Cervical cancer
| Cervical cancer Classification and external resources |
|
 |
|
|---|---|
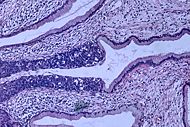
| Histopathologic image (H&E stain) of carcinoma in situ, stage 0. | |
| ICD-10 | C53 |
| ICD-9 | 180 |
| OMIM | 603956 |
| DiseasesDB | 2278 |
| MedlinePlus | 000893 |
| eMedicine | med/324 radio/140 |
| MeSH | D002583 |

Cervical cancer is malignant cancer of the cervix uteri or cervical area. It may present with vaginal bleeding but symptoms may be absent until the cancer is in its advanced stages.[1] Treatment consists of surgery (including local excision) in early stages and chemotherapy and radiotherapy in advanced stages of the disease.
Pap smear screening can identify potentially precancerous changes. Treatment of high grade changes can prevent the development of cancer. In developed countries, the widespread use of cervical screening programs has reduced the incidence of invasive cervical cancer by 50% or more.
Human papillomavirus (HPV) infection is a necessary factor in the development of nearly all cases of cervical cancer.[1][2] HPV vaccine effective against the two strains of HPV that cause the most cervical cancer has been licensed in the U.S. and the EU. These two HPV strains together are currently responsible for approximately 70%[3][4] of all cervical cancers. Since the vaccine only covers some high-risk types, women should seek regular Pap smear screening, even after vaccination.[5]
Contents |
Classification
Cervical cancer is a carcinoma, typically composed of squamous cells, and is similar in some respects to squamous cell cancers of the head and neck and anus. All three of these diseases may be associated with human papillomavirus infection.
Signs and symptoms
The early stages of cervical cancer may be completely asymptomatic.[1][6] Vaginal bleeding, contact bleeding or (rarely) a vaginal mass may indicate the presence of malignancy. Also, moderate pain during sexual intercourse and vaginal discharge are symptoms of cervical cancer. In advanced disease, metastases may be present in the abdomen, lungs or elsewhere.
Symptoms of advanced cervical cancer may include: loss of appetite, weight loss, fatigue, pelvic pain, back pain, leg pain, single swollen leg, heavy bleeding from the vagina, leaking of urine or feces from the vagina,[7] and bone fractures.
Causes
Human papillomavirus infection
The most important risk factor in the development of cervical cancer is infection with a high-risk strain of human papillomavirus. The virus cancer link works by triggering alterations in the cells of the cervix, which can lead to the development of cervical intraepithelial neoplasia, which can lead to cancer.
Women who have many sexual partners (or who have sex with men or women who had many partners) have a greater risk.[8][9]
More than 250 types of HPV are acknowledged to exist (some sources indicate more than 200 subtypes).[10][11] Of these, 15 are classified as high-risk types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82), 3 as probable high-risk (26, 53, and 66), and 12 as low-risk (6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81, and CP6108),[12] but even those may cause cancer. Types 16 and 18 are generally acknowledged to cause about 70% of cervical cancer cases. Together with type 31, they are the prime risk factors for cervical cancer.[13]
Genital warts are caused by various strains of HPV which are usually not related to cervical cancer.
The medically accepted paradigm, officially endorsed by the American Cancer Society and other organizations, is that a patient must have been infected with HPV to develop cervical cancer, and is hence viewed as a sexually transmitted disease, but most women infected with high risk HPV will not develop cervical cancer.[14] Use of condoms reduces, but does not always prevent transmission. Likewise, HPV can be transmitted by skin-to-skin-contact with infected areas. In males, HPV is thought to grow preferentially in the epithelium of the glans penis, and cleaning of this area may be preventative.
Cofactors
The American Cancer Society provides the following list of risk factors for cervical cancer: human papillomavirus (HPV) infection, smoking, HIV infection, chlamydia infection, dietary factors, hormonal contraception, multiple pregnancies, exposure to the hormonal drug diethylstilbestrol (DES) and a family history of cervical cancer.[8] There is a possible genetic risk associated with HLA-B7.
