Heart failure
| Heart failure Classification and external resources |
|
 |
|
|---|---|
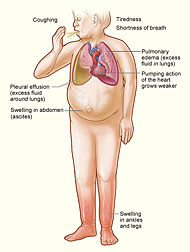
| The major signs and symptoms of heart failure. | |
| ICD-10 | I50.0 |
| ICD-9 | 428.0 |
| DiseasesDB | 16209 |
| MedlinePlus | 000158 |
| eMedicine | med/3552 emerg/108 radio/189 med/1367150 ped/2636 |
| MeSH | D006333 |
Heart failure (HF) is a condition in which a problem with the structure or function of the heart impairs its ability to supply sufficient blood flow to meet the body's needs.[1] It should not be confused with cardiac arrest (see Terminology, below).
Common causes of heart failure include myocardial infarction and other forms of ischemic heart disease, hypertension, valvular heart disease and cardiomyopathy.[2] Heart failure can cause a large variety of symptoms such as shortness of breath (typical worse when lying flat, which is called orthopnea), coughing, ankle swelling and reduced exercise capacity. Heart failure is often undiagnosed due to a lack of a universally agreed definition and challenges in definitive diagnosis. Treatment commonly consist of lifestyle measures (such as decreased salt intake) and medications, and sometimes of devices or even surgery.
Heart failure is a common, costly, disabling and deadly condition.[2] In developing countries, around 2% of adults suffer from heart failure, but in those over the age of 65, this increases to 6—10%.[2][3] Mostly due to costs of hospitalisation, it is associated with a high health expenditure; costs have been estimated to amount to 2% of the total budget of the National Health Service in the United Kingdom, and more than $35 billion in the United States.[4][5] Heart failure is associated with significantly reduced physical and mental health, resulting in a markedly decreased quality of life.[6][7] With the exception of heart failure caused by reversible conditions, the condition usually worsens over time. Although some patients survive many years, progressive disease is associated with an overall annual mortality rate of 10%.[8]
Contents |
Terminology
Heart failure is a global term for the physiological state in which cardiac output is insufficient for the body's needs.
This may occur when the cardiac output is low (often termed "congestive heart failure").[9]
In contrast, it may also occur when the body's requirements are increased, and demand outstrips what the heart can provide, (termed "high output cardiac failure") [10]. This can occur in the context of severe anemia, beriberi (vitamin B1/thiamine deficiency), thyrotoxicosis, Paget's disease, arteriovenous fistulae or arteriovenous malformations.
Fluid overload is a common problem for people with heart failure, but is not synonymous with it. Patients with treated heart failure will often be euvolaemic (a term for normal fluid status), or more rarely, dehydrated.
Doctors use the word "acute" to mean of rapid onset, and "chronic" of long duration. Chronic heart failure is therefore a long term situation, usually with stable treated symptomatology.
Acute decompensated heart failure, which should just describe sudden onset HF, is also used to describe exacerbated or decompensated heart failure, referring to episodes in which a patient with known chronic heart failure abruptly develops symptoms.
There are several terms which are closely related to heart failure, and may be the cause of heart failure, but should not be confused with it:
- Cardiac arrest, and asystole both refer to situations in which there is no cardiac output at all. Without urgent treatment, these result in sudden death.
- Heart attack refers to a blockage in a coronary (heart) artery resulting in heart muscle damage.
- Cardiomyopathy refers specifically to problems within the heart muscle, and these problems usually result in heart failure. Ischemic cardiomyopathy implies that the cause of muscle damage is coronary artery disease. Dilated cardiomyopathy implies that the muscle damage has resulted in enlargement of the heart. Hypertrophic cardiomyopathy involves enlargement and thickening of the heart muscle.
Classification
There are many different ways to categorize heart failure, including:
- the side of the heart involved, (left heart failure versus right heart failure)
- whether the abnormality is due to contraction or relaxation of the heart (systolic dysfunction vs. diastolic dysfunction)
- whether the problem is primarily increased venous back pressure (behind) the heart, or failure to supply adequate arterial perfusion (in front of) the heart (backward vs. forward failure)
- whether the abnormality is due to low cardiac output with high systemic vascular resistance or high cardiac output with low vascular resistance (low-output heart failure vs. high-output heart failure)
- the degree of functional impairment conferred by the abnormality (as in the NYHA functional classification)
Functional classification generally relies on the New York Heart Association Functional Classification.[11] The classes (I-IV) are:
- Class I: no limitation is experienced in any activities; there are no symptoms from ordinary activities.
- Class II: slight, mild limitation of activity; the patient is comfortable at rest or with mild exertion.
- Class III: marked limitation of any activity; the patient is comfortable only at rest.
- Class IV: any physical activity brings on discomfort and symptoms occur at rest.
This score documents severity of symptoms, and can be used to assess response to treatment. While its use is widespread, the NYHA score is not very reproducible and doesn't reliably predict the walking distance or exercise tolerance on formal testing.[12]
In its 2001 guidelines, the American College of Cardiology/American Heart Association working group introduced four stages of heart failure:[13]
- Stage A: Patients at high risk for developing HF in the future but no functional or structural heart disorder;
- Stage B: a structural heart disorder but no symptoms at any stage;
- Stage C: previous or current symptoms of heart failure in the context of an underlying structural heart problem, but managed with medical treatment;
- Stage D: advanced disease requiring hospital-based support, a heart transplant or palliative care.
The ACC staging system is useful in that Stage A encompasses "pre-heart failure" - a stage where intervention with treatment can presumably prevent progression to overt symptoms. ACC stage A does not have a corresponding NYHA class. ACC Stage B would correspond to NYHA Class I. ACC Stage C corresponds to NYHA Class II and III, while ACC Stage D overlaps with NYHA Class IV.
Diagnostic criteria
No system of diagnostic criteria has been agreed as the gold standard for heart failure. Commonly used systems are the "Framingham criteria"[14] (derived from the Framingham Heart Study), the "Boston criteria",[15] the "Duke criteria",[16] and (in the setting of acute myocardial infarction) the "Killip class".[17]
Signs and symptoms
Symptoms
Heart failure symptoms are traditionally and somewhat arbitrarily divided into "left" and "right" sided, recognising that the left and right ventricles of the heart supply different portions of the circulation. This division erroneously implies that the manifestation of failure is predominantly "backward" - with increased venous pressure in the pulmonary circulation for "left" heart failure, and in the systemic circulation for "right" heart failure.
Left sided forward failure overlaps with right sided backward failure. Additionally, the most common cause of right-sided heart failure is left-sided heart failure. The result is that patients commonly present with both sets of signs and symptoms. The division is still however commonly taught to health professionals.
Left-sided failure
Backward failure of the left ventricle causes congestion of the pulmonary vasculature, and so the symptoms are predominantly respiratory in nature. The patient will have dyspnea (shortness of breath) on exertion (dyspnée d'effort) and in severe cases, dyspnea at rest. Increasing breathlessness on reclining, called orthopnea, occurs. It is often measured in the number of pillows required to lie comfortably, and in severe cases, the patient may resort to sleeping while sitting up. Another symptom of heart failure is paroxysmal nocturnal dyspnea, a sudden nighttime attack of severe breathlessness, usually several hours after going to sleep. Easy fatigueability and exercise intolerance are also common complaints related to respiratory compromise.
