Hay fever
| Hay Fever Classification and external resources |
|
 |
|
|---|---|
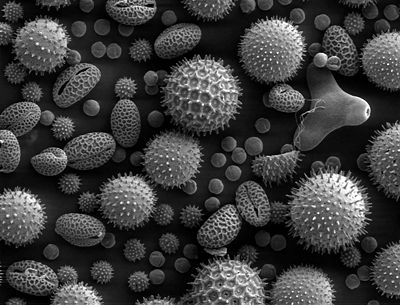
| Pollen grains from a variety of common plants can cause hay fever. | |
| ICD-10 | J30.1 |
| ICD-9 | 477 |
| OMIM | 607154 |
| DiseasesDB | 31140 |
| MedlinePlus | 000813 |
| eMedicine | ent/194 med/104 ped/2560 |
| MeSH | D006255 |
Allergic rhinitis, known as hay fever, is caused by pollens of specific seasonal plants, airborne chemicals and dust particles in people who are allergic to these substances. It is characterised by sneezing, runny nose and itching eyes. This seasonal allergic rhinitis is commonly known as 'hay fever', because it is most prevalent during haying season. It is particularly prevalent from late May to the end of June (in the Northern Hemisphere). However, it is possible to suffer from hay fever throughout the year.
Contents |
Causes
Hay fever involves an allergic reaction to pollen. A virtually identical reaction occurs with allergy to mold, animal dander, dust and similar inhaled allergens. Particulate matter in polluted air and chemicals such as chlorine and detergents, which can normally be tolerated, can greatly aggravate the condition.
The pollen which causes hay fever varies from person to person and from region to region; generally speaking, the tiny, hardly visible pollens of wind-pollinated plants are the predominant cause. Pollens of insect-pollinated plants are too large to remain airborne and pose no risk. Examples of plants commonly responsible for hay fever include:
- Trees: such as birch (Betula), alder (Alnus), cedar (Cedrus), hazel (Corylus), hornbeam (Carpinus), horse chestnut (Aesculus), willow (Salix), poplar (Populus), plane (Platanus), linden/lime (Tilia) and olive (Olea). In northern latitudes birch is considered to be the most important allergenic tree pollen, with an estimated 15–20% of hay fever sufferers sensitive to birch pollen grains. Olive pollen is most predominant in Mediterranean regions.
- Grasses (Family Poaceae): especially ryegrass (Lolium sp.) and timothy (Phleum pratense). An estimated 90% of hay fever sufferers are allergic to grass pollen.
- Weeds: ragweed (Ambrosia), plantain (Plantago), nettle/parietaria (Urticaceae), mugwort (Artemisia), Fat hen (Chenopodium) and sorrel/dock (Rumex)
In addition to individual sensitivity and geographic differences in local plant populations, the amount of pollen in the air can be a factor in whether hay fever symptoms develop. Hot, dry, windy days are more likely to have increased amounts of pollen in the air than cool, damp, rainy days when most pollen is washed to the ground.
The time of year at which hay fever symptoms manifest themselves varies greatly depending on the types of pollen to which an allergic reaction is produced. The pollen count, in general, is highest from mid-spring to early summer. As most pollens are produced at fixed periods in the year, a long-term hay fever sufferer may also be able to anticipate when the symptoms are most likely to begin and end, although this may be complicated by an allergy to dust particles.
When an allergen such as pollen or dust is inhaled by a person with a sensitized immune system, it triggers antibody production. These antibodies mostly bind to mast cells, which contain histamine. When the mast cells are stimulated by pollen and dust, histamine (and other chemicals) are released. This causes itching, swelling, and mucus production. Symptoms vary in severity from person to person. Very sensitive individuals can experience hives or other rashes.
Some disorders may be associated with allergies: Comorbidities include eczema, asthma, depression and migraine.[1]
Allergies are common. Heredity and environmental exposures may contribute to a predisposition to allergies. It is roughly estimated that one in three people have an active allergy at any given time and at least three in four people develop an allergic reaction at least once in their lives.
The two categories of allergic rhinitis include:
- seasonal - occurs particularly during pollen seasons. Seasonal allergic rhinitis does not usually develop until after 6 years of age.