Despite the development of an HPV vaccine, some researchers argue that routine neonatal male circumcision is an acceptable way to lower the risk of cervical cancer in their future female sexual partners. Others maintain that the benefits do not outweigh the risks and/or consider the removal of healthy genital tissue from infants to be unethical as it cannot be reasonably assumed that a male would choose to be circumcised. There has not been any definitive evidence to support the claim that male circumcision prevents cervical cancer, although some researchers say there is compelling epidemiological evidence that men who have been circumcised are less likely to be infected with HPV.[15] However, in men with low-risk sexual behaviour and monogamous female partners, circumcision makes no difference to the risk of cervical cancer.[16]
Diagnosis
Biopsy procedures
While the pap smear is an effective screening test, confirmation of the diagnosis of cervical cancer or pre-cancer requires a biopsy of the cervix. This is often done through colposcopy, a magnified visual inspection of the cervix aided by using a dilute acetic acid (e.g. vinegar) solution to highlight abnormal cells on the surface of the cervix.[1]
Further diagnostic procedures are loop electrical excision procedure (LEEP) and conization, in which the inner lining of the cervix is removed to be examined pathologically. These are carried out if the biopsy confirms severe cervical intraepithelial neoplasia.
Pathologic types
Cervical intraepithelial neoplasia, the precursor to cervical cancer, is often diagnosed on examiniation of cervical biopsies by a pathologist. Histologic subtypes of invasive cervical carcinoma include the following:[17][18] Though squamous cell carcinoma is the cervical cancer with the most incidence, the incidence of adenocarcinoma of the cervix has been increasing in recent decades[1].
- squamous cell carcinoma (about 80-85%)
- adenocarcinoma
- adenosquamous carcinoma
- small cell carcinoma
- neuroendocrine carcinoma
Non-carcinoma malignancies which can rarely occur in the cervix include
Note that the FIGO stage does not incorporate lymph node involvement in contrast to the TNM staging for most other cancers.
For cases treated surgically, information obtained from the pathologist can be used in assigning a separate pathologic stage but is not to replace the original clinical stage.
For premalignant dysplastic changes, the CIN (cervical intraepithelial neoplasia) grading is used.
Staging
Cervical cancer is staged by the International Federation of Gynecology and Obstetrics (FIGO) staging system, which is based on clinical examination, rather than surgical findings. It allows only the following diagnostic tests to be used in determining the stage: palpation, inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, intravenous urography, and X-ray examination of the lungs and skeleton, and cervical conization.
The TNM staging system for cervical cancer is analogous to the FIGO stage.
- Stage 0 - full-thickness involvement of the epithelium without invasion into the stroma (carcinoma in situ)
- Stage I - limited to the cervix
- IA - diagnosed only by microscopy; no visible lesions
- IA1 - stromal invasion less than 3 mm in depth and 7 mm or less in horizontal spread
- IA2 - stromal invasion between 3 and 5 mm with horizontal spread of 7 mm or less
- IB - visible lesion or a microscopic lesion with more than 5 mm of depth or horizontal spread of more than 7 mm
- IB1 - visible lesion 4 cm or less in greatest dimension
- IB2 - visible lesion more than 4 cm
- IA - diagnosed only by microscopy; no visible lesions
- Stage II - invades beyond cervix
- IIA - without parametrial invasion, but involve upper 2/3 of vagina
- IIB - with parametrial invasion
- Stage III - extends to pelvic wall or lower third of the vagina
- IIIA - involves lower third of vagina
- IIIB - extends to pelvic wall and/or causes hydronephrosis or non-functioning kidney
- IVA - invades mucosa of bladder or rectum and/or extends beyond true pelvis
- IVB - distant metastasis
Treatment
Microinvasive cancer (stage IA) is usually treated by hysterectomy (removal of the whole uterus including part of the vagina). For stage IA2, the lymph nodes are removed as well. An alternative for patients who desire to remain fertile is a local surgical procedure such as a loop electrical excision procedure (LEEP) or cone biopsy.[19]
If a cone biopsy does not produce clear margins,[20] one more possible treatment option for patients who want to preserve their fertility is a trachelectomy.[21] This attempts to surgically remove the cancer while preserving the ovaries and uterus, providing for a more conservative operation than a hysterectomy. It is a viable option for those in stage I cervical cancer which has not spread; however, it is not yet considered a standard of care,[22] as few doctors are skilled in this procedure. Even the most experienced surgeon cannot promise that a trachelectomy can be performed until after surgical microscopic examination, as the extent of the spread of cancer is unknown. If the surgeon is not able to microscopically confirm clear margins of cervical tissue once the patient is under general anesthesia in the operating room, a hysterectomy may still be needed. This can only be done during the same operation if the patient has given prior consent. Due to the possible risk of cancer spread to the lymph nodes in stage 1b cancers and some stage 1a cancers, the surgeon may also need to remove some lymph nodes from around the uterus for pathologic evaluation.