Compromise of left ventricular forward function may result in symptoms of poor systemic circulation such as dizziness, confusion and cool extremities at rest.
Right-sided failure
Backward failure of the right ventricle leads to congestion of systemic capillaries. This helps to generate excess fluid accumulation in the body. This causes swelling under the skin (termed peripheral edema or anasarca) and usually affects the dependent parts of the body first (causing foot and ankle swelling in people who are standing up, and sacral edema in people who are predominantly lying down). Nocturia (frequent nighttime urination) may occur when fluid from the legs is returned to the bloodstream while lying down at night. In progressively severe cases, ascites (fluid accumulation in the abdominal cavity causing swelling) and hepatomegaly (painful enlargement of the liver) may develop. Significant liver congestion may result in impaired liver function, and jaundice and even coagulopathy (problems of decreased blood clotting) may occur.
Signs
Left-sided failure
Common respiratory signs are tachypnea (increased rate of breathing) and increased work of breathing (non-specific signs of respiratory distress). Rales or crackles, heard initially in the lung bases, and when severe, throughout the lung fields suggest the development of pulmonary edema (fluid in the alveoli). Dullness of the lung fields to finger percussion and reduced breath sounds at the bases of the lung may suggest the development of a pleural effusion (fluid collection in between the lung and the chest wall). Cyanosis which suggests severe hypoxemia, is a late sign of extremely severe pulmonary edema.
Additional signs indicating left ventricular failure include a laterally displaced apex beat (which occurs if the heart is enlarged) and a gallop rhythm (additional heart sounds) may be heard as a marker of increased blood flow, or increased intra-cardiac pressure. Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g. aortic stenosis) or as a result (e.g. mitral regurgitation) of the heart failure.
Right-sided failure
Physical examination can reveal pitting peripheral edema, ascites, and hepatomegaly. Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by the hepatojugular reflux. If the right ventriclar pressure is increased, a parasternal heave may be present, signifying the compensatory increase in contraction strength.
Causes
Chronic Heart Failure
The predominance of causes of heart failure are difficult to analyse due to challenges in diagnosis, differences in populations, and changing prevalence of causes with age.
A 19 year study of 13000 healthy adults in the United States (the National Health and Nutrition Examination Survey (NHANES I) found the following causes ranked by Population Attributable Risk score: [18]
- Ischaemic Heart Disease 62%
- Cigarette Smoking 16%
- Hypertension (high blood pressure)10%
- Obesity 8%
- Diabetes 3%
- Valvular Heart Disease 2% (much higher in older populations)
An Italian registry of over 6200 patients with heart failure showed the following underlying causes: [19]
- Ischaemic Heart Disease 40%
- Dilated Cardiomyopathy 32%
- Valvular Heart Disease 12%
- Hypertension 11%
- Other 5%
Rarer causes of heart failure include:
- Viral Myocarditis (an infection of the heart muscle)
- Infiltrations of the muscle such as amyloidosis
- HIV cardiomyopathy (caused by Human Immunodeficiency Virus)
- Connective Tissue Diseases such as Systemic lupus erythematosus
- Drugs of abuse such as alcohol
- Pharmaceutical drugs such as chemotherapeutic agents.
- Arrhythmias
Obstructive Sleep Apnea a condition of sleep disordered breathing overlaps with obesity, hypertension and diabetes and is regarded as an independent cause of heart failure.
Acute decompensated heart failure
- See main article: Acute decompensated heart failure
Chronic stable heart failure may easily decompensate. This most commonly results from an intercurrent illness (such as pneumonia), myocardial infarction (a heart attack), arrhythmias, uncontrolled hypertension, or a patient's failure to maintain a fluid restriction, diet or medication.[20] Other well recognised precipitating factors include anaemia and hyperthyroidism which place additional strain on the heart muscle. Excessive fluid or salt intake, and medication that causes fluid retention such as NSAIDs and thiazolidinediones, may also precipitate decompensation.[21]
Pathophysiology
Heart failure is caused by any condition which reduces the efficiency of the myocardium, or heart muscle, through damage or overloading. As such, it can be caused by as diverse an array of conditions as myocardial infarction (in which the heart muscle is starved of oxygen and dies), hypertension (which increases the force of contraction needed to pump blood) and amyloidosis (in which protein is deposited in the heart muscle, causing it to stiffen). Over time these increases in workload will produce changes to the heart itself:
- Reduced contractility, or force of contraction, due to overloading of the ventricle. In health, increased filling of the ventricle results in increased contractility (by the Frank-Starling law of the heart) and thus a rise in cardiac output. In heart failure this mechanism fails, as the ventricle is loaded with blood to the point where heart muscle contraction becomes less efficient. This is due to reduced ability to cross-link actin and myosin filaments in over-stretched heart muscle.[22]
- A reduced stroke volume, as a result of a failure of systole, diastole or both. Increased end systolic volume is usually caused by reduced contractility. Decreased end diastolic volume results from impaired ventricular filling – as occurs when the compliance of the ventricle falls (i.e. when the walls stiffen).
- Reduced spare capacity. As the heart works harder to meet normal metabolic demands, the amount cardiac output can increase in times of increased oxygen demand (e.g. exercise) is reduced. This contributes to the exercise intolerance commonly seen in heart failure.
- Increased heart rate, stimulated by increased sympathetic activity in order to maintain cardiac output. Initially, this helps compensate for heart failure by maintaining blood pressure and perfusion, but places further strain on the myocardium, increasing coronary perfusion requirements, which can lead to worsening of ischemic heart disease. Sympathetic activity may also cause potentially fatal arrhythmias.
- Hypertrophy (an increase in physical size) of the myocardium, caused by the terminally differentiated heart muscle fibres increasing in size in an attempt to improve contractility. This may contribute to the increased stiffness and decreased ability to relax during diastole.
- Enlargement of the ventricles, contributing to the enlargement and spherical shape of the failing heart. The increase in ventricular volume also causes a reduction in stroke volume due to mechanical and contractile inefficiency.[23]
The general effect is one of reduced cardiac output and increased strain on the heart. This increases the risk of cardiac arrest (specifically due to ventricular dysrhythmias), and reduces blood supply to the rest of the body. In chronic disease the reduced cardiac output causes a number of changes in the rest of the body, some of which are physiological compensations, some of which are part of the disease process:
- Arterial blood pressure falls. This destimulates baroreceptors in the carotid body and aortic arch which link to the nucleus tractus solitarius. This center in the brain increases sympathetic activity, releasing catecholamines into the blood stream. Binding to alpha-1 receptors results in systemic arterial vasoconstriction. This helps restore blood pressure but also increases the total peripheral resistance, increasing the workload of the heart. Binding to beta-1 receptors in the myocardium increases the heart rate and make contractions more forceful, in an attempt to increase cardiac output. This also, however, increases the amount of work the heart has to perform.
