Human papillomavirus
| Human papillomavirus | ||||||
|---|---|---|---|---|---|---|
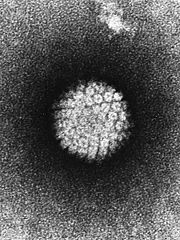 EM of papillomavirus
|
||||||
| Virus classification | ||||||
|
||||||
| Genera | ||||||
|
Alphapapillomavirus |
| Human Papilloma Viruses Classification and external resources |
|
| ICD-10 | B97.7 |
|---|---|
| ICD-9 | 078.1 079.4 |
| DiseasesDB | 6032 |
| eMedicine | med/1037 |
| MeSH | D030361 |
A human papillomavirus (HPV) is a papillomavirus that infects the skin and mucous membranes of humans. Approximately 130 HPV types have been identified. Some HPV types can cause warts (verrucae) or cancer, while others have no symptoms.
About 30-40 HPV types are typically transmitted through sexual contact and infect the anogenital region. Some sexually transmitted HPV types may cause genital warts, while others do not cause any noticeable signs of infection.
Persistent infection with "high-risk" HPV types — different from the ones that cause warts — may progress to precancerous lesions and invasive cancer. HPV infection is a cause of nearly all cases of cervical cancer.[1]
A cervical Pap smear is used to detect cellular abnormalities. This allows targeted surgical removal of condylomatous and/or potentially precancerous lesions prior to the development of invasive cervical cancer. Although the widespread use of Pap testing has reduced the incidence and lethality of cervical cancer in developed countries, the disease still kills several hundred thousand women per year worldwide.[2] HPV vaccines Gardasil and Cervarix, which prevent infection with some of the sexually transmitted HPV types that cause the most disease may lead to further decreases in the incidence of HPV-induced cancers.[3]
Contents |
Prevalence
United States
Estimates of prevalence vary from 14% to more than 90%.[4] One reason for the difference is that some studies report women who currently have a detectable infection, while other studies report women who have ever had a detectable infection.[5][6] Another cause of discrepancy is the difference in strains that were tested for.
HPV is the most common sexually transmitted infection in the United States.[7] According to the National Cervical Cancer Coalition (NCCC), 11% of American women do not have regular cervical cancer screenings. Women who do not have regular cervical cancer screenings substantially increase their risk of developing cancer[2], because precancerous lesions will not be detected and removed. The American Cancer Society estimates that in 2008, about 11,070 women in the United States will be diagnosed with invasive cervical cancer, and about 3,870 US women will die from this disease.[8] Most cases of HPV infection which become cancerous are due to a failure to get regular checkups and removal of precancerous lesions. [9] Death from mere HPV infection is unlikely if a woman has regular checkups and participates in necessary follow-up procedures such as removal of lesions.
One study found that, during 2003–2004, at any given time, 26.8% of women aged 14 to 59 were infected with at least one type of HPV. This was higher than previous estimates. 15.2% were infected with one or more of the high-risk types that can cause cancer. However only 3.4% were infected with one or more of the four types prevented by the Gardasil vaccine, which was lower than previous estimates.[7][10]
| Age (years) | Prevalence (%) |
|---|---|
| 14 to 19 | 24.5% |
| 20 to 24 | 44.8% |
| 25 to 29 | 27.4% |
| 30 to 39 | 27.5% |
| 40 to 49 | 25.2% |
| 50 to 59 | 19.6% |
| 14 to 59 | 26.8% |
Note that incidence decreases with age. This is most likely due to the fact that HPV infection can clear with time, or at least sink to harmless and undetectable levels while still present in the body.
The concern about life-long recurrences may be based on a misconception rather than a myth. It is true that at present there is no cure for genital human papillomavirus. It will probably remain in the infected person's cells for an indefinite time--most often in a latent state, but occasionally producing symptoms or disease.
Recent studies from the Albert Einstein College of Medicine and from the University of Washington suggest that HPV may eventually be cleared, or rooted out altogether, in most people with well functioning immune systems. It appears that in some cases the virus does remain in the body indefinitely, producing symptoms if the immune system weakens.
It was estimated that in the year 2000, there were approximately 6.2 million new HPV infections among Americans aged 15-44; of these, an estimated 74% occurred to people between ages 15-24.[11] Of the STDs studied, genital HPV was the most commonly acquired.[11]
Genital HPV is the most common sexually transmitted infection. Most sexually active men and women will probably acquire genital HPV infection at some point in their lives.[12] The American Social Health Association reported estimates that about 75-80% of sexually active Americans will be infected with HPV at some point in their lifetime.[13][14] According to the Centers for Disease Control (CDC), by the age of 50 more than 80% of American women will have contracted at least one strain of genital HPV.[15]
HPV lifecycle
The HPV lifecycle strictly follows the differentiation program of the host keratinocyte. It is thought that the HPV virion infects epithelial tissues through micro-abrasions, whereby the virion associates with putative receptors such as alpha integrins and laminins, leading to entry of the virions into basal epithelial cells through clathrin-mediated endocytosis and/or caveolin-mediated endocytosis depending on the type of HPV. At this point, the viral genome is transported to the nucleus by unknown mechanisms and establishes itself at a copy number between 10-200 viral genomes per cell. A sophisticated transcriptional cascade then occurs as the host keratinocyte begins to divide and become increasingly differentiated in the upper layers of the epithelium. The viral oncogenes, E6 and E7, are thought to modify the cell cycle so as to retain the differentiating host keratinocyte in a state that is amiable to the amplification of viral genome replication and consequent late gene expression. E6 in association with host E6 AP (associated protein), which has ubiquitin ligase activity act to ubiquitinate p53 leading to its proteosomal degradation. E7 (inoncogenic HPV's) acts as the primary transforming protein. E7 competes for pRb binding, freeing the transcription factor E2F to transactivate its targets, thus pushing the cell cycle forwards. All HPV can induce transient proliferation, but only 16 and 18 can immortalise cell intes (in vitro). It has also been shown that HPV 16 and 18 cannot immortalise primary rat cells alone, there needs to be activation of the ras oncogene. In the upper layers of the host epithelium, the late genes L1 and L2 are transcribed/translated and serve as structural proteins which encapsidate (Encapsidation is the process of incorporating a nucleic acid sequence (e.g., a vector, or a viral genome) into a viral particle) the amplified viral genomes. Virions can then be sloughed off in the dead squames of the host epithelium and the viral lifecycle continues.