A radical trachelectomy can be performed abdominally[23] or vaginally[24] and there are conflicting opinions as to which is better.[25] A radical abdominal trachelectomy with lymphadenectomy usually only requires a two to three day hospital stay, and most women recover very quickly (approximately six weeks). Complications are uncommon, although women who are able to conceive after surgery are susceptible to preterm labor and possible late miscarriage.[26] It is generally recommended to wait at least one year before attempting to become pregnant after surgery.[27] Recurrence in the residual cervix is very rare if the cancer has been cleared with the trachelectomy.[22]Yet, it is recommended for patients to practice vigilant prevention and follow up care including pap screenings/colposcopy, with biopsies of the remaining lower uterine segment as needed (every 3-4 months for at least 5 years) to monitor for any recurrence in addition to minimizing any new exposures to HPV through safe sex practices until one is actively trying to conceive.
Early stages (IB1 and IIA less than 4 cm) can be treated with radical hysterectomy with removal of the lymph nodes or radiation therapy. Radiation therapy is given as external beam radiotherapy to the pelvis and brachytherapy (internal radiation). Patients treated with surgery who have high risk features found on pathologic examination are given radiation therapy with or without chemotherapy in order to reduce the risk of relapse.
Larger early stage tumors (IB2 and IIA more than 4 cm) may be treated with radiation therapy and cisplatin-based chemotherapy, hysterectomy (which then usually requires adjuvant radiation therapy), or cisplatin chemotherapy followed by hysterectomy.
Advanced stage tumors (IIB-IVA) are treated with radiation therapy and cisplatin-based chemotherapy.
On June 15, 2006, the US Food and Drug Administration approved the use of a combination of two chemotherapy drugs, hycamtin and cisplatin for women with late-stage (IVB) cervical cancer treatment.[28] Combination treatment has significant risk of neutropenia, anemia, and thrombocytopenia side effects. Hycamtin is manufactured by GlaxoSmithKline.
Prevention
Awareness
According to the US National Cancer Institute's 2005 Health Information National Trends survey, only 40% of American women surveyed had heard of human papillomavirus (HPV) infection and only 20% had heard of its link to cervical cancer.[29] In 2008 an estimated 3,870 women in the US will die of cervical cancer, and around 11,000 new cases are expected to be diagnosed.[30]
Screening
The widespread introduction of the Papanicolaou test, or Pap smear for cervical cancer screening has been credited with dramatically reducing the incidence and mortality of cervical cancer in developed countries.[6] Abnormal Pap smear results may suggest the presence of cervical intraepithelial neoplasia (potentially premalignant changes in the cervix) before a cancer has developed, allowing examination and possible preventive treatment. Recommendations for how often a Pap smear should be done vary from once a year to once every five years. The American Cancer Society (ACS) recommends that cervical cancer screening should begin approximately three years after the onset of vaginal intercourse and/or no later than twenty-one years of age.[31] Guidelines vary on how long to continue screening, but well screened women who have not had abnormal smears can stop screening about age 65 (USPSTF) to 70 (ACS). If premalignant disease or cervical cancer is detected early, it can be monitored or treated relatively noninvasively, and without impairing fertility.
