunner's glands
Enhances effects of cholecystokinin Stops production of gastric juice |
||
| peptide | Somatostatin | SRIF | hypothalamus, islets of Langerhans, gastrointestinal system | delta cells in islets Neuroendocrince cells of the Periventricular nucleus in hypothalamus |
Inhibit release of GH and TRH from anterior pituitary Suppress release of gastrin, cholecystokinin (CCK), secretin, motilin, vasoactive intestinal peptide (VIP), gastric inhibitory polypeptide (GIP), enteroglucagon in gastrointestinal system Lowers rate of gastric emptying Reduces smooth muscle contractions and blood flow within the intestine [6] |
||
| peptide | Thrombopoietin | TPO | liver, kidney, striated muscle | Myocytes | megakaryocytes | produce platelets[8] | |
| peptide | Thyroid-stimulating hormone (or thyrotropin) | TSH | anterior pituitary | thyrotropes | cAMP | thyroid gland | secrete thyroxine (T4) and triiodothyronine (T3) |
| peptide | Thyrotropin-releasing hormone | TRH | hypothalamus | Parvocellular neurosecretory neurons | IP3 | anterior pituitary | Release thyroid-stimulating hormone (primarily) Stimulate prolactin release |
| steroid - glu. | Cortisol | adrenal cortex (zona fasciculata and zona reticularis cells) | direct | Stimulation of gluconeogenesis
Inhibition of glucose uptake in muscle and adipose tissue Mobilization of amino acids from extrahepatic tissues Stimulation of fat breakdown in adipose tissue anti-inflammatory and immunosuppressive |
|||
| steroid - min. | Aldosterone | adrenal cortex (zona glomerulosa) | direct | Increase blood volume by reabsorption of sodium in kidneys (primarily)
Potassium and H+ secretion in kidney. |
|||
| steroid - sex (and) | Testosterone | testes | Leydig cells | direct | Anabolic: growth of muscle mass and strength, increased bone density, growth and strength,
Virilizing: maturation of sex organs, formation of scrotum, deepening of voice, growth of beard and axillary hair. |
||
| steroid - sex (and) | Dehydroepiandrosterone | DHEA | testes, ovary, kidney | Zona fasciculata and Zona reticularis cells of kidney theca cells of ovary Leydig cellss of testes |
direct | Virilization, anabolic | |
| steroid - sex (and) | Androstenedione | adrenal glands, gonads | direct | Substrate for estrogen | |||
| steroid - sex (and) | Dihydrotestosterone | DHT | multiple | direct | |||
| steroid - sex (est) | Estradiol | E2 | females: ovary, males testes | females: granulosa cells, males: Sertoli cell | direct | Females:
Structural:
Protein synthesis:
Increase HDL, triglyceride, height growth Decrease LDL, fat deposition Fluid balance:
Gastrointestinal tract:
Melanin:
Cancer: support hormone-sensitive breast cancers [9] Suppression of production in the body of estrogen is a treatment for these cancers. Lung function:
|
|
| steroid - sex (est) | Estrone | ovary | granulosa cells, Adipocytes | direct | |||
| steroid - sex (est) | Estriol | placenta | syncytiotrophoblast | direct | |||
| steroid - sex (pro) | Progesterone | ovary, adrenal glands, placenta (when pregnant) | Granulosa cells theca cells of ovary | direct | Support pregnancy[12]:
Convert endometrium to secretory stage Make cervical mucus permeable to sperm. Inhibit immune response, e.g. towards the human embryo. Decrease uterine smooth muscle contractility[12] Inhibit lactation Inhibit onset of labor. Support fetal production of adrenal mineralo- and glucosteroids. Other: Raise epidermal growth factor-1 levels Increase core temperature during ovulation[13] Reduce spasm and relax smooth muscle (widen bronchi and regulate mucus) Antiinflammatory Reduce gall-bladder activity[14] Normalize blood clotting and vascular tone, zinc and copper levels, cell oxygen levels, and use of fat stores for energy. Assist in thyroid function and bone growth by osteoblasts Relsilience in bone, teeth, gums, joint, tendon, ligament and skin Healing by regulating collagen Nerve function and healing by regulating myelin Prevent endometrial cancer by regulating effects of estrogen. |