Latency period
Once an HPV viron invades a cell, an active infection occurs, and the virus can be transmitted. Several months to years may elapse before squamous intraepithelial lesions (SIL) develop and can be clinically detected. The time from active infection to clinically detectable disease makes it difficult for someone who has become infected to establish which partner was the source of infection.
HPV types and associated diseases

Over 100 different HPV types have been identified and are referred to by number. Types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68 are "high-risk" sexually transmitted HPVs and may lead to the development of cervical intraepithelial neoplasia (CIN), vulvar intraepithelial neoplasia (VIN), penile intraepithelial neoplasia (PIN), and/or anal intraepithelial neoplasia (AIN).
| Disease | HPV type |
|---|---|
| Common warts | 2, 7 |
| Plantar warts | 1, 2, 4 |
| Flat warts | 3, 10 |
| Anogenital warts | 6, 11, 42, 43, 44, 55 and others |
| Genital cancers | 16, 18, 31, 33, 35, 39, 45, 51 |
| Epidermodysplasia verruciformis | more than 15 types |
| Focal epithelial hyperplasia (oral) | 13, 32 |
| Oral papillomas | 6, 7, 11, 16, 32 |
Cancer

- See also: Cervical cancer
About a dozen HPV types (including types 16, 18, 31 and 45) are called "high-risk" types because they can lead to cervical cancer, as well as anal cancer, vulvar cancer, and penile cancer.[16] Several types of HPV, particularly type 16, have been found to be associated with oropharyngeal squamous-cell carcinoma, a form of head and neck cancer.[17] HPV-induced cancers often have viral sequences integrated into the cellular DNA. Some of the HPV "early" genes, such as E6 and E7, are known to act as oncogenes that promote tumor growth and malignant transformation.
The p53 protein prevents cell growth in the presence of DNA damage primarily through the BAX domain, which blocks the anti-apoptotic effects of the mitochondrial BCL-2 receptor. In addition, p53 also upregulates the p21 protein, which blocks the formation of the Cyclin D/Cdk4 complex, thereby preventing the phosphorylation of RB and, in turn, halting cell cycle progression by preventing the activation of E2F. In short, p53 is a tumor suppressor gene that arrests the cell cycle when there is DNA damage. The E6 and E7 proteins work by inhibiting tumor suppression genes involved in that pathway: E6 inhibits p53, while E7 inhibits p53, p21, and RB.

An infection with one or more high-risk HPV types is believed to be a prerequisite for the development of cervical cancer (the vast majority of HPV infections are not high risk); according to the American Cancer Society, women with no history of the virus do not develop this type of cancer. However, most HPV infections are cleared rapidly by the immune system and do not progress to cervical cancer. Because the process of transforming normal cervical cells into cancerous ones is slow, cancer occurs in people who have been infected with HPV for a long time, usually over a decade or more.[18][19]
Sexually transmitted HPVs also cause a major fraction of anal cancers and approximately 25% of cancers of the mouth and upper throat (known as the oropharynx) (see figure). The latter commonly present in the tonsil area and HPV is linked to the increase in oral cancers in non-smokers.[20][21] Engaging in anal sex or oral sex with an HPV-infected partner may increase the risk of developing these types of cancers.[17]
Studies show a link between HPV infection and penile and anal cancer, and the risk for anal cancer is 17 to 31 times higher among gay and bisexual men than among heterosexual men.[22][23]
Warts
Skin warts
Some HPV infections can cause warts (verrucae), which are noncancerous skin growths. Infection with these types of HPV causes a rapid growth of cells on the outer layer of the skin.[24] Types of warts include:
- Common warts: Some "cutaneous" HPV types, such as HPV-1 and HPV-2, cause common skin warts. Common warts are often found on the hands and feet, but can also occur in other areas, such as the elbows or knees. Common warts have a characteristic cauliflower-like surface and are typically slightly raised above the surrounding skin. Cutaneous HPV types do not usually cause genital warts and are not associated with the development of cancer.
- Plantar warts are found on the soles of the feet. Plantar warts grow inward, generally causing pain when walking.
- Subungual or periungual warts form under the fingernail (subungual), around the fingernail or on the cuticle (periungual). They may be more difficult to treat than warts in other locations.[25]
- Flat warts: Flat warts are most commonly found on the arms, face or forehead. Like common warts, flat warts occur most frequently in children and teens. In people with normal immune function, flat warts are not associated with the development of cancer.[26]
Genital warts are quite contagious, while common, flat, and plantar warts are much less likely to spread from person to person.
Genital warts
Genital or anal warts (condylomata acuminata or venereal warts) are the most easily recognized sign of genital HPV infection. Although a wide variety of HPV types can cause genital warts, types 6 and 11 account for about 90% of all cases.[27][28]
Most people who acquire genital wart-associated HPV types clear the infection rapidly without ever developing warts or any other symptoms. People may transmit the virus to others even if they don't display overt symptoms of infection.
HPV types that tend to cause genital warts are not the same ones that cause cervical cancer.[29] However, since an individual can be infected with multiple types of HPV, the presence of warts does not rule out the possibility of high risk types of the virus also being present.