Until recently the Pap smear has remained the principal technology for preventing cervical cancer. However, following a rapid review of the published literature, originally commissioned by NICE [32], liquid based cytology has been incorporated within the UK national screening programme. Although it was probably intended to improve on the accuracy of the Pap test, its main advantage has been to reduce the number of inadequate smears from around 9% to around 1%.[33] This reduces the need to recall women for a further smear.
Automated technologies have been developed with the aim of improving on the interpretation of smears, normally carried out by cytotechnicians. Unfortunately these on the whole have proven less useful; although the more recent reviews suggest that generally they may be no worse than human interpretation [34].
The HPV test is a newer technique for cervical cancer triage which detects the presence of human papillomavirus infection in the cervix. It is more sensitive than the pap smear (less likely to produce false negative results), but less specific (more likely to produce false positive results) and its role in routine screening is still evolving. Since more than 99% of invasive cervical cancers worldwide contain HPV, some researchers recommend that HPV testing be done together with routine cervical screening.[13] But, given the prevalence of HPV (around 80% infection history among the sexually active population) others suggest that routine HPV testing would cause undue alarm to carriers.
HPV testing can reduce the incidence of grade 2 or 3 cervical intraepithelial neoplasia or cervical cancer detected by subsequent screening tests among women 32-38 years old according to a randomized controlled trial.[35] The relative risk reduction was 41.3%. For patients at similar risk to those in this study (63.0% had CIN 2-3 or cancer), this leads to an absolute risk reduction of 26%. 3.8 patients must be treated for one to benefit (number needed to treat = 3.8). Click here to adjust these results for patients at higher or lower risk of CIN 2-3.
Preventive Vaccination
Merck & Co. has developed a vaccine against four strains of HPV (6,11,16,18), called Gardasil. It is now on the market after receiving approval from the US Food and Drug Administration on June 8, 2006.[3] Gardasil has also been approved in the EU.[36]
GlaxoSmithKline has developed a vaccine called Cervarix which has been shown to be 100% effective in preventing HPV strains 16 and 18 and is effective for more than four years.[37] Cervarix has been approved some places and is in approval process elsewhere.[38]
Neither Merck & Co. nor GlaxoSmithKline invented the vaccine. The vaccine's key developmental steps are claimed by the National Cancer Institute in the US, the University of Rochester in New York, Georgetown University in Washington, DC, Dartmouth College in Hanover, NH, and the Queensland University in Brisbane, Australia. Both Merck & Co. and GlaxoSmithKline have licensed patents from all of these parties.[39]
Together, HPV types 16 and 18 currently cause about 70% of cervical cancer cases. HPV types 6 and 11 cause about 90% of genital wart cases.
HPV vaccines are targeted at girls and women of age 9 to 26 because the vaccine only works if given before infection occurs; therefore, public health workers are targeting girls before they begin having sex. The use of the vaccine in men to prevent genital warts and interrupt transmission to women is initially considered only a secondary market.
The high cost of this vaccine has been a cause for concern. Several countries have or are considering programs to fund HPV vaccination.
Condoms
Condoms may also be useful in treating potentially precancerous changes in the cervix. Exposure to semen appears to increase the risk of precancerous changes (CIN 3), and use of condoms helps to cause these changes to regress and helps clear HPV.[40] One study suggests that prostaglandin in semen may fuel the growth of cervical and uterine tumours and that affected women may benefit from the use of condoms.[41][42]
Prognosis
Prognosis depends on the stage of the cancer. With treatment, the 5-year relative survival rate for the earliest stage of invasive cervical cancer is 92%, and the overall (all stages combined) 5-year survival rate is about 72%. These statistics may be improved when applied to women newly diagnosed, bearing in mind that these outcome may be partly based on the state of treatment five years ago when the women studied were first diagnosed.[30]
With treatment, 80 to 90% of women with stage I cancer and 50 to 65% of those with stage II cancer are alive 5 years after diagnosis. Only 25 to 35% of women with stage III cancer and 15% or fewer of those with stage IV cancer are alive after 5 years.[43]
According to the International Federation of Gynecology and Obstetrics, survival improves when radiotherapy is combined with cisplatin-based chemotherapy.[44]
As the cancer metastasizes to other parts of the body, prognosis drops dramatically because treatment of local lesions is generally more effective than whole body treatments such as chemotherapy.