||
| sterol | Calcitriol (1,25-dihydroxyvitamin D3) | skin/proximal tubule of kidneys | direct | Active form of vitamin D3
Increase absorption of calcium and phosphate from gastrointestinal tract and kidneys inhibit release of PTH |
|||
| sterol | Calcidiol (25-hydroxyvitamin D3) | skin/proximal tubule of kidneys | direct | Inactive form of Vitamin D3 | |||
| eicosanoid | Prostaglandins | PG | seminal vesicle | ||||
| eicosanoid | Leukotrienes | LT | white blood cells | ||||
| eicosanoid | Prostacyclin | PGI2 | endothelium | ||||
| eicosanoid | Thromboxane | TXA2 | platelets | ||||
| Prolactin releasing hormone | PRH | hypothalamus | Release prolactin from anterior pituitary | ||||
| Lipotropin | PRH | anterior pituitary | Corticotropes | lipolysis and steroidogenesis, stimulates melanocytes to produce melanin |
|||
| Brain natriuretic peptide | BNP | heart | Cardiac myocytes | (To a minor degree than ANP) reduce blood pressure by:
reducing systemic vascular resistance, reducing blood water, sodium and fats |
|||
| Neuropeptide Y | NPY | Stomach | increased food intake and decreased physical activity | ||||
| Histamine | Stomach | ECL cells | stimulate gastric acid secretion | ||||
| Endothelin | Stomach | X cells | Smooth muscle contraction of stomach [15] | ||||
| Pancreatic polypeptide | Pancreas | PP cells | Unknown | ||||
| Renin | Kidney | Juxtaglomerular cells | Activates the renin-angiotensin system by producing angiotensin I of angiotensinogen | ||||
| Enkephalin | Kidney | Chromaffin cells | Regulate pain |
References
- ↑ Mathews, CK and van Holde, K. E. (1990). "Integration and control of metabolic processes". in Bowen, D.. Biochemistry. The Benjamin/Cummings publishing group. pp. 790–792. ISBN 0-8053-5015-2. OCLC 20352437.
- ↑ Beato M, Chavez S and Truss M (1996). "Transcriptional regulation by steroid hormones". Steroids 61 (4): 240–251. doi:. PMID 8733009.
- ↑ Hammes SR (2003). "The further redefining of steroid-mediated signaling". Proc Natl Acad Sci USA 100 (5): 21680–2170. doi:. PMID 12606724.
- ↑ Kosfeld M et al. (2005) Oxytocin increases trust in humans. Nature 435:673-676. PDF PMID 15931222
- ↑ Scientific American Mind, "Rhythm and Blues"; June/July 2007; Scientific American Mind; by Ulrich Kraft
- ↑ http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/otherendo/somatostatin.html Colorado State University - Biomedical Hypertextbooks - Somatostatin
- ↑ 7.0 7.1 Physiology at MCG 5/5ch4/s5ch4_17
- ↑ Kaushansky K. Lineage-specific hematopoietic growth factors. N Engl J Med 2006;354:2034-45. PMID 16687716.
- ↑ Hormonal Therapy
- ↑ Massaro D, Massaro GD (2004). "Estrogen regulates pulmonary alveolar formation, loss, and regeneration in mice". American Journal of Physiology. Lung Cellular and Molecular Physiology 287 (6): L1154–9. doi:. PMID 15298854. http://ajplung.physiology.org/cgi/content/full/287/6/L1154.
- ↑ Pentikäinen V, Erkkilä K, Suomalainen L, Parvinen M, Dunkel L. Estradiol Acts as a Germ Cell Survival Factor in the Human Testis in vitro. The Journal of Clinical Endocrinology & Metabolism 2006;85:2057-67 PMID 10843196
- ↑ 12.0 12.1 Placental Hormones
- ↑ Physiology at MCG 5/5ch9/s5ch9_13
- ↑ Hould F, Fried G, Fazekas A, Tremblay S, Mersereau W (1988). "Progesterone receptors regulate gallbladder motility". J Surg Res 45 (6): 505–12. doi:. PMID 3184927.
- ↑ Diabetes-related changes in contractile responses of stomach fundus to endothelin-1 in streptozotocin-induced diabetic rats Journal of Smooth Muscle Research Vol. 41 (2005) , No. 1 35-47. Kazuki Endo1), Takayuki Matsumoto1), Tsuneo Kobayashi1), Yutaka Kasuya1) and Katsuo Kamata1)
See also
- Endocrinology
- Endocrine system
- Neuroendocrinology
- Plant hormones or plant growth regulators
- Autocrine signaling
- Paracrine signaling
- Intracrine
- Cytokine
- Growth factor
- Hormone disruptor
External links
|
|||||||||||||||||||||||||||||||||