Respiratory papillomatosis
HPV types 6 and 11 can cause a rare condition known as recurrent respiratory papillomatosis, in which warts form on the larynx or other areas of the respiratory tract.[30][19]
These warts can recur frequently, may require repetitive surgery, may interfere with breathing, and in extremely rare cases can progress to cancer.[31][19]
HPV in immunocompromised patients
In very rare cases, HPV may cause epidermodysplasia verruciformis in immunocompromised individuals. The virus, unchecked by the immune system, causes the overproduction of keratin by skin cells, resulting in lesions resembling warts or cutaneous horns.[32]
For instance, Dede Koswara, an Indonesian man developed warts that spread across his body and became root-like growths. Attempted treatment by both Indonesian and American doctors included surgical removal of the warts.
Cervical cancer prevention
Avoiding sexual contact with an infected person is the only 100% effective prevention method; however, many people are unaware that they are infected with HPV. Condoms offer some protection, but exposed skin can transmit the virus. Two vaccines are currently available (see "HPV vaccines" below) to women between the ages of 9 and 26.
Pap smear screening

Certain types of sexually transmitted HPVs can cause cervical cancer. Persistent infection with one or more of about a dozen of these "high-risk" HPV types is an important factor in nearly all cases of cervical cancer. The development of HPV-induced cervical cancer is a slow process that generally takes many years. During this development phase, pre-cancerous cells can be detected by regular cervical cytology Papanicolaou screening, colloquially known as "Pap" smear testing. The Pap test is an effective strategy for reducing the risk of invasive cervical cancer. The Pap test involves taking cells from the cervix and putting them on a small glass slide and examining them under a microscope to look for abnormal cells. This method is 70% to 80% effective in detecting HPV-caused cellular abnormalities. A more sensitive method is a “Thin Prep,” in which the cells from the cervix are placed in a liquid solution. This test is 85% to 95% effective in detecting HPV-caused cellular abnormalities. The latter method is mainly used on women over 30. It is a combination Pap-HPV DNA test. If this test comes back negative women can usually wait 3 years before having the test done again. Detailed inspection of the cervix by colposcopy may be indicated if abnormal cells are detected by routine Pap smear. A frequently occurring example of an abnormal cell found in association with HPV is the koilocyte. (See figure.) The American College of Obstetricians and Gynecologists states that the newer liquid based cytology methods (Thinprep and Surepath) may miss 15-35% of CIN3's and cancer.
The Center for Disease Control (CDC) recommends that women get a Pap test no later than 3 years after their first sexual encounter and no later than 21 years of age. Women should have a Pap test every year until age 30. After age 30, women should discuss risk factors with their health care provider to determine whether a Pap test should be done yearly. If risk factors are low and previous Pap tests have been negative, most women only need to have tests every 2-3 years until 65 years of age (Centers for Disease Control 2005). All women are encouraged to get a yearly pap smear solely to detect cellular abnormalities caused by HPV.[15]
Since the Pap test was developed there has been a 70% decrease in cervical cancer deaths over the last 50 years. Pap smear testing has proven to be one of the most successful screening tests in the history of medicine.
A study published in April 2007 suggests that the act of performing a Pap smear produces an inflammatory cytokine response, which may initiate immunologic clearance of HPV, therefore reducing the risk of cervical cancer. Women who had even a single Pap smear in their history had a lower incidence of cancer. "A statistically significant decline in the HPV positivity rate correlated with the lifetime number of Pap smears received."[33]
It has been suggested that anal Pap smear screening for anal cancer might benefit some sub-populations of men or women who engage in anal sex.[34]
HPV testing
The HPV test detects many common "low" and "high-risk" HPV genotypes. This test is an important screening option, since a doctor may recommend more frequent Pap testing if the HPV test is positive for "high-risk" HPV. In March 2003, the US FDA approved a "hybrid-capture" test, marketed by Digene, as a primary screening tool for detecting HPV. This test was also approved for use as an adjunct to Pap testing, and may be performed during a routine Pap smear.
When patients are screened with both HPV testing and Pap testing the sensitivity reaches 100%. HPV testing can diagnose CIN 2-3 among women older than 30 years.[35] The sensitivity of HPV testing alone was 94.6% and specificity was 94.1%. For patients at similar risk to those in this study (0.4% had CIN 2-3), this leads to a positive predictive value of 6.0% and negative predictive value of 100.0% (click here to adjust these results for patients at higher or lower risk of CIN 2-3).
The CDC states on its "STD Facts-HPV Vaccine" page that "An HPV test or a Pap test can tell that a woman may have HPV, but these tests cannot tell the specific HPV type(s) that a woman has."[15]
In Australia, a self-sampling HPV DNA test - that women can do at home using an ordinary tampon - is being marketed by Tam Pap. It has been approved by the Therapeutic Goods Administration for distribution in Australia.
The recent outcomes in the identification of molecular pathways involved in cervical cancer provide helpful information about novel biomarkers that allow monitoring these essential molecular events in histological or cytological specimens. These biomarkers are likely to improve the detection of lesions that have a high risk of progression in both primary screening and triage settings. E6 and E7 mRNA detection (HPV OncoTect) or p16 cell-cycle protein levels are examples of these new molecular markers. According to published results these markers, which are highly sensitive and specific, allow to identify cells going through malignant transformation. [36]
HPV testing in males
Although it is possible to test for HPV DNA in men,[37] there are no FDA-approved tests for general screening in the United States[22] or tests approved by the Canadian government[38], since the testing is inconclusive and considered medically unnecessary.[39]
Genital warts are the only visible sign of low-risk HPV in men, and can be identified with a visual check of the genital area. These visible growths, however, are the result of non-carcinogenic HPV types. 5% acetic acid (vinegar) is used to identify both warts and squamous intraepithelial neoplasia (SIL) lesions with limited success[22] by causing abnormal tissue to appear white, but most doctors have found this technique helpful only in moist areas, such as the female genital tract.[22]
HPV vaccines
On June 8, 2006, the US Food and Drug Administration approved Gardasil, a prophylactic HPV vaccine which is marketed by Merck. The vaccine trial,[40] conducted in adult women with a mean age of 23, showed protection against initial infection with HPV types 16 and 18, which together cause 70% of cervical cancers, and can cause other cancers, such as anal cancer. The vaccine also protects against HPV types 6 and 11, which cause 90 percent of genital warts.