Interval evaluation of the patient after therapy is imperative. Recurrent cervical cancer detected at its earliest stages might be successfully treated with surgery, radiation, chemotherapy, or a combination of the three. Thirty-five percent of patients with invasive cervical cancer have persistent or recurrent disease after treatment.[45]
Average years of potential life lost from cervical cancer are 25.3 (SEER Cancer Statistics Review 1975-2000, National Cancer Institute (NCI)). Approximately 4,600 women were projected to die in 2001 in the US of cervical cancer (DSTD), and the annual incidence was 13,000 in 2002 in the US, as calculated by SEER. Thus the ratio of deaths to incidence is approximately 35.4%.
Regular screening has meant that pre cancerous changes and early stage cervical cancers have been detected and treated early. Figures suggest that cervical screening is saving 5,000 lives each year in the UK by preventing cervical cancer.[46]
About 1,000 women per year die of cervical cancer in the UK.
Epidemiology
Worldwide, cervical cancer is the fifth most deadly cancer in women.[47] It affects about 16 per 100,000 women per year and kills about 9 per 100,000 per year.[48]
In the United States, it is only the 8th most common cancer of women. In 1998, about 12,800 women were diagnosed in the US and about 4,800 died.[6] Among gynecological cancers it ranks behind endometrial cancer and ovarian cancer. The incidence and mortality in the US are about half those for the rest of the world, which is due in part to the success of screening with the Pap smear.[6]
In Great Britain, the incidence is 8.8/100,000 per year (2001), similar to the rest of Northern Europe, and mortality is 2.8/100,000 per year (2003) (Cancer Research UK Cervical cancer statistics for the UK). With a 42% reduction from 1988-1997 the NHS implemented screening programme has been highly successful, screening the highest risk age group (25-49 years) every 3 years, and those ages 50-64 every 5 years.
In Canada, an estimated 1,300 women will be diagnosed with cervical cancer in 2008 and 380 will die.[49]
Worldwide it is estimated that there are 473,000 cases of cervical cancer, and 253,500 deaths per year.[50]
History
- 400 BCE - Hippocrates: cervical cancer incurable
- 1925 - Hans Hinselmann: invented colposcope
- 1928 - Papanicolaou: developed Pap technique
- 1941 - Papanicolaou and Trout: Pap screening
- 1946 - Ayer: spatula to scrape the cervix
- 1976 - Zur Hausen and Gisam: found HPV DNA in cervical cancer and warts
- 1988 - Bethesda System for Pap results developed
Epidemiologists working in the early 20th century noted that:
- Cervical cancer was common in female sex workers.
- It was rare in nuns, except for those who had been sexually active before entering the convent. (Rigoni in 1841)
- It was more common in the second wives of men whose first wives had died from cervical cancer.
- It was rare in Jewish women.[51]
- In 1935, Syverton and Berry discovered a relationship between RPV (Rabbit Papillomavirus) and skin cancer in rabbits. (HPV is species specific and therefore cannot be transmitted to rabbits)
This led to the deduction that cervical cancer could be caused by a sexually transmitted agent. Initial research in the 1950s and 1960s put the blame on smegma (e.g. Heins et al 1958)[52] , but it wasn't until the 1970s that human papillomavirus (HPV) was identified. A description by electron microscopy was given earlier in 1949 and HPV-DNA was identified in 1963. It has since been demonstrated that HPV is implicated in virtually all cervical cancers.[4] Specific viral subtypes implicated are HPV 16, 18, 31, 45 and others.
References and Notes
- ↑ 1.0 1.1 1.2 1.3 1.4 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N.. Robbins Basic Pathology ((8th ed.) ed.). Saunders Elsevier. pp. 718-721. ISBN 978-1-4160-2973-1.