- Increased sympathetic stimulation also causes the hypothalamus to secrete vasopressin (also known as antidiuretic hormone or ADH), which causes fluid retention at the kidneys. This increases the blood volume and blood pressure.
- Reduced perfusion (blood flow) to the kidneys stimulates the release of renin – an enzyme which catalyses the production of the potent vasopressor angiotensin. Angiotensin and its metabolites cause further vasocontriction, and stimulate increased secretion of the steroid aldosterone from the adrenal glands. This promotes salt and fluid retention at the kidneys, also increasing the blood volume.
- The chronically high levels of circulating neuroendocrine hormones such as catecholamines, renin, angiotensin, and aldosterone affects the myocardium directly, causing structural remodelling of the heart over the long term. Many of these remodelling effects seem to be mediated by transforming growth factor beta (TGF-beta), which is a common downstream target of the signal transduction cascade initiated by catecholamines[24] and angiotensin II[25], and also by epidermal growth factor (EGF), which is a target of the signaling pathway activated by aldosterone[26]
- Reduced perfusion of skeletal muscle causes atrophy of the muscle fibres. This can result in weakness, increased fatigueability and decreased peak strength - all contributing to exercise intolerance.[27]
The increased peripheral resistance and greater blood volume place further strain on the heart and accelerates the process of damage to the myocardium. Vasoconstriction and fluid retention produce an increased hydrostatic pressure in the capillaries. This shifts of the balance of forces in favour of interstitial fluid formation as the increased pressure forces additional fluid out of the blood, into the tissue. This results in edema (fluid build-up) in the tissues. In right-sided heart failure this commonly starts in the ankles where venous pressure is high due to the effects of gravity (although if the patient is bed-ridden, fluid accumulation may begin in the sacral region.) It may also occur in the abdominal cavity, where the fluid build-up is called ascites. In left-sided heart failure edema can occur in the lungs - this is called cardiogenic pulmonary oedema. This reduces spare capacity for ventilation, causes stiffening of the lungs and reduces the efficiency of gas exchange by increasing the distance between the air and the blood. The consequences of this are shortness of breath, orthopnoea and paroxysmal nocturnal dyspnea.
The symptoms of heart failure are largely determined by which side of the heart fails. The left side pumps blood into the systemic circulation, whilst the right side pumps blood into the pulmonary circulation. Whilst left-sided heart failure will reduce cardiac output to the systemic circultion, the initial symptoms often manifest due to effects on the pulmonary circulation. In systolic dysfunction, the ejection fraction is decreased, leaving an abnormally elevated volume of blood in the left ventricle. In diastolic dysfunction, end-diastolic ventricular pressure will be high. This increase in volume or pressure backs up to the left atrium and then to the pulmonary veins. Increased volume or pressure in the pulmonary veins impairs the normal drainage of the alveoli and favors the flow of fluid from the capillaries to the lung parenchyma, causing pulmonary edema. This impairs gas exchange. Thus, left-sided heart failure often presents with respiratory symptoms: shortness of breath, orthopnea and paroxysmal nocturnal dyspnea.
In severe cardiomyopathy, the effects of decreased cardiac output and poor perfusion become more apparent, and patients will manifest with cold and clammy extremities, cyanosis, claudication, generalized weakness, dizziness, and syncope
The resultant hypoxia caused by pulmonary edema causes vasoconstriction in the pulmonary circulation, which results in pulmonary hypertension. Since the right ventricle generates far lower pressures than the left ventricle (approximately 20 mmHg versus around 120 mmHg, respectively, in the healthy individual) but nonetheless generates cardiac output exactly equal to the left ventricle, this means that a small increase in pulmonary vascular resistance causes a large increase in amount of work the right ventricle must perform. However, the main mechanism by which left-sided heart failure causes right-sided heart failure is actually not well understood. Some theories invoke mechanisms that are mediated by neurohormonal activation. Mechanical effects may also contribute. As the left ventricle distends, the intraventricular septum bows into the right ventricle, decreasing the capacity of the right ventricle.
Systolic dysfunction
Heart failure caused by systolic dysfunction is more readily recognized. It can be simplistically described as failure of the pump function of the heart. It is characterized by a decreased ejection fraction (less than 45%). The strength of ventricular contraction is attenuated and inadequate for creating an adequate stroke volume, resulting in inadequate cardiac output. In general, this is caused by dysfunction or destruction of cardiac myocytes or their molecular components. In congenital diseases such as Duchenne muscular dystrophy, the molecular structure of individual myocytes is affected. Myocytes and their components can be damaged by inflammation (such as in myocarditis) or by infiltration (such as in amyloidosis). Toxins and pharmacological agents (such as ethanol, cocaine, and amphetamines) cause intracellular damage and oxidative stress. The most common mechanism of damage is ischemia causing infarction and scar formation. After myocardial infarction, dead myocytes are replaced by scar tissue, deleteriously affecting the function of the myocardium. On echocardiogram, this is manifest by abnormal or absent wall motion.
Because the ventricle is inadequately emptied, ventricular end-diastolic pressure and volumes increase. This is transmitted to the atrium. On the left side of the heart, the increased pressure is transmitted to the pulmonary vasculature, and the resultant hydrostatic pressure favors extravassation of fluid into the lung parenchyma, causing pulmonary edema. On the right side of the heart, the increased pressure is transmitted to the systemic venous circulation and systemic capillary beds, favoring extravassation of fluid into the tissues of target organs and extremities, resulting in dependent peripheral edema.
Diastolic dysfunction
Heart failure caused by diastolic dysfunction is generally described as the failure of the ventricle to adequately relax and typically denotes a stiffer ventricular wall. This causes inadequate filling of the ventricle, and therefore results in an inadequate stroke volume. The failure of ventricular relaxation also results in elevated end-diastolic pressures, and the end result is identical to the case of systolic dysfunction (pulmonary edema in left heart failure, peripheral edema in right heart failure.)
Diastolic dysfunction can be caused by processes similar to those that cause systolic dysfunction, particularly causes that affect cardiac remodeling.
Diastolic dysfunction may not manifest itself except in physiologic extremes if systolic function is preserved. The patient may be completely asymptomatic at rest. However, they are exquisitely sensitive to increases in heart rate, and sudden bouts of tachycardia (which can be caused simply by physiological responses to exertion, fever, or dehydration, or by pathological tachyarrhythmias such as atrial fibrillation with rapid ventricular response) may result in flash pulmonary edema. Adequate rate control (usually with a pharmacological agent that slows down AV conduction such as a calcium channel blocker or a beta-blocker) is therefore key to preventing decompensation.
Left ventricular diastolic function can be determined through echocardiography by measurement of various parameters such as the E/A ratio (early-to-atrial left ventricular filling ratio), the E (early left ventricular filling) deceleration time, and the isovolumic relaxation time.