GlaxoSmithKline is seeking approval for a prophylactic vaccine known as Cervarix targeting HPV types 16 and 18. It is delivered in three shots over six months. It is intended for females from 10 years of age onwards.[41]
Gardasil vaccine is delivered in a series of three shots over six months at a cost of approximately $360 (US dollars). The CDC recommends that girls and women between the ages of 11 and 26 be vaccinated,[15] though girls as young as 9 may benefit.[42] Females not yet sexually active can be expected to receive the full benefit of vaccination. Women over 26 can be vaccinated at the discretion of a doctor, but the vaccination has not yet been approved by the FDA for this age range, and may not be covered by insurance. Studies have not yet conclusively shown benefits for patients over 26, possibly due to the high prevalence of infection and the fact that the vaccine has no effect upon current infections.
HPV vaccine is made up of proteins from the outer coat of the virus (HPV). There is no infectious material in this vaccine. There is also no thimerosal, a mercury based preservative, in the HPV vaccine.[15] This vaccine has been tested in over 11,000 females (ages 9-26 years) around the world. These studies have shown no serious side effects. The most common side effect is soreness at the injection site. CDC, working with the FDA, will continue to monitor the safety of the vaccine after it is in general use.[43]
The vaccine does not appear to protect against HPV types that females are infected with at the time of vaccination. However, females already infected with one or more vaccine HPV types before vaccination would be protected against disease caused by the other vaccine HPV types covered by the vaccine. Therefore, although overall vaccine effectiveness would be lower when administered to females who have been sexually active, and would decrease with age and likelihood of HPV exposure with increasing number of sex partners, the majority of females in this age group will derive at least partial benefit from vaccination. The vaccine will not have any therapeutic effect on existing HPV infection or cervical lesions.[44]
Since the current vaccine will not protect women against all the HPV types that cause cervical cancer, women should continue to seek Pap smear testing, even after receiving the vaccine. Cervical cancer screening recommendations have not changed for females who receive HPV vaccine.[44]
Both men and women are carriers of HPV.[45] Possible benefits or efficacy of vaccinating men are being studied.
In addition to preventive vaccines, laboratory research and several human clinical trials are focused on the development of therapeutic HPV vaccines. In general, these vaccines focus on the main HPV oncogenes E6 and E7. Since expression of E6 and E7 is required for promoting the growth of cervical cancer cells (and cells within warts), it is hoped that immune responses against the two oncogenes might eradicate established tumors.[46]
Smoking avoidance
Carcinogens from tobacco and second-hand smoke are concentrated in the cervix, increasing rate of dysplasia by four to five times, and doubling the risk of cervical cancer.[47]
Condoms
The Centers for Disease Control and Prevention says that "While the effect of condoms in preventing HPV infection is unknown, condom use has been associated with a lower rate of cervical cancer, an HPV-associated disease."[29]
According to Marcus Steiner and Willard Cates in the New England Journal of Medicine, "the protection that condoms offer cannot be precisely quantified."[48] However, in a study reported in the same issue,[49] of 82 female university students followed for eight months, the incidence of genital HPV infection was 37.8 per 100 patient-years among women whose partners used condoms for all instances of intercourse, compared with 89.3 per 100 patient-years in women whose partners used condoms less than 5% of the time. The researchers concluded that "Among newly sexually active women, consistent condom use by their partners appears to reduce the risk of cervical and vulvovaginal HPV infection."
Other studies have suggested that regular condom use can effectively limit the ongoing persistence and spread of HPV to additional genital sites in individuals who are already infected.[50][51]
Thus, condom use may reduce the risk that infected individuals will progress to cervical cancer or develop additional genital warts. Planned Parenthood recommends condom use to reduce the risk of contracting HPV.[52]
Microbicides
Ongoing research has suggested that several inexpensive chemicals might serve to block HPV transmission if applied to the genitals prior to sexual contact.[53] These candidate agents, known as topical microbicides, are currently undergoing clinical efficacy testing. A recent study indicates that some sexual lubricant brands that use a gelling agent called carrageenan can inhibit papillomavirus infection in vitro.[54] See Carrageenan#Sexual lubricant and microbicide for details.
Clinical trials are needed to determine whether carrageenan-based sexual lubricant gels are effective for blocking the sexual transmission of HPVs in vivo.