- ↑ Walboomers JM, Jacobs MV, Manos MM, et al (1999). "Human papillomavirus is a necessary cause of invasive cervical cancer worldwide". J. Pathol. 189 (1): 12–9. doi:. PMID 10451482.
- ↑ 3.0 3.1 "FDA Licenses New Vaccine for Prevention of Cervical Cancer", U.S. Food and Drug Administration (2006-06-08). Retrieved on 2007-12-02.
- ↑ 4.0 4.1 Lowy DR, Schiller JT (2006). "Prophylactic human papillomavirus vaccines.". J. Clin. Invest. 116 (5): 1167–73. doi:. PMID 16670757. http://www.jci.org/articles/view/JCI28607. Retrieved on 2007-12-01.
- ↑ "Human Papillomavirus (HPV) Vaccines: Q & A - National Cancer Institute". Retrieved on 2008-07-18.
- ↑ 6.0 6.1 6.2 6.3 Canavan TP, Doshi NR (2000). "Cervical cancer.". Am Fam Physician 61 (5): 1369–76. PMID 10735343. http://www.aafp.org/afp/20000301/1369.html. Retrieved on 2007-12-01.
- ↑ Nanda, Rita (2006-06-09). "Cervical cancer". MedlinePlus Medical Encyclopedia. National Institutes of Health. Retrieved on 2007-12-02.
- ↑ 8.0 8.1 "What Causes Cancer of the Cervix?". American Cancer Society (2006-11-30). Retrieved on 2007-12-02.
- ↑ Marrazzo JM, Koutsky LA, Kiviat NB, Kuypers JM, Stine K (2001). "Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women.". Am J Public Health 91 (6): 947–52. PMID 11392939. http://www.ajph.org/cgi/pmidlookup?view=long&pmid=11392939. Retrieved on 2007-12-30.
- ↑ "HPV Type-Detect". Medical Diagnostic Laboratories (2007-10-30). Retrieved on 2007-12-02.
- ↑ Gottlieb, Nicole (2002-04-24). "A Primer on HPV". Benchmarks. National Cancer Institute. Retrieved on 2007-12-02.
- ↑ Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ (2003). "Epidemiologic classification of human papillomavirus types associated with cervical cancer.". N. Engl. J. Med. 348 (6): 518–27. doi:. PMID 12571259. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=12571259&promo=ONFLNS19. Retrieved on 2007-12-01.
- ↑ 13.0 13.1 Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N (1999). "Human papillomavirus is a necessary cause of invasive cervical cancer worldwide.". J. Pathol. 189 (1): 12–9. doi:. PMID 10451482.
- ↑ Snijders PJ, Steenbergen RD, Heideman DA, Meijer CJ (2006). "HPV-mediated cervical carcinogenesis: concepts and clinical implications.". J. Pathol. 208 (2): 152–64. doi:. PMID 16362994.
- ↑ Nader, Carol (2005-02-16). "Expert says circumcision makes sex safer", The Age, Fairfax Media. Retrieved on 2007-12-02.
- ↑ Rivet C (2003). "Circumcision and cervical cancer. Is there a link?". Can Fam Physician 49: 1096–7. PMID 14526861. http://www.cfpc.ca/cfp/2003/sep/vol49-sep-critical-1.asp. Retrieved on 2007-12-01.
- ↑ Garcia, Agustin; Omid Hamid, Anthony El-Khoueiry (2006-07-06). "Cervical Cancer". eMedicine. WebMD. Retrieved on 2007-12-02.
- ↑ Dolinsky, Christopher (2006-07-17). "Cervical Cancer: The Basics", OncoLink, Abramson Cancer Center of the University of Pennsylvania. Retrieved on 2007-12-02.
- ↑ Erstad, Shannon (2007-01-12). "Cone biopsy (conization) for abnormal cervical cell changes", WebMD. Retrieved on 2007-12-02.
- ↑ Jones WB, Mercer GO, Lewis JL, Rubin SC, Hoskins WJ (1993). "Early invasive carcinoma of the cervix.". Gynecol. Oncol. 51 (1): 26–32. doi:. PMID 8244170. http://linkinghub.elsevier.com/retrieve/pii/S0090-8258(83)71241-2. Retrieved on 2007-12-01.
