Blood sugar
Blood sugar is a term which in colloquial usage refers to the amount of glucose present in a mammal's blood. However, the term, if used in a physiological context, is a misnomer and misleading because other sugars besides glucose are always present. However, since these other sugars are largely inert, and only glucose serves as a controlling signal for metabolic regulation, the term has gained some currency and is used by medical persons and lay persons alike. Glucose, transported via the bloodstream from the intestines or liver to body cells, is the primary source of energy for the body's cells.
Blood sugar concentration, or glucose level, is tightly regulated in the human body. Normally, the blood glucose level is maintained at a reference range between about 4 and 6 mM (mmol/l). The normal blood glucose level is about 90mg/100ml, which works out to 5mM (mmol/l), since the molecular weight of glucose, C6H12O6, is about 180 g/mol daltons. The total amount of glucose in circulating blood is therefore about 3.3 to 7g (assuming an ordinary adult blood volume of 5 litres, plausible for an average adult male). Glucose levels rise after meals for an hour or two by a few grams and are usually lowest in the morning, before the first meal of the day.
Failure to maintain blood glucose in the normal range leads to conditions of persistently high (hyperglycemia) or low (hypoglycemia) blood sugar. Diabetes mellitus, characterized by persistent hyperglycemia from any of several causes, is the most prominent disease related to failure of blood sugar regulation.
Contents |
Normal values
Despite widely variable intervals between meals or the occasional consumption of meals with a substantial carbohydrate load, human blood glucose levels normally remain within a remarkably narrow range. In most humans this varies from about 80 mg/dl to perhaps 110 mg/dl (3.9 to 6.0 mmol/litre) except shortly after eating when the blood glucose level rises temporarily (up to maybe 140 mg/dl or a bit more in non-diabetics).
It is usually a surprise to realize how little glucose is actually maintained in the blood and body fluids. The control mechanism works on very small quantities. In a healthy adult male of 75 kg (165.35 lb) with a blood volume of 5 litres (1.32 gal), a blood glucose level of 100 mg/dl or 5.5 mmol/l corresponds to about 5 g (0.2 oz or 0.002 gal, 1/500 of the total) of glucose in the blood and approximately 45 g (1½ ounces) in the total body water (which obviously includes more than merely blood and will be usually about 60% of the total body weight in men). A more familiar comparison may help – 5 grams of glucose is about equivalent to a commercial sugar packet (as provided in many restaurants with coffee or tea).
Regulation
main article: blood sugar regulation
The homeostatic mechanism which keeps the blood value of glucose in a remarkably narrow range is composed of several interacting systems, of which hormone regulation is the most important.
There are two types of mutually antagonistic metabolic hormones affecting blood glucose levels:
- catabolic hormones (such as glucagon, growth hormone, catecholamines, thyroxine and somatostatin), which increase blood glucose
- and one anabolic hormone (insulin), which decreases blood glucose.
Glucose measurement
Sample type
Glucose can be measured in whole blood, serum, or plasma. Historically, blood glucose values were given in terms of whole blood, but most laboratories now measure and report the serum glucose levels. Because RBC (erythrocytes) have a higher concentration of protein (eg, hemoglobin) than serum, serum has a higher water content and consequently more dissolved glucose than does whole blood. To convert from whole-blood glucose, multiplication by 1.15 has been shown to generally give the serum/plasma level.
Collection of blood in clot tubes for serum chemistry analysis permits the metabolism of glucose in the sample by blood cells until separated by centrifugation. Red blood cells, for instance, do not require insulin to intake glucose from the blood. Higher than normal amounts of white or red blood cell counts can lead to excessive glycolysis in the sample with substantial reduction of glucose level if the sample is not processed quickly. Ambient temperature at which the blood sample is kept prior to centrifuging and separation of Plasma/Serum also affects glucose levels. At refrigerator temperatures, glucose remains relatively stable for several hours in a blood sample. At room temperature (25 °C), a loss of 1 to 2% of total glucose per hour should be expected in whole blood samples. Loss of glucose under these conditions can be prevented by using Fluoride tubes (ie, gray-top) since fluoride inhibits glycolysis. However, these should only be used when blood will be transported from one hospital laboratory to another for glucose measurement. Red-top serum separator tubes also preserve glucose in samples after being centrifuged isolating the serum from cells.
Particular care should be given to drawing blood samples from the arm opposite the one in which an intravenous line is inserted, to prevent contamination of the sample with intravenous fluids. Alternatively, blood can be drawn from the same arm with an IV line after the IV has been turned off for at least 5 minutes, and the arm elevated to drain infused fluids away from the vein. Inattention can lead to large errors, since as little as 10% contamination with 5% dextrose (D5W) will elevate glucose in a sample by 500 mg/dl or more. Remember that the actual concentration of glucose in blood is very low, even in the hyperglycemic.
Arterial, capillary and venous blood have comparable glucose levels in a fasting individual. After meals venous levels are somewhat lower than capillary or arterial blood; a common estimate is about 10%.
