Hematocrit
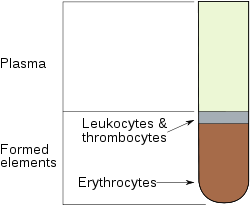
The hematocrit (Ht or HCT) or packed cell volume (PCV) or erythrocyte volume fraction (EVF) is the proportion of blood volume that is occupied by red blood cells. It is normally about 45% for men and 42% for women.[1] It is considered an integral part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count, and platelet count.
In mammals, hematocrit is independent of body size.
HISTORY The term "hematocrit" was coined in 1903. Its roots stem from the Greek words hema (Gr αίμα) - blood, and krites (Gr κριτής), judge - meaning to gauge or judge the blood.
Contents |
Method of measuring

The packed cell volume can be determined by centrifuging heparinized blood in a capillary tube (also known as a microhematocrit tube) at 10,000 RPM for five minutes.[1] This separates the blood into layers. The volume of packed red blood cells, divided by the total volume of the blood sample gives the PCV. Because a tube is used this can be calculated by measuring the lengths of the layers.
With modern lab equipment the hematocrit is calculated by an automated analyzer and not directly measured. It is determined by multiplying the red cell count by the mean cell volume. The hematocrit is slightly more accurate as the PCV includes small amounts of blood plasma trapped between the red cells. An estimated hematocrit as a percentage may be derived by multiplying the hemoglobin concentration in g/dL times three and dropping the units. [2]. The hemoglobin level is the measure used by blood banks.
There have been cases where the blood for testing was inadvertently drawn from the same arm with the intravenous line running in a transfusion of packed red cells. In this sample, the hemoglobin measurement will be high because it is measuring the fluid being transfused (that is, mostly red cells) rather than the diluted serum. In this case, the hematocrit measurement will be artificially very high.
Conversely, if blood for hematology testing is drawn from a site proximal to that of an intravenous line infusing fluids into a patient, the blood sample will be diluted by those fluids and the hematocrit will be artificially low.
Elevated hematocrit
In cases of dengue fever a high hematocrit is a danger sign of an increased risk of dengue shock syndrome.
Polycythemia vera (PV), a myeloproliferative disorder in which the bone marrow produces excessive numbers of red cells, is associated with elevated hematocrit.
Chronic obstructive pulmonary disease (COPD) and other pulmonary conditions associated with hypoxia may elicit an increased production of red blood cells. This increase is mediated by the increased levels of erythropoietin by the kidneys in response to hypoxia.
Professional athletes' hematocrit levels are measured as part of tests for blood doping or Erythropoietin (EPO) use; the level of hematocrit in a blood sample is compared with the long-term level for that athlete (to allow for individual variations in hematocrit level), and against an absolute permitted maximum (which is based on maximum expected levels within the population, and the hematocrit level which causes increased risk of blood clots resulting in strokes or heart attacks).
If a patient is dehydrated, the hematocrit may be elevated. Repeat testing after adequate hydration therapy will usually result in a more reliable result.
Lowered hematocrit
Lowered hematocrit can imply significant hemorrhage (for example, in an ectopic pregnancy.)
The mean corpuscular volume (MCV) and the red cell distribution width (RDW) can be quite helpful in evaluating a lower-than-normal hematocrit, because it can help the clinician determine whether blood loss is chronic or acute. The MCV is the size of the red cells and the RDW is a relative measure of the variation in size of the red cell population. A low hematocrit with a low MCV with a normal RDW suggests a chronic iron-deficient erythropoiesis, but a high RDW suggests a blood loss that is more acute, such as a hemorrhage.
Groups of individuals who are at risk for developing anemia include:
- infants who may not have adequate iron intake
- children going through a rapid growth spurt, during which the iron available cannot keep up with the demands for a growing red cell mass
- women in childbearing years who have an excessive need for iron because of blood loss during menstruation
- pregnant women, in whom the growing fetus creates a high demand for iron.
- patients with chronic kidney disease, as their kidneys no longer secrete sufficient levels of the hormone erythropoietin, which stimulates red blood cell production by the bone marrow.
See also
- Anemia
- Blood tests
- Hematology
- Blood doping
References
- ↑ Purves, William K.; David Sadava, Gordon H. Orians, H. Craig Heller (2004). Life: The Science of Biology (7th ed.). Sunderland, Mass: Sinauer Associates. pp. 954. ISBN 0-7167-9856-5.
|
||||||||||||||||||||||||||||||||||||||