- ↑ Dolson, Laura (2001). "Trachelectomy". Retrieved on 2007-12-02.
- ↑ 22.0 22.1 Burnett AF (2006). "Radical trachelectomy with laparoscopic lymphadenectomy: review of oncologic and obstetrical outcomes.". Curr. Opin. Obstet. Gynecol. 18 (1): 8–13. doi:. PMID 16493253. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?an=00001703-200602000-00004. Retrieved on 2007-12-01.
- ↑ Cibula D, Ungár L, Svárovský J, Zivný J, Freitag P (2005). "[Abdominal radical trachelectomy--technique and experience]" (in Czech). Ceska Gynekol 70 (2): 117–22. PMID 15918265.
- ↑ Plante M, Renaud MC, Hoskins IA, Roy M (2005). "Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer. A series of 50 pregnancies and review of the literature.". Gynecol. Oncol. 98 (1): 3–10. doi:. PMID 15936061. http://linkinghub.elsevier.com/retrieve/pii/S0090-8258(05)00270-2. Retrieved on 2007-12-01.
- ↑ Roy M, Plante M, Renaud MC, Têtu B (1996). "Vaginal radical hysterectomy versus abdominal radical hysterectomy in the treatment of early-stage cervical cancer.". Gynecol. Oncol. 62 (3): 336–9. doi:. PMID 8812529. http://linkinghub.elsevier.com/retrieve/pii/S0090-8258(96)90245-0. Retrieved on 2007-12-01.
- ↑ Dargent D, Martin X, Sacchetoni A, Mathevet P (2000). "Laparoscopic vaginal radical trachelectomy: a treatment to preserve the fertility of cervical carcinoma patients.". Cancer 88 (8): 1877–82. doi:. PMID 10760765.
- ↑ Schlaerth JB, Spirtos NM, Schlaerth AC (2003). "Radical trachelectomy and pelvic lymphadenectomy with uterine preservation in the treatment of cervical cancer.". Am. J. Obstet. Gynecol. 188 (1): 29–34. doi:. PMID 12548192.
- ↑ "FDA Approves First Drug Treatment for Late-Stage Cervical Cancer", U.S. Food and Drug Administration (2006-06-15). Retrieved on 2007-12-02.
- ↑ Tiro JA, Meissner HI, Kobrin S, Chollette V (2007). "What do women in the U.S. know about human papillomavirus and cervical cancer?". Cancer Epidemiol. Biomarkers Prev. 16 (2): 288–94. doi:. PMID 17267388. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=17267388. Retrieved on 2007-12-01.
- ↑ 30.0 30.1 "What Are the Key Statistics About Cervical Cancer?". American Cancer Society (2008-03-26). Retrieved on 2008-08-19.
- ↑ Saslow D, Runowicz CD, Solomon D, et al (2002). "American Cancer Society guideline for the early detection of cervical neoplasia and cancer". CA: a cancer journal for clinicians 52 (6): 342–62. PMID 12469763.
- ↑ Payne N, Chilcott J, McGoogan E (2000). "Liquid-based cytology in cervical screening: a rapid and systematic review". Health technology assessment (Winchester, England) 4 (18): 1–73. PMID 10932023. http://www.hta.ac.uk/execsumm/summ418.htm.
- ↑ [1]
- ↑ Willis BH, Barton P, Pearmain P, Bryan S, Hyde C (March 2005). "Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK". Health technology assessment (Winchester, England) 9 (13): 1–207, iii. PMID 15774236. http://www.hta.ac.uk/execsumm/summ913.htm.
- ↑ Naucler P, Ryd W, Törnberg S, et al (2007). "Human papillomavirus and Papanicolaou tests to screen for cervical cancer". N. Engl. J. Med. 357 (16): 1589–97. doi:. PMID 17942872. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=17942872&promo=ONFLNS19.
- ↑ "EU approves cervical cancer jab", BBC (2006-09-22). Retrieved on 2007-12-02.