Diagnosis

Imaging
Echocardiography is commonly used to support a clinical diagnosis of heart failure. This modality uses ultrasound to determine the stroke volume (SV, the amount of blood in the heart that exits the ventricles with each beat), the end-diastolic volume (EDV, the total amount of blood at the end of diastole), and the SV in proportion to the EDV, a value known as the ejection fraction. In pediatrics, the shortening fraction is the preferred measure of systolic function. Normally, the EF should be between 50% and 70%; in systolic heart failure, it drops below 40%. Echocardiography can also identify valvular heart disease and assess the state of the pericardium (the connective tissue sac surrounding the heart). Echocardiography may also aid in deciding what treatments will help the patient, such as medication, insertion of an implantable cardioverter-defibrillator or cardiac resynchronization therapy. Echocardiography can also help determine if acute myocardial ischemia is the precipitating cause, and may manifest as regional wall motion abnormalities on echo.
Chest X-rays are frequently used to aid in the diagnosis of CHF. In the compensated patient, this may show cardiomegaly (visible enlargement of the heart), quantified as the cardiothoracic ratio (proportion of the heart size to the chest). In left ventricular failure, there may be evidence of vascular redistribution ("upper lobe blood diversion" or "cephalization"), Kerley lines, cuffing of the areas around the bronchi, and interstitial edema.
Electrophysiology
An electrocardiogram (ECG/EKG) is used to identify arrhythmias, ischemic heart disease, right and left ventricular hypertrophy, and presence of conduction delay or abnormalities (e.g. left bundle branch block). An ECG may also diagnose acute myocardial ischemia or infarction (if ST depression or elevation are present).
Blood tests
Blood tests routinely performed include electrolytes (sodium, potassium), measures of renal function, liver function tests, thyroid function tests, a complete blood count, and often C-reactive protein if infection is suspected. An elevated B-type natriuretic peptide (BNP) is a specific test indicative of heart failure. Additionally, BNP can be used to differentiate between causes of dyspnea due to heart failure from other causes of dyspnea. If myocardial infarction is suspected, various cardiac markers may be used.
According to a meta-analysis comparing BNP and N-terminal pro-BNP (NTproBNP) in the diagnosis of heart failure, BNP is a better indicator for heart failure and left ventricular systolic dysfunction. In groups of symptomatic patients, a diagnostic odds ratio of 27 for BNP compares with a sensitivity of 85% and specificity of 84% in detecting heart failure. [28]
Angiography
Heart failure may be the result of coronary artery disease, and its prognosis depends in part on the ability of the coronary arteries to supply blood to the myocardium (heart muscle). As a result, coronary catheterization may be used to identify possibilities for revascularisation through percutaneous coronary intervention or bypass surgery.
Monitoring
Various measures are often used to assess the progress of patients being treated for heart failure. These include fluid balance (calculation of fluid intake and excretion), monitoring body weight (which in the shorter term reflects fluid shifts).
Treatment
Treatment focuses on improving the symptoms and preventing the progression of the disease. Reversible causes of the heart failure also need to be addressed: (e.g. infection, alcohol ingestion, anemia, thyrotoxicosis, arrhythmia, hypertension). Treatments include lifestyle and pharmacological modalities.
Modalities
Diet and lifestyle measures
Patients with CHF are educated to undertake various non-pharmacological measures to improve symptoms and prognosis. Such measures include:[29]
- Moderate physical activity, when symptoms are mild or moderate; or bed rest when symptoms are severe.
- If sleep apnea is identified, treat with CPAP, BiPAP, dental appliances or surgery. Sleep apnea is an under recognized risk factor for heart failure
- Weight reduction – through physical activity and dietary modification, as obesity is a risk factor for heart failure and left ventricular hypertrophy.
- Monitor weight - this is a parameter that can easily be measured at home. Rapid weight increase is generally due to fluid retention. Weight gain of more than 2 pounds is associated with admission to the hospital for heart failure[30]
- Sodium restriction – excessive sodium intake may precipitate or exacerbate heart failure, thus a "no added salt" diet (60–100 mmol total daily intake) is recommended for patients with CHF. More severe restrictions may be required in severe CHF.
- Fluid restriction – patients with CHF have a diminished ability to excrete free water load. Hyponatremia frequently develops in decompensated heart failure due to the effects of excess circulating neuroendocrine hormones. While the activation of the renin-angiotensin-aldosterone axis due to decreased renal perfusion promotes both sodium and water retention, the activation of atrial natriuretic peptide due to atrial stretch favors sodium excretion, and the activation of antidiuretic hormone due to peripheral baroreceptors that sense hypotension as well as due to the activation of the sympathetic nervous system favors water retention alone, leading to disproportionately more water retention than sodium retention. The severity of the hyponatremia during an episode of decompensated heart failure can be predictive of mortality. Generally water intake should be limited to 1.5 L daily or less in patients with hyponatremia, though fluid restriction may be beneficial regardless in symptomatic reduction.
Pharmacological management
There is a significant evidence–practice gap in the treatment of CHF; particularly the underuse of ACE inhibitors and β-blockers and aldosterone antagonists which have been shown to provide mortality benefit.[31] Treatment of CHF aims to relieve symptoms, to maintain a euvolemic state (normal fluid level in the circulatory system), and to improve prognosis by delaying progression of heart failure and reducing cardiovascular risk. Drugs used include: diuretic agents, vasodilator agents, positive inotropes, ACE inhibitors, beta blockers, and aldosterone antagonists (e.g. spironolactone). Some drugs which increase heart function, such as the positive inotrope Milrinone, lead to increased mortality, and are contraindicated.[32][33]
Angiotensin-modulating agents
ACE inhibitor (ACE) therapy is recommended for all patients with systolic heart failure, irrespective of symptomatic severity or blood pressure.[34][13][35] ACE inhibitors improve symptoms, decrease mortality and reduce ventricular hypertrophy. Angiotensin II receptor antagonist therapy (also referred to as AT1-antagonists or angiotensin receptor blockers), particularly using candesartan, is an acceptable alternative if the patient is unable to tolerate ACEI therapy.[36][37] ACEIs and ARBs decrease afterload by antagonizing the vasopressor effect of angiotensin, thereby decreasing the amount of work the heart must perform. It is also believed that angiotensin directly affects cardiac remodeling, and blocking its activity can thereby slow the deterioration of cardiac function.
Diuretics
Diuretic therapy is indicated for relief of congestive symptoms. Several classes are used, with combinations reserved for severe heart failure:[29]
- Loop diuretics (e.g. furosemide, bumetanide) – most commonly used class in CHF, usually for moderate CHF.
- Thiazide diuretics (e.g. hydrochlorothiazide, chlorthalidone, chlorthiazide) – may be useful for mild CHF, but typically used in severe CHF in combination with loop diuretics, resulting in a synergistic effect.
- Potassium-sparing diuretics (e.g. amiloride) – used first-line use to correct hypokalaemia.
- Spironolactone is used as add-on therapy to ACEI plus loop diuretic in severe CHF.
- Eplerenone is specifically indicated for post-MI reduction of cardiovascular risk.