- perennial - occurs throughout the year. This type of allergic rhinitis is commonly seen in younger children.[2]
Signs and tests
The history of the person's symptoms is important in diagnosing allergic rhinitis, including whether the symptoms vary according to time of day or the season, exposure to pets or other allergens, and diet changes.
Allergy testing may reveal the specific allergens the person is reacting to. Skin testing is the most common method of allergy testing. This may include intradermal, scratch, patch, or other tests. Less commonly, the suspected allergen is dissolved and dropped onto the lower eyelid as a means of testing for allergies. (This test should only be done by a physician, never the patient, since it can be harmful if done improperly.)
In some individuals who cannot undergo skin testing (as determined by the doctor), the RAST blood test may be helpful in determining specific allergen sensitivity.
Sufferers might also find that cross-reactivity occurs.[3] For example, someone allergic to birch pollen may also find that they have an allergic reaction to the skin of apples or potatoes.[4] A clear sign of this is the occurrence of an itchy throat after eating an apple or sneezing when peeling potatoes or apples. This occurs because of similarities in the proteins of the pollen and the food.[5] There are many cross-reacting substances.
Treatment and Prevention
The goal of treatment is to reduce allergy symptoms caused by the inflammation of affected tissues. The most effective way to decrease allergic symptoms is to completely avoid the allergen.[6] [7]
Prevention
Effectively preventing or reducing exposure to pollen requires consistent efforts.
Many people reduce their exposure by remaining indoors during hay fever season, particular in the morning and evening, when outdoor pollen levels are at their highest. Closing all the windows and doors prevents wind-borne pollen from entering the home or office. When traveling in a vehicle, closing all the windows reduces exposure. Air conditioners are reasonably effective filters, and special pollen filters can be fitted to both home and vehicle air conditioning systems.
Because pollen clings to clothing, skin, and hair, regular cleaning reduces exposure and therefore symptoms. People with hay fever experience fewer symptoms when they wash their hands, faces, and hair frequently. Not rubbing the eyes reduces the likelihood that pollen on the hands will get into the eyes. Many people bathe before sleeping, to minimize their exposure to the pollen that has stuck to their bodies during the day. Some people use nasal irrigation to rinse pollen out of their noses.
Frequently cleaning floors and washing bedding reduces pollen that is tracked in by family, pets and visitors. Drying clothes outside increases exposure to pollen, as wind-borne pollen will cling to the clothing.
Some specific activities increase pollen exposure and should be avoided. For example, walking in or near fields, large areas of grassland, or in rural areas risks significant pollen exposure. Mowing the grass, gardening, or doing other outdoor work risks pollen exposure. When these tasks are unavoidable, reducing the exposure to pollen may be helpful. Face masks designed to filter out pollen will reduce the amount of pollen that is inhaled, and wrap-around sunglasses will reduce the amount of pollen entering the eyes.
Medication
The most appropriate medication depends on the type and severity of symptoms. Specific illnesses that are caused by allergies (such as asthma and eczema) may require other treatments.
Options include the following:
Systemic therapy
Therapies that have an overall effect on a person's body and therefore thay may help for all of the symptoms include:
- Antihistamines
- these are taken orally and may relieve mild to moderate symptoms. The first-generation (non-selective or classical) antihistamines such as chlorphenamine and promethazine are perhaps the most effective, but their sedative side effects limits their usefulness compared to the newer second-generation and third-generation (selective, non-sedating) antihistamines such as loratadine and cetirizine. Most of these antihistamines are available as over-the-counter drugs.
- Glucocorticoids
- Corticosteroids administered to the whole body, such as Triamcinolone (Kenalog) by intramuscular injection, are also effective, but their use is limited by their short duration of effect, lasting a few weeks, and the side effects of prolonged steroid therapy.
- Leukotriene receptor antagonists
- these newer products, such as montelukast (Singulair) and zafirlukast (Accolate), have proven very effective in dealing with allergic rhinitis, without the common side-effects of the first-generation antihistamines, such as drowsiness. These medicines are also long-acting and are taken once-daily.
Topical therapy
Localised treatments may give more effective relief of eye or nasal symptoms.
Nasal treatments
- Steroid nasal sprays
- are effective and safe, and may be effective without oral antihistamines. These medications include, in order of potency: beclomethasone (Beconase), budesonide (Rhinocort), flunisolide (Syntaris), mometasone (Nasonex), fluticasone (Flonase, Flixonase), triamcinolone (Nasacort AQ). They take several days to act and so need be taken continually for several weeks as their therapeutic effect builds up with time.