Measurement techniques
Two major methods that have been used to measure glucose. The first, still in use in some places, is a chemical method exploiting the nonspecific reducing property of glucose in a reaction with an indicator substance that changes color when reduced. Since other blood compounds also have reducing properties (e.g., urea, which can be abnormally high in uremic patients), this technique can produce erroneous readings in some situations (5 to 15 mg/dl has been reported). The more recent technique, using enzymes specific to glucose, are less susceptible to this kind of error. The two most common employed enzymes are glucose oxidase and hexokinase.
In either case, the chemical system is commonly contained on a test strip, to which a blood sample is applied, and which is then inserted into the meter for reading. Test strip shapes and their exact chemical composition vary between meter systems and cannot be interchanged. Formerly, some test strips were read (after timing and wiping away the blood sample) by visual comparison against a color chart printed on the vial label. Strips of this type are still used for urine glucose readings, but for blood glucose levels they are obsolete. Their error rates were, in any case, much higher.
Urine glucose readings, however taken, are much less useful. In properly functioning kidneys, glucose does not appear in urine until the renal threshold for glucose has been exceeded. This is substantially above any normal glucose level, and so is evidence of an existing severe hyperglycemic condition. However, urine is stored in the bladder and so any glucose in it might have been produced at any time since the last time the bladder was emptied. Since metabolic conditions change rapidly, as a result of any of several factors, this is delayed news and gives no warning of a developing condition. Blood glucose monitoring is far preferable, both clinically and for home monitoring by patients.
| I. CHEMICAL METHODS | ||
| A. Oxidation-Reduction Reaction | ||
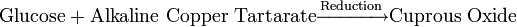 |
||
| 1. Alkaline Copper Reduction | ||
| Folin Wu Method | 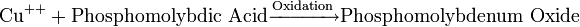 |
Blue end-product |
| Benedict's method |
|
|
| Nelson Somoygi Method | 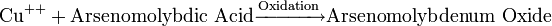 |
Blue end-product |
| Neocuproine Method |  * * |
Yellow-orange color Neocuproine |
| Shaeffer Hartmann Somygi |
|
|
| 2. Alkaline Ferricyanide Reduction | ||
| Hagedorn Jensen | 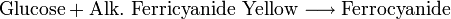 |
Colorless end product; other reducing substances interfere with reaction |
| B. Condensation | ||
| Ortho-toluidine Method |
|
|
| Anthrone (Phenols) Method |
|
|
| II. ENZYMATIC METHODS | ||
| A. Glucose Oxidase | ||
![\mathrm{Glucose} + \mathrm{O}^{2}\xrightarrow[\mathrm{Oxidation}] {\mathrm{glucose\ oxidase}}\mathrm{Cuprous\ Oxide}](/2009-wikipedia_en_wp1-0.7_2009-05/I/ee4b420e1c8f2445a89e73f63727897d.png) |
||
| Saifer Gernstenfield Method | ![\mathrm{H_{2}O_2} + \textrm{\textit{O}-dianisidine}\xrightarrow[\mathrm{Oxidation}] {\mathrm{peroxidase}} \mathrm{H_2O} + \mathrm{oxidized\ chromogen}](/2009-wikipedia_en_wp1-0.7_2009-05/I/e563e5405afc63ea175af0bdcdce58e3.png) |
Inhibited by reducing substances like BUA, Bilirubin, Glutathione, Ascorbic Acid |
| Trinder Method |
|
|
| Kodak Ektachem |
|
|
| Glucometer |
|
|
| B. Hexokinase | ||
|
|
||
|
||
Blood glucose laboratory tests
- fasting blood sugar (ie, glucose) test (FBS)
- urine glucose test
- two-hr postprandial blood sugar test (2-h PPBS)
- oral glucose tolerance test (OGTT)
- intravenous glucose tolerance test (IVGTT)
- glycosylated hemoglobin (HbA1C)
- self-monitoring of glucose level via patient testing
Clinical correlation
The fasting blood glucose (FBG) level is the most commonly used indication of overall glucose homeostasis, largely because disturbing events such as food intake are avoided. Conditions affecting glucose levels are shown in the table below. Abnormalities in these test results are due to problems in the multiple control mechanism of glucose regulation.
The metabolic response to a carbohydrate challenge is conveniently assessed by a postprandial glucose level drawn 2 hours after a meal or a glucose load. In addition, the glucose tolerance test, consisting of several timed measurements after a standardized amount of oral glucose intake, is used to aid in the diagnosis of diabetes. It is regarded as the gold standard of clinical tests of the insulin / glucose control system, but is difficult to administer, requiring much time and repeated blood tests. Note that food commonly includes carbohydrates which don't participate in the metabolic control system; simple sugars such as fructose, many of the disaccarhides (which either contain simple sugars other than glucose or cannot be digested by humans) and the more complex sugars which also cannot be digested by humans. And there are carbohydrates which are not digested even with the assistance of gut bacteria; several of the fibres (soluble or insoluble) are chemically carbohydrates. Food also commonly contains components which affect glucose (and other sugar's) digestion; fat, for example slows down digestive processing, even for such easily handled food constituents as starch. Avoiding the effects of food on blood glucose measurement is important for reliable results since those effects are so variable.