- ↑ "GSK's HPV Vaccine 100% Effective For Four Years, Data Show", Medical News Today, MediLexicon International Ltd (2006-02-27). Retrieved on 2007-12-02.
- ↑ "Cancer jab 'stops 75% of deaths'", BBC (2006-09-04). Retrieved on 2007-12-02.
- ↑ McNeil C (2006). "Who invented the VLP cervical cancer vaccines?". J. Natl. Cancer Inst. 98 (7): 433. doi:. PMID 16595773. http://jnci.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16595773. Retrieved on 2007-12-01.
- ↑ Cornelis J.A. Hogewoning, Maaike C.G. Bleeker, et al. (2003). "Condom use Promotes the Regression of Cervical Intraepithelial Neoplasia and Clearance of HPV: Randomized Clinical Trial". International Journal of Cancer 107: 811–816. doi:. PMID 14566832.
- ↑ "Semen 'may fuel cervical cancer'", BBC (2006-08-31). Retrieved on 2007-12-02.
- ↑ "Semen can worsen cervical cancer", Medical Research Council (UK). Retrieved on 2007-12-02.
- ↑ "Cervical Cancer". Cervical Cancer: Cancers of the Female Reproductive System: Merck Manual Home Edition. Merck Manual Home Edition. Retrieved on 2007-03-24.
- ↑ Committee on Practice Bulletins-Gynecology (2002). "ACOG practice bulletin. Diagnosis and treatment of cervical carcinomas, number 35, May 2002". Obstetrics and gynecology 99 (5 Pt 1): 855–67. PMID 11978302.
- ↑ "Cervical Cancer". Cervical Cancer: Pathology, Symptoms and Signs, Diagnosis, Prognosis and Treatment. Armenian Health Network, Health.am.
- ↑ "Cervical cancer statistics and prognosis". Cancer Research UK. Retrieved on 2007-03-24.
- ↑ World Health Organization (February 2006). "Fact sheet No. 297: Cancer". Retrieved on 2007-12-01.
- ↑ "GLOBOCAN 2002 database: summary table by cancer". Retrieved on 2008-10-26.
- ↑ Noni MacDonald, Matthew B. Stanbrook, and Paul C. Hébert (September 9, 2008). "Human papillomavirus vaccine risk and reality". CMAJ 179 (6). doi:. http://www.cmaj.ca/cgi/content/full/179/6/503. Retrieved on 2008-11-17.
- ↑ "NCCC National Cervical Cancer Coalition". Retrieved on 2008-07-01.
- ↑ Menczer J (2003). "The low incidence of cervical cancer in Jewish women: has the puzzle finally been solved?" (PDF). Isr. Med. Assoc. J. 5 (2): 120–3. PMID 12674663. http://www.ima.org.il/imaj/ar03feb-11.pdf. Retrieved on 2007-12-01.
- ↑ Heins Jr, HC; EJ Dennis, HR Pratt-Thomas (1958-10-01). "The possible role of smegma in carcinoma of the cervix.". American Journal of Obstetrics & Gynecology 76 (4): 726–33. PMID 13583012.
- Harper DM, Franco EL, Wheeler C, Ferris DG, Jenkins D, Schuind A, Zahaf T, Innis B, Naud P, De Carvalho NS, Roteli-Martins CM, Teixeira J, Blatter MM, Korn AP, Quint W, Dubin G (2004). "Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with human papillomavirus types 16 and 18 in young women: a randomised controlled trial.". Lancet 364 (9447): 1757–65. doi:. PMID 15541448. http://linkinghub.elsevier.com/retrieve/pii/S0140673604173984. Retrieved on 2007-12-01.
- Peto, J; C Gilham, O Fletcher, FE Matthews (2004-07-17). "The cervical cancer epidemic that screening has prevented in the UK.". Lancet 364 (9430): 249–56. doi:. PMID 15262102.
External links
- Cervical cancer at the Open Directory Project
- Cervical cancer at the Yahoo! Directory
|
||||||||||||||||||||||||||||||||||||