Nutrition
Fruits and vegetables
Higher levels of vegetable consumption were associated with a 54% decrease risk of HPV persistence.[55] Consumption of papaya at least once a week was inversely associated with persistent HPV infection.[56]
Vitamin A
There is weak evidence to suggest a significant deficiency of retinol can increase chances of cervical dysplasia, independently of HPV infection. A small (n~=500) case-control study of a narrow ethnic group (native Americans in New Mexico) assessed serum micro-nutrients as risk factors for cervical dysplasia. Subjects in the lowest serum retinol quartile were at increased risk of CIN I compared with women in the highest quartile.[57]
However, the study population had low overall serum retinol, suggesting deficiency. A study of serum retinol in a well-nourished population reveals that the bottom 20% had serum retinol close to that of the highest levels in this New Mexico sub-population.[58]
Vitamin C
Risk of type-specific, persistent HPV infection was lower among women reporting intake values of vitamin C in the upper quartile compared with those reporting intake in the lowest quartile.[59]
Vitamin E
HPV clearance time was significantly shorter among women with the highest compared with the lowest serum levels of tocopherols, but significant trends in these associations were limited to infections lasting </=120 days. Clearance of persistent HPV infection (lasting >120 days) was not significantly associated with circulating levels of tocopherols. Results from this investigation support an association of micronutrients with the rapid clearance of incident oncogenic HPV infection of the uterine cervix.[60]
A statistically significantly lower level of alpha-tocopherol was observed in the blood serum of HPV-positive patients with cervical intraepithelial neoplasia. The risk of dysplasia was four times higher for an alpha-tocopherol level < 7.95 mumol/l.[61]
Folic acid
Higher folate status was inversely associated with becoming HPV test-positive. Women with higher folate status were significantly less likely to be repeatedly HPV test-positive and more likely to become test-negative. Studies have shown that lower levels of antioxidants coexisting with low levels of folic acid increases the risk of CIN development. Improving folate status in subjects at risk of getting infected or already infected with high-risk HPV may have a beneficial impact in the prevention of cervical cancer.[62][63]
However, another study showed no relationship between folate status and cervical dysplasia.[57]
Carotenoids
Higher circulating levels of carotenoids were associated with a significant decrease in the clearance time of type-specific HPV infection, particularly during the early stages of infection (</=120 days). Clearance of persistent HPV infection (lasting >120 days) was not significantly associated with circulating levels of carotenoids.[60]
The likelihood of clearing an oncogenic HPV infection is significantly higher with increasing levels of lycopenes.[64] A 56% reduction in HPV persistence risk was observed in women with the highest plasma [lycopene] concentrations compared with women with the lowest plasma lycopene concentrations. These data suggests that vegetable consumption and circulating lycopene may be protective against HPV persistence.[55][56][65]
CoQ10
Women who had either CIN or cervical cancer had markedly lower levels of CoQ10 in their blood and in their cervical cells than the women who were healthy.
Fish oil
In a 1999 study, Docosahexaenoic acid inhibited growth of HPV16 immortalized cells.[66]
Treatment
"There is currently no cure or treatment for HPV infection."[47][15]
Therapies for conditions caused by HPV are addressed in main articles covering the various HPV-related diseases.
Epidemiology
Cutaneous HPVs
Infection with cutaneous HPVs is ubiquitous.[67] Some HPV types, such as HPV-5, may establish infections that persist for the lifetime of the individual without ever manifesting any clinical symptoms. Like remora suckerfish that hitchhike harmlessly on sharks, these HPV types can be thought of as human commensals. Other cutaneous HPVs, such as HPV types 1 or 2, may cause common warts in some infected individuals. Skin warts are most common in childhood and typically appear and regress spontaneously over the course of weeks to months. About 10% of adults also suffer from recurring skin warts. All HPVs are believed to be capable of establishing long-term "latent" infections in small numbers of stem cells present in the skin. Although these latent infections may never be fully eradicated, immunological control is thought to block the appearance of symptoms such as warts. Immunological control is likely HPV type-specific, meaning that an individual may become immunologically resistant to one HPV type while remaining susceptible to other types.
Genital HPVs
A large increase in the incidence of genital HPV infection occurs at the age when individuals begin to engage in sexual activity. The great majority of genital HPV infections never cause any overt symptoms and are cleared by the immune system in a matter of months. As with cutaneous HPVs, immunity is believed to be HPV type-specific. Some infected individuals may fail to bring genital HPV infection under immunological control. Lingering infection with high-risk HPV types, such as HPVs 16, 18, 31 and 45, can lead to the development of cervical cancer or other types of cancer.[68] In addition to persistent infection with high-risk HPV types, epidemiological and molecular data suggest that co-factors such as the cigarette smoke carcinogen benzo[a]pyrene (BaP) enhance development of certain HPV-induced cancers.[69]
High-risk HPV types 16 and 18 are together responsible for over 65% of cervical cancer cases.[70][12] Type 16 causes 41 to 54% of cervical cancers,[71][12] and accounts for an even greater majority of HPV-induced vaginal/vulvar cancers,[72] penile cancers, anal cancers and head and neck cancers.[73]
Perinatal transmission
Although genital HPV types are sometimes transmitted from mother to child during birth, the appearance of genital HPV-related diseases in newborns is rare. Perinatal transmission of HPV types 6 and 11 can result in the development of juvenile-onset recurrent respiratory papillomatosis (JORRP). JORRP is very rare, with rates of about 2 cases per 100,000 children in the United States.[19] Although JORRP rates are substantially higher if a woman presents with genital warts at the time of giving birth, the risk of JORRP in such cases is still less than 1%.
History of discovering link between virus and cancer
- See also: Cervical cancer#History
The fact that prostitutes have much higher rates of cervical cancer than nuns was a key early observation leading researchers to speculate about a causal link between sexually transmitted HPVs and cervical cancer.[74]
Dr. Harald zur Hausen of the German Cancer Research Centre, Heidelberg, Germany, was awarded 2008 Nobel Prize in Physiology or Medicine for his discovery of human papilloma viruses causing cervical cancer.[75]
See also
- Loop electrical excision procedure
- koilocyte
References
- ↑ Walboomers JM, Jacobs MV, Manos MM, et al (1999). "Human papillomavirus is a necessary cause of invasive cervical cancer worldwide". J. Pathol. 189 (1): 12–9. doi:. PMID 10451482.
- ↑ 2.0 2.1 "NCCC National Cervical Cancer Coalition". Retrieved on 2008-07-01.