- Cromoglicate
- is a drug that stabilizes mast cells to prevent their degranulation and subsequent release of histamine. It is available as a nasal spray (Nasalcrom) for treating hay fever, although it is generally less effective than nasal steroid sprays.
- Antihistamine
- Azelastine (Astelin) is the only antihistamine available as a nasal spray.
- Topical decongestants
- may also be helpful in reducing symptoms such as nasal congestion, but should not be used for long periods as stopping them after protracted use can lead to a rebound nasal congestion (Rhinitis medicamentosa).
- Saltwater sprays, rinses or steam
- this removes dust, secretions and allergenic molecules from the mucosa, as they are all instant water soluble. A suitable solution is 2-3 spoonful of salt dissolved in one litre of lukewarm water.[8]
Eye treatments
- Cromoglicate
- is also used as eye drops (Crolom in US and Opticrom in UK being best known brands). Nedocromil is a newer variant of cromoglycate and has essentially the same activity.
Allergy immunotherapy
Allergy immunotherapy is commonly used in patients suffering from allergic rhinitis, allergic asthma, or life threatening stinging insect allergy. This type of therapy has been found to potentially alter the course of all three of the above disorders. Allergen immunotherapy provides long-term relief of the symptoms associated with rhinitis and asthma.
"Allergy shots" (Hyposensibilization, immunotherapy) are occasionally recommended if the allergen cannot be avoided and if symptoms are hard to control. This includes regular injections of the allergen, given in increasing doses, which may help the body adjust to the antigen. These tend to be offered as a last resort as the therapy is more expensive at first, although patients may save money on medications and doctor visits in the long run. They may also increase the risk of triggering a secondary allergic reaction such as an asthma attack.
Allergy shot treatment is the closest thing to a ‘cure’ for allergic symptoms. This therapy requires a long-term commitment.
Herbal treatments
A large number of over-the-counter treatments are sold without FDA approval, including herbs like eyebright (Euphrasia officinalis), nettle (Urtica dioica), and bayberry (Myrica cerifera), which have not been shown to reduce the symptoms of nasal-pharynx congestion. In addition, feverfew (Tanacetum parthenium) and turmeric (Curcuma longa) has been shown to inhibit phospholipase A2, the enzyme which releases the inflammatory precursor arachidonic acid from the bi-layer membrane of mast cells (the main cells which respond to respiratory allergens and lead to inflammation) but this is only in test tubes and it is not established as anti-inflammatory in humans.
Homeopathy
It has been claimed that homeopathy provides relief free of side-effects. However, this is strongly disputed by the medical profession on the grounds that there is no valid evidence to support this claim.[9]
Acupuncture
Therapeutic efficacy of complementary-alternative treatments for rhinitis and asthma is not supported by currently available evidence.[10][11]
Nevertheless, there have been some attempts with controlled trials[12] to show that acupuncture is more effective than antihistamine drugs in treatment of hay fever. Complementary-alternative medicines such as acupuncture are extensively offered in the treatment of allergic rhinitis by non-physicians but evidence-based recommendations are lacking. The methodology of clinical trials with complementary-alternative medicine is frequently inadequate. Meta-analyses provides no clear evidence for the efficacy of acupuncture in rhinitis (or asthma). It is not possible to provide evidence-based recommendations for acupuncture or homeopathy in the treatment of allergic rhinitis.
Honey
Eating locally produced unfiltered honey is believed by many to be a treatment for hayfever, supposedly by introducing manageable amounts of pollen to the body. Clinical studies have not provided any evidence for this belief.[13]
Expectations
Most symptoms of allergic rhinitis can be readily treated.
In some cases (particularly in children), people may outgrow an allergy as the immune system becomes less sensitive to the allergen. However, as a general rule, once a substance causes allergies for an individual, it can continue to affect the person over the long term.
More severe cases of allergic rhinitis require immunotherapy (allergy shots) or removal of tissue in the nose (e.g., nasal polyps) or sinuses.