Error rates for blood glucose measurements systems vary, depending on laboratories, and on the methods used. Colorimetry techniques can be biased by color changes in test strips (from airborne or finger borne contamination, perhaps) or interference (eg, tinting contaminants) with light source or the light sensor. Electrical techniques are less susceptible to these errors, though not to others. In home use, the most important issue is not precision, but trend. Thus if your meter / test strip system is consistently wrong by 10%, there will be little consequence, as long as changes (eg, due to exercise or medication adjustments) are properly tracked. In the US, home use blood test meters must be approved by the Federal Food and Drug Administration before they can be sold. Similar supervision is imposed in other jurisdictions.
Finally, there are several influences on blood glucose level aside from food intake. Infection, for instance, tends to change blood glucose levels, as does stress either physical or psychological. Exercise, especially if prolonged or long after the most recent meal, will have an effect as well. In the normal person, maintenance of blood glucose at near constant levels will nevertheless be quite effective.
| Persistent Hyperglycemia | Transient Hyperglycemia | Persistent Hypoglycemia | Transient Hypoglycemia |
|---|---|---|---|
| Reference Range, FBG: 70-110 mg/dl | |||
| Diabetes Mellitus | Pheochromocytoma | Insulinoma | Acute Alcohol Ingestion |
| Adrenal cortical hyperactivity Cushing's Syndrome | Severe Liver Disease | Adrenal cortical insufficiency Addison's Disease | Drugs: salicylates, antituberculosis agents |
| Hyperthyroidism | Acute stress reaction | Hypopituitarism | Severe Liver disease |
| Acromegaly | Shock | Galactosemia | Several Glycogen storage diseases |
| Obesity | Convulsions | Ectopic Insulin production from tumors | Hereditary fructose intolerance |
Health effects
If blood sugar levels drop too low, a potentially fatal condition called hypoglycemia develops. Symptoms may include lethargy, impaired mental functioning, irritability, and loss of consciousness. Brain damage is even possible.
If levels remain too high, appetite is suppressed over the short term. Long-term hyperglycemia causes many of the long-term health problems associated with diabetes, including eye, kidney, and nerve damage.
Low blood sugar
Some people report drowsiness or impaired cognitive function several hours after meals, which they believe is related to a drop in blood sugar, or "low blood sugar". For more information, see:
- idiopathic postprandial syndrome
- hypoglycemia
Mechanisms which restore satisfactory blood glucose levels after hypoglycemia must be quick and effective, because of the immediately serious consequences of insufficient glucose; in the extreme, coma, but also less immediately dangerous, confusion or unsteadiness, amongst many other symptoms. This is because, at least in the short term, it is far more dangerous to have too little glucose in the blood than too much. In healthy individuals these mechanisms are generally quite effective, and symptomatic hypoglycemia is generally only found in diabetics using insulin or other pharmacological treatment. Such hypoglycemic episodes vary greatly between persons and from time to time, both in severity and swiftness of onset. For severe cases, prompt medical assistance is essential, as damage (to brain and other tissues) and even death will result from sufficiently low blood glucose levels.
Converting glucose units
In most countries, blood glucose is reported in terms of molarity, measured in mmol/L (or millimolar, abbreviated mM). In the United States, and to a lesser extent elsewhere, mass concentration, measured in mg/dL, is typically used.
To convert blood glucose readings between the two units:
- Divide a mg/dL figure by 18 (or multiply by 0.055) to get mmol/L.
- Multiply a mmol/L figure by 18 (or divide by 0.055) to get mg/dL.
Comparative content

References
- John Bernard Henry, M.D.: Clinical diagnosis and Management by Laboratory Methods 20th edition, Saunders, Philadelphia, PA, 2001.
- Ronald A. Sacher and Richard A. McPherson: Widmann's Clinical Interpretation of Laboratory Tests 11th edition, F.A. Davis Company, 2001.
See also
- Current research - Boronic acids in supramolecular chemistry: Saccharide recognition
- Blood glucose monitoring
|
||||||||

![\begin{alignat}{2}
& \mathrm{Glucose} + \mathrm{ATP}\xrightarrow[\mathrm{Phosphorylation}] {\mathrm{Hexokinase} + \mathrm{Mg}^{++}} \textrm{G-6PO}_4 + \mathrm{ADP} \\
& \textrm{G-6PO}_4 + \mathrm{NADP}\xrightarrow[\mathrm{Oxidation}] {\textrm{G-6PD}} \textrm{G-Phosphogluconate} + \mathrm{NADPH} + \mathrm{H}^{+} \\
\end{alignat}](/2009-wikipedia_en_wp1-0.7_2009-05/I/55e5b2ebdbaddaf4c69d398449ddf479.png)