If a heart failure patient exhibits a resistance to or poor response to diuretic therapy, ultrafiltration or aquapheresis may be needed to achieve adequate control of fluid retention and congestion. The use of such mechanical methods of fluid removal can produce meaningful clinical benefits in patients with diuretic-resistant heart failure and may restore responsiveness to conventional doses of diuretics.9
Beta blockers
Until recently (within the last 20 years), β-blockers were contraindicated in CHF, owing to their negative inotropic effect and ability to produce bradycardia – effects which worsen heart failure. However, current guidelines recommend β-blocker therapy for patients with systolic heart failure due to left ventricular systolic dysfunction after stabilization with diuretic and ACEI therapy, irrespective of symptomatic severity or blood pressure.[35] As with ACEI therapy, the addition of a β-blocker can decrease mortality and improve left ventricular function. Several β-blockers are specifically indicated for CHF including: bisoprolol, carvedilol,nebivolol and extended-release metoprolol. The antagonism of β1 inotropic and chronotropic effects decreases the amount of work the heart must perform. It is also thought that catecholamines and other sympathomimetics have an effect on cardiac remodeling, and blocking their activity can slow the deterioration of cardiac function.
Positive inotropes
Digoxin (a mildly positive inotrope and negative chronotrope), once used as first-line therapy, is now reserved for control of ventricular rhythm in patients with atrial fibrillation; or where adequate control is not achieved with an ACEI, a beta blocker and a loop diuretic.[35] There is no evidence that digoxin reduces mortality in CHF, although some studies suggest a decreased rate in hospital admissions.[38] It is contraindicated in cardiac tamponade and restrictive cardiomyopathy.
The inotropic agent dobutamine is advised only in the short-term use of acutely decompensated heart failure, and has no other uses.[35]
Phosphodiesterase inhibitors such as milrinone are sometimes utilized in severe cardiomyopathy. The mechanism of action is through the antagonism of adenosine receptors, resulting in inotropic effects and modest diuretic effects.
Alternative vasodilators
The combination of isosorbide dinitrate/hydralazine is the only vasodilator regimen, other than ACE inhibitors or angiotensin II receptor antagonists, with proven survival benefits. This combination appears to be particularly beneficial in CHF patients with an African American background, who respond less effectively to ACEI therapy.[39][40]
Aldosterone receptor antagonists
The RALES trial[41] showed that the addition of spironolactone can improve mortality, particularly in severe cardiomyopathy (ejection fraction less than 25%.) The related drug eplerenone was shown in the EPHESUS trial[42] to have a similar effect, and it is specifically labelled for use in decompensated heart failure complicating acute myocardial infarction. While the antagonism of aldosterone will decrease the effects of sodium and water retention, it is thought that the main mechanism of action is by antagonizing the deleterious effects of aldosterone on cardiac remodeling.
Recombinant neuroendocrine hormones
Nesiritide, a recombinant form of B-natriuretic peptide, is indicated for use in patients with acute decompensated heart failure who have dyspnea at rest. Nesiritide promotes diuresis and natriuresis, thereby ameliorating volume overload. It is thought that, while BNP is elevated in heart failure, the peptide that is produced is actually dysfunctional or non-functional and thereby ineffective.
Vasopressin receptor antagonists
Tolvaptan and conivaptan antagonize the effects of antidiuretic hormone (vasopressin), thereby promoting the specific excretion of free water, directly ameliorating the volume overloaded state, and counteracting the hyponatremia that occurs due to the release of neuroendocrine hormones in an attempt to counteract the effects of heart failure. The EVEREST trial, which utilized tolvaptan, showed that when used in combination with conventional therapy, many symptoms of acute decompensated heart failure were significantly improved compared to conventional therapy alone[43] although they found no difference in mortality and morbidity when compared to conventional therapy.[44].
Devices
Patients with NYHA class III or IV, left ventricular ejection fraction (LVEF) of 35% or less and a QRS interval of 120 ms or more may benefit from cardiac resynchronization therapy (CRT; pacing both the left and right ventricles), through implantation of a bi-ventricular pacemaker, or surgical remodeling of the heart. These treatment modalities may make the patient symptomatically better, improving quality of life and in some trials have been proven to reduce mortality.
The COMPANION trial demonstrated that CRT improved survival in individuals with NYHA class III or IV heart failure with a widened QRS complex on an electrocardiogram.[45] The CARE-HF trial showed that patients receiving CRT and optimal medical therapy benefited from a 36% reduction in all cause mortality, and a reduction in cardiovascular-related hospitalization.[46]
Patients with NYHA class II, III or IV, and LVEF of 35% (without a QRS requirement) may also benefit from an implantable cardioverter-defibrillator (ICD), a device that is proven to reduce all cause mortality by 23% compared to placebo in patients who were already optimally managed on drug therapy.[47][48] Patients with severe cardiomyopathy are at high risk for sudden cardiac death due to ventricular dysrhythmias. Although ICDs deliver electrical shocks to resynchronize heart rhythm which are potentially destressing to the patient, they have not been shown to affect quality of life.[49] The number of (appropriate and inappropriate) shocks seems to be associated to a worse outcome.[50] Although they are expensive, ICDs are potentially cost-effective in this setting.[51]
Another current treatment involves the use of left ventricular assist devices (LVADs). LVADs are battery-operated mechanical pump-type devices that are surgically implanted on the upper part of the abdomen. They take blood from the left ventricle and pump it through the aorta. LVADs are becoming more common and are often used by patients who have to wait for heart transplants.
Surgery
The final option, if other measures have failed, is heart transplantation or (temporary or prolonged) implantation of an artificial heart. These remain the recommended surgical treatment options. However, the limited number of hearts available for transplantation in a growing group of candidates, has led to the development of alternative surgical approaches to heart failure. These commonly involve surgical left ventricular remodeling. The aim of the procedures is to reduce the ventricle diameter (targeting Laplace's law and the disease mechanism of heart failure), improve its shape and/or remove non-viable tissue.[52] These procedures can be performed together with coronary artery bypass surgery or mitral valve repair.
If heart failure ensues after a myocardial infarction due to scarring and aneurysm formation, reconstructive surgery may be an option. These aneurysms bulge with every contraction, making it inefficient. Cooley and coworkers reported the first surgical treatment of a left ventricular aneurysm in 1958.[53] The used a linear closure after their excision. In the 1980s, Vincent Dor developed a method using an circular patch stitched to the inside of the ventricle (the endoventricular circular patch plasty or Dor procedure) to close the defect after excision.[54] His approach has been modified by others. Today, this is the preferred method for surgical treatment of incorrectly contracting (dyskinetic) left ventricle tissue, although a linear closure technique combined with septoplasty might be equally effective.[55][56] The multicenter RESTORE trial of 1198 participants demonstrated an increase in ejection fraction from about 30% to 40% with a concomitant shift in NYHA classes, with an early mortality of 5% and a 5-year survival of 70%.[57] As of yet, it remains unknown if surgery is superior to optimal medical therapy. The STICH trial (Surgical Treatment for IschemiC Heart Failure) will examine the role of medical treatment, coronary artery bypass surgery and left ventricle remodeling surgery in heart failure patients. Results are expected to be published in 2009 and 2011.[58]
The Batista procedure was invented by Brazilian doctor Randas Batista in 1994 for use in patients with non-ischemic dilated cardiomyopathy. It involves removal of a portion of viable tissue from the left ventricle to reduce its size (partial left ventriculectomy), with or without repair or replacement of the mitral valve.[59]. Although several studies showed benefits from this surgery, studies at the Cleveland Clinic concluded that this procedure was associated with a high early and late failure rate. At 3 years only 26 percent were event-free and survival rate was only 60 percent.[60] Most hospitals have abandoned this operation and it is no longer included in heart failure guidelines.[52]
Newer procedures under examination are based on the observation that the spherical configuration of the dilated heart reduces ejection fraction compared to the elliptical form. Mesh-like constraint devices such as the Acorn CorCap aim to improve contraction efficacy and prevent further remodeling. Clinical trials are underway.[61] Another technique which aims to divide the spherical ventricle into two elliptical halves is used with the Myosplint device.[62]
Approach
Acute decompensation
- See main article: Acute decompensated heart failure
In acute decompensated heart failure (ADHF), the immediate goal is to re-establish adequate perfusion and oxygen delivery to end organs. This entails ensuring that airway, breathing, and circulation are adequate.