- ↑ Lowy DR, Schiller JT (2006). "Prophylactic human papillomavirus vaccines". J. Clin. Invest. 116 (5): 1167–73. doi:. PMID 16670757.
- ↑ Revzina NV, Diclemente RJ (2005). "Prevalence and incidence of human papillomavirus infection in women in the USA: a systematic review". International journal of STD & AIDS 16 (8): 528–37. doi:. PMID 16105186."The prevalence of HPV reported in the assessed studies ranged from 14% to more than 90%."
- ↑ McCullough, Marie (2007-02-28). "Cancer-virus strains rarer than first estimated", The Philadelphia Inquirer. Retrieved on 2007-03-02.
- ↑ Brown, David (2007-02-28). "Study finds more women than expected have HPV", San Francisco Chronicle. Retrieved on 2007-03-02. (originally published in the Washington Post as "More American Women Have HPV Than Previously Thought")
- ↑ 7.0 7.1 7.2 Dunne EF, Unger ER, Sternberg M, et al (2007). "Prevalence of HPV infection among females in the United States". JAMA 297 (8): 813–9. doi:. PMID 17327523.
- ↑ "ACS:What Are the Key Statistics About Cervical Cancer?". Retrieved on 2008-07-01.
- ↑ "Pap Smear". Retrieved on 2008-10-09.
- ↑ Lindsey Tanner (March 11, 2008). "Study Finds 1 in 4 US Teens Has a STD". Newsvine. Retrieved on 2008-03-17.
- ↑ 11.0 11.1 Hillard Weinstock, Stuart Berman and Willard Cates, Jr. (January/February 2004). "Sexually Transmitted Diseases Among American Youth: Incidence and Prevalence Estimates, 2000". Perspectives on Sexual and Reproductive Health 36 (1): 6. doi:. http://www.guttmacher.org/pubs/journals/3600604.html.
- ↑ 12.0 12.1 12.2 Baseman JG, Koutsky LA (2005). "The epidemiology of human papillomavirus infections". J. Clin. Virol. 32 Suppl 1: S16–24. doi:. PMID 15753008. *Note: The authors state on page S17 "Overall, these DNA-based studies, combined with measurements of type-specific antibodies against HPV capsid antigens, have shown that most (>50%) sexually active women have been infected by one or more genital HPV types at some point in time."
- ↑ "American Social Health Association - HPV Resource Center". Retrieved on 2007-08-17.
- ↑ "American Social Health Association - National HPV and Cervical Cancer Prevention Resource Center". Retrieved on 2008-07-01.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 "STD Facts - HPV Vaccine" (2006-08-01). Retrieved on 2007-08-17.
- ↑ Parkin DM (2006). "The global health burden of infection-associated cancers in the year 2002". Int. J. Cancer 118 (12): 3030–44. doi:. PMID 16404738.
- ↑ 17.0 17.1 D'Souza G, Kreimer AR, Viscidi R, et al (2007). "Case-control study of human papillomavirus and oropharyngeal cancer". N. Engl. J. Med. 356 (19): 1944–56. doi:. PMID 17494927. http://content.nejm.org/cgi/content/full/356/19/1944.
- ↑ Greenblatt R.J. 2005. Human papillomaviruses: Diseases, diagnosis, and a possible vaccine. Clinical Microbiology Newsletter, 27(18), 139-145. Abstract available.
- ↑ 19.0 19.1 19.2 19.3 Sinal SH, Woods CR (2005). "Human papillomavirus infections of the genital and respiratory tracts in young children". Seminars in pediatric infectious diseases 16 (4): 306–16. doi:. PMID 16210110.
- ↑ Gillison ML, Koch WM, Capone RB, et al (2000). "Evidence for a causal association between human papillomavirus and a subset of head and neck cancers". J. Natl. Cancer Inst. 92 (9): 709–20. doi:. PMID 10793107.
- ↑ Gillison ML (2006). "Human papillomavirus and prognosis of oropharyngeal squamous cell carcinoma: implications for clinical research in head and neck cancers". J. Clin. Oncol. 24 (36): 5623–5. doi:. PMID 17179099.
- ↑ 22.0 22.1 22.2 22.3 "STD Facts - HPV and Men". Retrieved on 2007-08-17.
- ↑ Frisch M, Smith E, Grulich A, Johansen C (2003). "Cancer in a population-based cohort of men and women in registered homosexual partnerships". Am. J. Epidemiol. 157 (11): 966–72. doi:. PMID 12777359. http://171.66.121.65/cgi/content/full/157/11/966. "However, the risk for invasive anal squamous carcinoma, which is believed to be caused by certain types of sexually transmitted human papillomaviruses, notably type 16, was significantly 31-fold elevated at a crude incidence of 25.6 per 100,000 person-years.".
- ↑ Mayo Clinic.com, Common warts, http://www.mayoclinic.com/print/common-warts/DS00370/DSECTION=all&METHOD=print
- ↑ Lountzis NI, Rahman O (2008). "Images in clinical medicine. Digital verrucae". N. Engl. J. Med. 359 (2): 177. doi:. PMID 18614785. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=18614785&promo=ONFLNS19.
- ↑ MedlinePlus, Warts, http://www.nlm.nih.gov/medlineplus/warts.html#cat42 (general reference with links). Also, see
- ↑ Greer CE, Wheeler CM, Ladner MB, et al (1995). "Human papillomavirus (HPV) type distribution and serological response to HPV type 6 virus-like particles in patients with genital warts". J. Clin. Microbiol. 33 (8): 2058–63. PMID 7559948.
- ↑ Gearheart PA, Randall TC, Buckley RM Jr (2004). "Human Papillomavirus". eMedicine.