Complications
- drowsiness and other side effects of antihistamines
- side-effects of other medications (see the specific medication)
- asthma
- sinusitis
- nasal polyps
- disruption of lifestyle (can be extensive)
A case-control study found "symptomatic allergic rhinitis and rhinitis medication use are associated with a significantly increased risk of unexpectedly dropping a grade in summer examinations".[14]
References
- ↑ "Allergists Explore Rising Prevalence and Unmet Needs Attributed to Allergic Rhinitis". ACAAI (November 12, 2006). Retrieved on 2008-10-01.
- ↑ "Rush University Medical Center". Retrieved on 2008-03-05.
- ↑ Czaja-Bulsa G, Bachórska J (1998). "[Food allergy in children with pollinosis in the Western sea coast region]". Pol Merkur Lekarski 5 (30): 338–40. PMID 10101519.
- ↑ Yamamoto T, Asakura K, Shirasaki H, Himi T, Ogasawara H, Narita S, Kataura A (2005). "[Relationship between pollen allergy and oral allergy syndrome]". Nippon Jibiinkoka Gakkai Kaiho 108 (10): 971–9. PMID 16285612.
- ↑ Malandain H (2003). "[Allergies associated with both food and pollen]". Allerg Immunol (Paris) 35 (7): 253–6. PMID 14626714.
- ↑ "The Facts about Hay Fever". Healthlink. University of Wisconsin. Retrieved on 2007-06-19.
- ↑ "NHS advice on hayfever".
- ↑
- ↑ Susan O'Meara, Paul Wilson, Chris Bridle, Jos Kleijnen and Kath Wright (2002). "Effective Health Care: Homeopathy" (PDF). NHS Centre for Reviews and Dissemination. Retrieved on 2007-06-10. "There are currently insufficient data ... to recommend homeopathy as a treatment for any specific condition"
- ↑ Passalacqua G, Bousquet PJ, Carlsen KH, Kemp J, Lockey RF, Niggemann B, Pawankar R, Price D, Bousquet J (2006). "ARIA update: I--Systematic review of complementary and alternative medicine for rhinitis and asthma". J. Allergy Clin. Immunol. 117 (5): 1054–62. doi:. PMID 16675332.
- ↑ Terr A (2004). "Unproven and controversial forms of immunotherapy". Clin Allergy Immunol. 18 (1): 703–10. PMID 15042943.
- ↑ World Health Organisation (2002). Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials. 87. ISBN 9789241545433.
- ↑ (Furthermore, it should be noted that honeybees visit precisely those plants that are not pollinated by the wind and are, therefore, less likely to cause allergic rhinitis.) TV Rajan, H Tennen, RL Lindquist, L Cohen, J Clive (February 2002). "Effect of ingestion of honey on symptoms of rhinoconjunctivitis". Annals of allergy, asthma & immunology 88 (2): 198–203. ISSN 1081-1206. PMID 11868925. "This study does not confirm the widely held belief that honey relieves the symptoms of allergic rhinoconjunctivitis".
- ↑ Walker S, Khan-Wasti S, Fletcher M, Cullinan P, Harris J, Sheikh A (2007). "Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study". J. Allergy Clin. Immunol. 120 (2): 381–7. doi:. PMID 17560637.
External links
- Specialist Library for ENT and Audiology Hay fever resources - online library of high quality research on hay fever and other ENT disorders
- American Academy of Otolaryngic Allergy
- American Academy of Allergy, Asthma & Immunology
- Sinus Infection And Hay Fever
- Ancient Herbal Remedy Beats Hayfever
- Asthma and Allergy Foundation of America – patient advocacy organization
- American Board of Allergy – ABAI establishes qualifications and examines physicians to become recognized specialists in allergy and immunology in the USA
- Daily Pollen Count in the USA
- Hay Fever information page. Asthma and Allergy Foundation of America
- Information on hay fever and children from Seattle Children's Hospital
- eMedicine Health
- Hayfever forum
- Hayfever and acupuncture
- Could you host a hookworm? Nottingham (UK) Hayfever Hookworm Trials
- David Beaulieu. "Giant Ragweed: Allergy Plants". About.com. Retrieved on 2006-09-19. – Giant ragweed is a major source of fall allergies, site helps to identify the weed with included pictures.
- Clinical trial of a new nasal spray for the treatment of hayfever at the Woolcock Institute (Sydney, Au)
- Seasonal Allergic Rhinitis, Steven Jay WEISS MD.
|
||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
|||||||||||||||||