Chronic management
The goal is to prevent the development of acute decompensated heart failure, to counteract the deleterious effects of cardiac remodeling, and to minimize the symptoms that the patient suffers. In addition to pharmacologic agents (oral loop diuretics, beta-blockers, ACE inhibitors or angiotensin receptor blockers, vasodilators, and in severe cardiomyopathy aldosterone receptor antagonists), behavioral modification should be pursued, specifically with regards to dietary guidelines regarding salt and fluid intake. Exercise should be encouraged as tolerated, as sufficient conditioning can significantly improve quality-of-life.
In patients with severe cardiomyopathy, implantation of an automatic implantable cardioverter defibrillator(AICD) should be considered. A select population will also probably benefit from ventricular resynchronization.
In select cases, cardiac transplantation can be considered. While this may resolve the problems associated with heart failure, the patient generally must remain on an immunosuppressive regimen to prevent rejection, which has its own significant downsides.
Palliative care and hospice
Without transplantation, heart failure caused by ischemic heart disease is not reversible, and cardiac function typically deteriorates with time. (In particular, diastolic function worsens as a function of age even in individuals without ischemic heart disease.) The growing number of patients with Stage D heart failure (intractable symptoms of fatigue, shortness of breath or chest pain at rest despite optimal medical therapy) should be considered for palliative care or hospice, according to American College of Cardiology/American Heart Association guidelines.
Prognosis
Prognosis in heart failure can be assessed in multiple ways including clinical prediction rules and cardiopulmonary exercise testing. Clinical prediction rules use a composite of clinical factors such as lab tests and blood pressure to estimate prognosis. Among several clinical prediction rules for prognosing acute heart failure, the 'EFFECT rule' slightly outperformed other rules in stratifying patients and identifying those at low risk of death during hospitalization or within 30 days.[63] Easy methods for identifying low risk patients are:
- ADHERE Tree rule indicates that patients with blood urea nitrogen < 43 mg/dl and systolic blood pressure at least 115 mm Hg have less than 10% chance of inpatient death or complications.
- BWH rule indicates that patients with systolic blood pressure over 90 mm Hg, respiratory rate of 30 or less breaths per minute, serum sodium over 135 mmol/L, no new ST-T wave changes have less than 10% chance of inpatient death or complications.
A very important method for assessing prognosis in advanced heart failure patients is cardiopulmonary exercise testing (CPX testing). CPX testing is usually required prior to heart transplantation as an indicator of prognosis. Cardiopulmonary exercise testing involves measurement of exhaled oxygen and carbon dioxide during exercise. The peak oxygen consumption (VO2 max) is used as an indicator of prognosis. As a general rule, a VO2 max less than 12-14 cc/kg/min indicates a poorer survival and suggests that the patient may be a candidate for a heart transplant. Patients with a VO2 max<10 cc/kg/min have clearly poorer prognosis. The most recent International Society for Heart and Lung Transplantation (ISHLT) guidelines (http://www.jhltonline.org/article/PIIS1053249806004608/fulltext#sec1) also suggest two other parameters that can be used for evaluation of prognosis in advanced heart failure, the heart failure survival score and the use of a criteria of VE/VCO2 slope>35 from the CPX test. The heart failure survival score is a score calculated using a combination of clinical predictors and the VO2 max from the cardiopulmonary exercise test.
Epidemiology
Heart failure is the leading cause of hospitalization in people older than 65.[64] In developed countries, the mean age of patients with heart failure is 75 years old.[4] In developing countries, two to three percent of the population suffers from heart failure, but in those 70 to 80 years old, it occurs in 20—30 percent.
References
- ↑ heart failure at Dorland's Medical Dictionary
- ↑ 2.0 2.1 2.2 McMurray JJ, Pfeffer MA (2005). "Heart failure". Lancet 365 (9474): 1877–89. doi:. PMID 15924986.
- ↑ Dickstein K, Cohen-Solal A, Filippatos G, et al (October 2008). "ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM)". Eur. Heart J. 29 (19): 2388–442. doi:. PMID 18799522. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=18799522.
- ↑ 4.0 4.1 Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, McMurray JJ (June 2002). "The current cost of heart failure to the National Health Service in the UK". Eur. J. Heart Fail. 4 (3): 361–71. PMID 12034163. http://linkinghub.elsevier.com/retrieve/pii/S1388984201001982.
- ↑ Rosamond W, Flegal K, Furie K, et al (January 2008). "Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee". Circulation 117 (4): e25–146. doi:. PMID 18086926. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=18086926.
- ↑ Juenger J, Schellberg D, Kraemer S, et al (March 2002). "Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables". Heart 87 (3): 235–41. PMID 11847161. PMC: 1767036. http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=11847161.
- ↑ Hobbs FD, Kenkre JE, Roalfe AK, Davis RC, Hare R, Davies MK (December 2002). "Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population". Eur. Heart J. 23 (23): 1867–76. PMID 12445536. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12445536.
- ↑ Neubauer S (2007). "The failing heart — an engine out of fuel". N Engl J Med 356 (11): 1140–51. doi:. PMID 17360992.
- ↑ congestive heart failure at Dorland's Medical Dictionary
- ↑ high-output heart failure at Dorland's Medical Dictionary
- ↑ Criteria Committee, New York Heart Association. Diseases of the heart and blood vessels. Nomenclature and criteria for diagnosis, 6th ed. Boston: Little, Brown and co, 1964;114.
- ↑ Raphael C, Briscoe C, Davies J, et al (2007). "Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure". Heart 93 (4): 476–82. doi:. PMID 17005715.
- ↑ 13.0 13.1 Hunt SA, Abraham WT, Chin MH, et al (2005). "ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult" (PDF). Circulation 112 (12): e154–235. doi:. PMID 16160202. http://circ.ahajournals.org/cgi/reprint/112/12/e154.pdf.
- ↑ McKee PA, Castelli WP, McNamara PM, Kannel WB (1971). "The natural history of congestive heart failure: the Framingham study". N. Engl. J. Med. 285 (26): 1441–6. PMID 5122894.