- ↑ 29.0 29.1 "STD Facts - Human papillomavirus (HPV)". Retrieved on 2007-08-17.
- ↑ Wu R, Sun S, Steinberg BM (2003). "Requirement of STAT3 activation for differentiation of mucosal stratified squamous epithelium". Mol. Med. 9 (3-4): 77–84. doi:. PMID 12865943.
- ↑ Moore CE, Wiatrak BJ, McClatchey KD, et al (1999). "High-risk human papillomavirus types and squamous cell carcinoma in patients with respiratory papillomas". Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 120 (5): 698–705. doi:. PMID 10229596.
- ↑ Moore, M. "Tree man 'who grew roots' may be cured" (November 21, 2007). The Telegraph.
- ↑ "Pap smears cause cytokine response that may help clear HPV", OncoLink. "J Inflamm 2007;4."
- ↑ Chin-Hong PV, Vittinghoff E, Cranston RD, et al (2005). "Age-related prevalence of anal cancer precursors in homosexual men: the EXPLORE study". J. Natl. Cancer Inst. 97 (12): 896–905. doi:. PMID 15956651.
- ↑ Mayrand MH, Duarte-Franco E, Rodrigues I, et al (2007). "Human papillomavirus DNA versus Papanicolaou screening tests for cervical cancer". N. Engl. J. Med. 357 (16): 1579–88. doi:. PMID 17942871. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=17942871&promo=ONFLNS19.
- ↑ Wentzensen, N. and M. von Knebel Doeberitz, Biomarkers in cervical cancer screening. Dis Markers, 2007. 23(4): p. 315-30.
- ↑ Dunne EF, Nielson CM, Stone KM, Markowitz LE, Giuliano AR (2006). "Prevalence of HPV infection among men: A systematic review of the literature". J. Infect. Dis. 194 (8): 1044–57. doi:. PMID 16991079.
- ↑ "Human Papillomavirus (HPV) and Men: Questions and Answers" (2007). Retrieved on 2008-09-10. "Currently, in Canada there is an HPV DNA test approved for women but not for men."
- ↑ "What Men Need to Know About HPV" (2006). Retrieved on 2007-04-04. "There is currently no FDA-approved test to detect HPV in men. That is because an effective, reliable way to collect a sample of male genital skin cells, which would allow detection of HPV, has yet to be developed."
- ↑ Harper DM, Franco EL, Wheeler CM, et al (2006). "Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: follow-up from a randomised control trial". Lancet 367 (9518): 1247–55. doi:. PMID 16631880.
- ↑ "Cervarix Package Leaflet: Information for the User". Retrieved on 2008-06-21.
- ↑ "HPV and HPV Vaccine - HCP" (2006-08-01). Retrieved on 2007-08-17.
- ↑ "Centers for Disease Control, HPV Vaccine - Questions & Answers For The Public About the Safety and Effectiveness of the Human Papillomavirus (HPV) Vaccine". Retrieved on 2007-06-28.
- ↑ 44.0 44.1 "Quadrivalent Human Papillomavirus Vaccine, Recommendations of the Advisory Committee on Immunization Practices". CDC, Morbidity and Mortality Weekly Report Recommendations 56 / RR-2: 17, Cervical Cancer Screening Among Vaccinated Females. March 23, 2007. http://www.cdc.gov/mmwr/PDF/rr/rr5602.pdf.
- ↑ "HPV Virus: Information About Human Papillomavirus". WebMD.
- ↑ Vaccination to prevent and treat cervical cancer Hum Pathol. 2004 Aug;35(8):971
- ↑ 47.0 47.1 American Cancer Society. "What Are the Risk Factors for Cervical Cancer?". Retrieved on 2008-02-21.
- ↑ Markus J. Steiner and Willard Cates, Jr. (2006). "Condoms and Sexually-Transmitted Infections". N. Engl. J. Med. 354 (25): 2642–3. doi:. PMID 16790696.[1]
- ↑ Winer RL, Hughes JP, Feng Q, et al (2006). "Condom use and the risk of genital human papillomavirus infection in young women". N. Engl. J. Med. 354 (25): 2645–54. doi:. PMID 16790697.[Free online]
- ↑ Moscicki AB (2005). "Impact of HPV infection in adolescent populations". The Journal of adolescent health : official publication of the Society for Adolescent Medicine 37 (6 Suppl): S3–9. PMID 16310138.
- ↑ Bleeker MC, Berkhof J, Hogewoning CJ, et al (2005). "HPV type concordance in sexual couples determines the effect of condoms on regression of flat penile lesions". Br. J. Cancer 92 (8): 1388–92. doi:. PMID 15812547.
- ↑ "Planned Parenthood - HPV". Retrieved on 2007-08-17.
- ↑ Howett MK, Kuhl JP (2005). "Microbicides for prevention of transmission of sexually transmitted diseases". Curr. Pharm. Des. 11 (29): 3731–46. doi:. PMID 16305508.
- ↑ Buck CB, Thompson CD, Roberts JN, Müller M, Lowy DR, Schiller JT (2006). "Carrageenan is a potent inhibitor of papillomavirus infection". PLoS Pathog. 2 (7): e69. doi:. PMID 16839203.
- ↑ 55.0 55.1 Sedjo RL, Roe DJ, Abrahamsen M, et al (2002). "Vitamin A, carotenoids, and risk of persistent oncogenic human papillomavirus infection". Cancer Epidemiol. Biomarkers Prev. 11 (9): 876–84. PMID 12223432.
- ↑ 56.0 56.1 Giuliano AR, Siegel EM, Roe DJ, et al (2003). "Dietary intake and risk of persistent human papillomavirus (HPV) infection: the Ludwig-McGill HPV Natural History Study". J. Infect. Dis. 188 (10): 1508–16. doi:. PMID 14624376.