- ↑ Carlson KJ, Lee DC, Goroll AH, Leahy M, Johnson RA (1985). "An analysis of physicians' reasons for prescribing long-term digitalis therapy in outpatients". Journal of chronic diseases 38 (9): 733–9. doi:. PMID 4030999.
- ↑ Harlan WR, oberman A, Grimm R, Rosati RA (1977). "Chronic congestive heart failure in coronary artery disease: clinical criteria". Ann. Intern. Med. 86 (2): 133–8. PMID 835934.
- ↑ Killip T, Kimball JT (1967). "Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients". Am. J. Cardiol. 20 (4): 457–64. doi:. PMID 6059183.
- ↑ He J; Ogden LG; Bazzano LA; Vupputuri S, et al (2001). "Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study.". Arch. Intern. Med. 161 (7): 996–1002. doi:. PMID 11295963.
- ↑ Baldasseroni S; Opasich C; Gorini M; Lucci D, et al (2002). "Left bundle-branch block is associated with increased 1-year sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report from the Italian network on congestive heart failure.". American Heart Journal 143 (3): 398–405. doi:. PMID 11868043.
- ↑ Fonarow GC, Abraham WT, Albert NM, et al (April 2008). "Factors Identified as Precipitating Hospital Admissions for Heart Failure and Clinical Outcomes: Findings From OPTIMIZE-HF". Arch. Intern. Med. 168 (8): 847–854. doi:. PMID 18443260.
- ↑ Nieminen MS, Böhm M, Cowie MR, et al (February 2005). "Executive summary of the guidelines on the diagnosis and treatment of acute heart failure: the Task Force on Acute Heart Failure of the European Society of Cardiology". Eur. Heart J. 26 (4): 384–416. doi:. PMID 15681577. http://eurheartj.oxfordjournals.org/cgi/content/full/26/4/384.
- ↑ Boron and Boulpaep 2005 Medical Physiology Updated Edition p533 ISBN 0721632564
- ↑ cardiac pathophysiology in heart failure at GPnotebook
- ↑ Shigeyama J, Yasumura Y, Sakamoto A, et al (December 2005). "Increased gene expression of collagen Types I and III is inhibited by beta-receptor blockade in patients with dilated cardiomyopathy". Eur. Heart J. 26 (24): 2698–705. doi:. PMID 16204268.
- ↑ Tsutsui H, Matsushima S, Kinugawa S, et al (May 2007). "Angiotensin II type 1 receptor blocker attenuates myocardial remodeling and preserves diastolic function in diabetic heart" (– Scholar search). Hypertens. Res. 30 (5): 439–49. doi:. PMID 17587756. http://joi.jlc.jst.go.jp/JST.JSTAGE/hypres/30.439?from=PubMed.
- ↑ Krug AW, Grossmann C, Schuster C, et al (October 2003). "Aldosterone stimulates epidermal growth factor receptor expression". J. Biol. Chem. 278 (44): 43060–6. doi:. PMID 12939263.
- ↑ systemic pathophysiology in heart failure at GPnotebook
- ↑ Ewald B, Ewald D, Thakkinstian A, Attia J (2008). "Meta-analysis of B type natriuretic peptide and N-terminal pro B natriuretic peptide in the diagnosis of clinical heart failure and population screening for left ventricular systolic dysfunction". Intern Med J 38 (2): 101–13. doi:. PMID 18290826. http://www.blackwell-synergy.com/doi/abs/10.1111/j.1445-5994.2007.01454.x.
- ↑ 29.0 29.1 Smith A, Aylward P, Campbell T, et al. Therapeutic Guidelines: Cardiovascular, 4th edition. North Melbourne: Therapeutic Guidelines; 2003. ISSN 1327-9513
- ↑ Chaudhry SI et al (2007). "Patterns of Weight Change Preceding Hospitalization for Heart Failure". Circulation 116: 1549. doi:. PMID 17846286.
- ↑ Jackson S, Bereznicki L, Peterson G. Under-use of ACE-inhibitor and β-blocker therapies in congestive cardiac failure. Australian Pharmacist 2005;24(12):936.
- ↑ Packer M (1989). "Effect of phosphodiesterase inhibitors on survival of patients with chronic congestive heart failure". Am. J. Cardiol. 63 (2): 41A–45A. doi:. PMID 2642629.
- ↑ Packer M, Carver JR, Rodeheffer RJ, et al (1991). "Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group". N. Engl. J. Med. 325 (21): 1468–75. PMID 1944425.
- ↑ Krum H, National Heart Foundation of Australia and Cardiac Society of Australia & New Zealand Chronic Heart Failure Clinical Practice Guidelines Writing Panel. (2001). "Guidelines for management of patients with chronic heart failure in Australia". Med J Aust 174 (9): 459–66. PMID 11386592.
- ↑ 35.0 35.1 35.2 35.3 National Institute for Clinical Excellence. Chronic heart failure: management of chronic heart failure in adults in primary and secondary care. Clinical Guideline 5. London: National Institute for Clinical Excellence; 2003 Jul. Available from: www.nice.org.uk/pdf/CG5NICEguideline.pdf
- ↑ Granger CB, McMurray JJ, Yusuf S, Held P, Michelson EL, Olofsson B, Ostergren J, Pfeffer MA, Swedberg K; CHARM Investigators and Committees. (2003). "Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial". Lancet 362 (9386): 772–6. doi:. PMID 13678870.
- ↑ Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, Yusuf S, Pocock S; CHARM Investigators and Committees. (2003). "Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme". Lancet 362 (9386): 759–66. doi:. PMID 13678868.
- ↑ Haji SA, Movahed A (2000). "Update on digoxin therapy in congestive heart failure". American family physician 62 (2): 409–16. PMID 10929703.
- ↑ Exner DV, Dries DL, Domanski MJ, Cohn JN (2001). "Lesser response to angiotensin-converting-enzyme inhibitor therapy in black as compared with white patients with left ventricular dysfunction". N Engl J Med. 344 (18): 1351–7. doi:. PMID 11333991.
- ↑ Taylor AL, Ziesche S, Yancy C, Carson P, D'Agostino R Jr, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN; African-American Heart Failure Trial Investigators. (2004). "Combination of isosorbide dinitrate and hydralazine in blacks with heart failure". N Engl J Med 351 (20): 2049–57. doi:. PMID 15533851.
- ↑ Pitt B, Zannad F, Remme W, Cody R, Castaigne A, Perez A, Palensky J, Wittes J (1999). "The Effect of Spironolactone on Morbidity and Mortality in Patients with Severe Heart Failure". N Engl J Med. 341 (10): 709–717. doi:. PMID 10471456.
- ↑ Pitt B, Williams G, Remme W, Martinez F, Lopez-Sendon J, Zannad F, Neaton J, Roniker B, Hurley S, Burns D, Bittman R, Kleiman J. (2001). "The EPHESUS trial: eplerenone in patients with heart failure due to systolic dysfunction complicating acute myocardial infarction. Eplerenone Post-AMI Heart Failure Efficacy and Survival Study". Cardiovasc Drugs Ther 15 (1): 79–87. doi:. PMID 11504167.