- ↑ 57.0 57.1 Yeo AS, Schiff MA, Montoya G, Masuk M, van Asselt-King L, Becker TM (2000). "Serum micronutrients and cervical dysplasia in Southwestern American Indian women". Nutrition and cancer 38 (2): 141–50. doi:. PMID 11525590.
- ↑ Michaëlsson K, Lithell H, Vessby B, Melhus H. (2003). "Serum Retinol Levels and the Risk of Fracture". NEJM 348 (4): 287–294. doi:. PMID 12540641.
- ↑ Giuliano AR, Siegel EM, Roe DJ, et al (2003). "Dietary intake and risk of persistent human papillomavirus (HPV) infection: the Ludwig-McGill HPV Natural History Study". J. Infect. Dis. 188 (10): 1508–16. doi:. PMID 14624376.
- ↑ 60.0 60.1 Goodman MT, Shvetsov YB, McDuffie K, et al (2007). "Hawaii cohort study of serum micronutrient concentrations and clearance of incident oncogenic human papillomavirus infection of the cervix". Cancer Res. 67 (12): 5987–96. doi:. PMID 17553901. http://cancerres.aacrjournals.org/cgi/content/full/67/12/5987.
- ↑ Kwaśniewska A, Tukendorf A, Semczuk M (1997). "Content of alpha-tocopherol in blood serum of human Papillomavirus-infected women with cervical dysplasias". Nutrition and cancer 28 (3): 248–51. PMID 9343832.
- ↑ Piyathilake CJ, Henao OL, Macaluso M, et al (2004). "Folate is associated with the natural history of high-risk human papillomaviruses". Cancer Res. 64 (23): 8788–93. doi:. PMID 15574793. http://cancerres.aacrjournals.org/cgi/content/full/64/23/8788.
- ↑ Kwaśniewska A, Tukendorf A, Goździcka-Józefiak A, Semczuk-Sikora A, Korobowicz E (2002). "Content of folic acid and free homocysteine in blood serum of human papillomavirus-infected women with cervical dysplasia". Eur. J. Gynaecol. Oncol. 23 (4): 311–6. PMID 12214730.
- ↑ Sedjo RL, Papenfuss MR, Craft NE, Giuliano AR (2003). "Effect of plasma micronutrients on clearance of oncogenic human papillomavirus (HPV) infection (United States)". Cancer Causes Control 14 (4): 319–26. doi:. PMID 12846362.
- ↑ Giuliano AR, Papenfuss M, Nour M, Canfield LM, Schneider A, Hatch K (1997). "Antioxidant nutrients: associations with persistent human papillomavirus infection". Cancer Epidemiol. Biomarkers Prev. 6 (11): 917–23. PMID 9367065.
- ↑ Chen D, Auborn K (1999). "Fish oil constituent docosahexa-enoic acid selectively inhibits growth of human papillomavirus immortalized keratinocytes". Carcinogenesis 20 (2): 249–54. doi:. PMID 10069461.
- ↑ Antonsson A, Forslund O, Ekberg H, Sterner G, Hansson BG (2000). "The ubiquity and impressive genomic diversity of human skin papillomaviruses suggest a commensalic nature of these viruses". J. Virol. 74 (24): 11636–41. doi:. PMID 11090162.
- ↑ Schiffman M, Castle PE (2005). "The promise of global cervical-cancer prevention". N. Engl. J. Med. 353 (20): 2101–4. doi:. PMID 16291978.
- ↑ Alam S, Conway MJ, Chen HS, Meyers C (2007). "Cigarette Smoke Carcinogen Benzo[a]pyrene Enhances Human Papillomavirus Synthesis". J Virol 82: 1053. doi:. PMID 17989183.
- ↑ Cohen J (2005). "Public health. High hopes and dilemmas for a cervical cancer vaccine". Science 308 (5722): 618–21. doi:. PMID 15860602.
- ↑ Noel J, Lespagnard L, Fayt I, Verhest A, Dargent J (2001). "Evidence of human papilloma virus infection but lack of Epstein-Barr virus in lymphoepithelioma-like carcinoma of uterine cervix: report of two cases and review of the literature". Hum. Pathol. 32 (1): 135–8. doi:. PMID 11172309.
- ↑ Edwards QT, Saunders-Goldson S, Morgan PD, Maradiegue A, Macri C (2005). "Vulvar intraepithelial neoplasia: varied signs, varied symptoms: what you need to know". Advance for nurse practitioners 13 (3): 49–52. PMID 15777042.
- ↑ Bolt J, Vo QN, Kim WJ, McWhorter AJ, Thomson J, Hagensee ME, Friedlander P, Brown KD, Gilbert J (2005). "The ATM/p53 pathway is commonly targeted for inactivation in squamous cell carcinoma of the head and neck (SCCHN) by multiple molecular mechanisms". Oral Oncol. 41 (10): 1013–20. doi:. PMID 16139561.
- ↑ zur Hausen H, de Villiers EM (1994). "Human papillomaviruses". Annu. Rev. Microbiol. 48: 427–47. doi:. PMID 7826013.
- ↑ http://nobelprize.org/nobel_prizes/medicine/laureates/2008/
External links
- Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER (2007). "Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR Recomm Rep 56 (RR-2): 1–24. PMID 17380109. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5602a1.htm.
- HPV Fact sheets from the Centers for Disease Control and Prevention
- Myths and misconceptions about HPV — American Social Health Association
- HPV's links to oral cancers peer reviewed information from The Oral Cancer Foundation
- HPV and pregnancy Answers for those pregnant with HPV
- NOW on PBS: "Vaccine Debate" — The political controversy over requiring HPV vaccinations for girls.
- HPV found under the fingernails of young men The Daily, University of Washington
|
||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||