- ↑ Gheorghiade M, Konstam MA, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C; Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators. (2007). "Short-term clinical effects of tolvaptan, an oral vasopressin antagonist, in patients hospitalized for heart failure: the EVEREST Clinical Status Trials". JAMA 297 (12): 1332–1343. doi:. PMID 17384438.
- ↑ Konstam MA, Gheorghiade M, Burnett JC Jr, Grinfeld L, Maggioni AP, Swedberg K, Udelson JE, Zannad F, Cook T, Ouyang J, Zimmer C, Orlandi C; Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan (EVEREST) Investigators. (2007). "Effects of oral tolvaptan in patients hospitalized for worsening heart failure: the EVEREST Outcome Trial". JAMA 297 (12): 1319–1331. doi:. PMID 17384437.
- ↑ Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM; Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators. (2004). "Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure". N Engl J Med 350 (21): 2140–50. doi:. PMID 15152059.
- ↑ Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. (2005). "The effect of cardiac resynchronization on morbidity and mortality in heart failure". N Engl J Med 352 (15): 1539–49. doi:. PMID 15753115.
- ↑ Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. (2005). "Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure". N Engl J Med 352 (3): 225–237. doi:. PMID 15659722.
- ↑ Moss AJ, Zareba W, Hall WJ, et al (March 2002). "Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction". N. Engl. J. Med. 346 (12): 877–83. doi:. PMID 11907286. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=11907286&promo=ONFLNS19.
- ↑ Mark DB, Anstrom KJ, Sun JL, Clapp-Channing NE, Tsiatis AA, Davidson-Ray L, Lee KL, Bardy GH; Sudden Cardiac Death in Heart Failure Trial Investigators (September 2008). "Quality of life with defibrillator therapy or amiodarone in heart failure". N. Engl. J. Med. 359 (10): 999–1008. doi:. PMID 18768943. http://content.nejm.org/cgi/content/abstract/359/10/999.
- ↑ Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, Talajic M, Wilber DJ, Fishbein DP, Packer DL, Mark DB, Lee KL, Bardy GH; Sudden Cardiac Death in Heart Failure Trial Investigators (September 2008). "Prognostic Importance of Defibrillator Shocks in Patients with Heart Failure". N. Engl. J. Med. 359 (10): 1009–1017. doi:. PMID 18768944. http://content.nejm.org/cgi/content/abstract/359/10/1009.
- ↑ Sanders GD, Hlatky MA, Owens DK (October 2005). "Cost-effectiveness of implantable cardioverter-defibrillators". N. Engl. J. Med. 353 (14): 1471–80. doi:. PMID 16207849. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=16207849&promo=ONFLNS19.
- ↑ 52.0 52.1 Tønnessen T, Knudsen CW (August 2005). "Surgical left ventricular remodeling in heart failure". Eur. J. Heart Fail. 7 (5): 704–9. doi:. PMID 16087128.
- ↑ Cooley DA, Collins HA, Morris GC, Chapman DW (May 1958). "Ventricular aneurysm after myocardial infarction; surgical excision with use of temporary cardiopulmonary bypass". J Am Med Assoc 167 (5): 557–60. PMID 13538738.
- ↑ Dor V (September 2001). "The endoventricular circular patch plasty ("Dor procedure") in ischemic akinetic dilated ventricles". Heart Fail Rev 6 (3): 187–93. doi:. PMID 11391036. http://www.kluweronline.com/art.pdf?issn=1382-4147&volume=6&page=187.
- ↑ Lundblad R, Abdelnoor M, Svennevig JL (September 2004). "Surgery for left ventricular aneurysm: early and late survival after simple linear repair and endoventricular patch plasty". J. Thorac. Cardiovasc. Surg. 128 (3): 449–56. doi:. PMID 15354107. http://linkinghub.elsevier.com/retrieve/pii/S0022522304006427.
- ↑ Mickleborough LL, Carson S, Ivanov J (April 2001). "Repair of dyskinetic or akinetic left ventricular aneurysm: results obtained with a modified linear closure". J. Thorac. Cardiovasc. Surg. 121 (4): 675–82. doi:. PMID 11279407. http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(01)49811-4.
- ↑ Athanasuleas CL, Buckberg GD, Stanley AW, et al (October 2004). "Surgical ventricular restoration in the treatment of congestive heart failure due to post-infarction ventricular dilation". J. Am. Coll. Cardiol. 44 (7): 1439–45. doi:. PMID 15464325. http://linkinghub.elsevier.com/retrieve/pii/S0735-1097(04)01443-3.
- ↑ Velazquez EJ, Lee KL, O'Connor CM, et al (December 2007). "The rationale and design of the Surgical Treatment for Ischemic Heart Failure (STICH) trial". J. Thorac. Cardiovasc. Surg. 134 (6): 1540–7. doi:. PMID 18023680. http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(07)01391-8.
- ↑ "Pioneers of heart surgery". NOVA Online: Cut to the heart. Retrieved on 2007-11-07.
- ↑ Franco-Cereceda A, McCarthy PM, Blackstone EH, et al (May 2001). "Partial left ventriculectomy for dilated cardiomyopathy: is this an alternative to transplantation?". J. Thorac. Cardiovasc. Surg. 121 (5): 879–93. doi:. PMID 11326231. http://linkinghub.elsevier.com/retrieve/pii/S0022-5223(01)37736-X.
- ↑ Oz MC, Konertz WF, Kleber FX, et al (October 2003). "Global surgical experience with the Acorn cardiac support device". J. Thorac. Cardiovasc. Surg. 126 (4): 983–91. doi:10.1016/S0022 (inactive 2008-06-29). PMID 14566236. http://linkinghub.elsevier.com/retrieve/pii/S0022522303000497.
- ↑ Schenk S, Reichenspurner H, Boehm DH, et al (June 2002). "Myosplint implant and shape-change procedure: intra- and peri-operative safety and feasibility". J. Heart Lung Transplant. 21 (6): 680–6. doi:. PMID 12057702.
- ↑ Auble TE, Hsieh M, McCausland JB, Yealy DM (2007). "Comparison of four clinical prediction rules for estimating risk in heart failure". Annals of emergency medicine 50 (2): 127–35, 135.e1–2. doi:. PMID 17449141.
- ↑ Krumholz HM, Chen YT, Wang Y, Vaccarino V, Radford MJ, Horwitz RI (2000). "Predictors of readmission among elderly survivors of admission with heart failure". Am. Heart J. 139 (1 Pt 1): 72–7. doi:. PMID 10618565.
See also
- Cardiogenic shock
- Heart transplant
- Dor procedure
- ACE inhibitor
- Isosorbide dinitrate/hydralazine
- Killip class
- Ventricular remodeling
- Fluid overload
- Framingham criteria
External links
- American Heart Association's Heart Failure web site - information and resources for treating and living with heart failure.
- Heart Failure Matters – patient information website of the Heart Failure Association of the European Society of Cardiology
- Congestive Heart Failure information from Seattle Children's Hospital Heart Center
- www.heartfailure-europe.com – patient information website of SHAPE (Study Group on Heart failure Awareness and Perception in Europe)
|
||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||