Benzodiazepine
| Benzodiazepine | |
|---|---|
 |
|
| IUPAC name | 5-phenyl-1,3-dihydro-2H-1,4-benzodiazepin-2-one |
| Other names | 5-phenyl-1H-benzo[e][1,4]diazepin-2(3H)-one |
| Identifiers | |
| CAS number | |
| PubChem | |
| SMILES |
|
| InChI |
|
| Properties | |
| Molecular formula | C15H12N2O |
| Molar mass | 236.269 g·mol−1 |
| Except where noted otherwise, data are given for materials in their standard state (at 25 °C, 100 kPa) Infobox references |
|
The benzodiazepines (pronounced /ˌbɛnzəʊdaɪˈæzəˌpiːn/, often abbreviated to "benzos") are a class of psychoactive drugs with varying hypnotic, sedative, anxiolytic, anticonvulsant, muscle relaxant and amnesic properties, which are mediated by slowing down the central nervous system.[1] Benzodiazepines are useful in treating anxiety, insomnia, agitation, seizures, and muscle spasms, as well as alcohol withdrawal. They can also be used before certain medical procedures such as endoscopies or dental work where tension and anxiety are present, and prior to some unpleasant medical procedures in order to induce sedation and amnesia[2] for the procedure. Another use is to counteract anxiety-related symptoms upon initial use of SSRIs and other antidepressants, or as an adjunctive treatment. Recreational stimulant users often use benzodiazepines as a means of "coming down". Benzodiazepines are also used to treat the panic that can be caused by hallucinogen intoxication.[3]
The long-term use of benzodiazapines can cause physical dependence. The use of benzodiazepines should therefore commence only after medical consultation and benzodiazepines should be prescribed the smallest dosage possible to provide an acceptable level of symptom relief. Dependence varies with the benzodiazepine used and with the user.
Contents |
History

The first benzodiazepine, chlordiazepoxide (Librium) was discovered serendipitously in 1954 by the Austrian scientist Leo Sternbach (1908–2005), working for the pharmaceutical company Hoffmann–La Roche. Chlordiazepoxide was synthesised from work on a chemical dye, quinazolone-3-oxides. Initially, he discontinued his work on the compound Ro-5-0690, but he "rediscovered" it in 1957 when an assistant was cleaning up the laboratory. Although initially discouraged by his employer, Sternbach conducted further research that revealed the compound was a very effective tranquilizer. Tests revealed that the compound had hypnotic, anxiolytic and muscle relaxant effects. Three years later chlordiazepoxide was marketed as a therapeutic benzodiazepine medication under the brand name Librium. Following chlordiazepoxide in 1963 diazepam hit the market under the brand name Valium, followed by many further benzodiazepine compounds which were introduced over the subsequent years and decades.[4]
The original chemical name of chlordiazepoxide was methaminodiazepoxide but it was changed to chlordiazepoxide. It was marketed under the trade name Librium, derived from the final syllables of equilibrium. In 1959 it was used by over 2,000 physicians and more than 20,000 patients. It was described as "chemically and clinically different from any of the tranquilizers, psychic energizers or other psychotherapeutic drugs now available." During studies, chlordiazepoxide induced muscle relaxation and a quieting effect on laboratory animals like mice, rats, cats, and dogs. Fear and aggression were eliminated in much smaller doses than those necessary to produce hypnosis. Chlordiazepoxide is similar to phenobarbital in its anticonvulsant properties. However, it lacks the hypnotic effects of barbiturates. Animal tests were conducted in the Boston Zoo and the San Diego Zoo. Forty-two hospital patients admitted for acute and chronic alcoholism, and various psychoses and neuroses were treated with chlordiazepoxide. In a majority of the patients, anxiety, tension, and motor excitement were "effectively reduced." The most positive results were observed among alcoholic patients. It was reported that ulcers and dermatologic problems, both of which involve emotional factors, were reduced by chlordiazepoxide.[5]
Chlordiazepoxide enabled the treatment of emotional disturbances without a loss of mental acuity or alertness. It assisted persons burdened by compulsive reactions like one that felt compelled to count the slats on venetian blinds upon entering a room.[6]
Dr. Carl F. Essig of the Addiction Research Center of the National Institute of Mental Health spoke at a symposium on drug abuse at an annual meeting of the American Association for the Advancement of Science, in December 1963. He named meprobamate, glutethimide, ethinamate, ethchlorvynol, methyprylon, and chlordiazepoxide as drugs whose usefulness can hardly be questioned. However, Essig labeled these newer products as drugs of addiction, like barbiturates, whose habit-forming qualities were more widely-known. He mentioned a 90-day study of chlordiazepoxide, which concluded that the automobile accident rate among 68 users was ten times higher than normal. Participants' daily dosage ranged from 5 to 100 milligrams.[7]
In 1963, approval for use was given to diazepam (Valium), a "simplified" version of chlordiazepoxide, primarily to counteract anxiety symptoms. Sleep-related problems were treated with nitrazepam (Mogadon), which was introduced in 1965, temazepam (Restoril), which was introduced in 1969, and flurazepam (Dalmane), which was introduced in 1973.[8]
A related class of drugs that also work on the benzodiazepine receptors, the nonbenzodiazepines, has recently been introduced.[9] Nonbenzodiazepines are molecularly distinct from benzodiazepines and have less addictive potential, while still offering benefits very similar to those of benzodiazepines.
Pharmacology
Duration of action
Benzodiazepines are commonly divided into three groups by their half-lives: Short-acting compounds have a half-life of less than 12 hours, and have few residual effects if taken before bedtime, but rebound insomnia may occur and they might cause wake-time anxiety. Intermediate-acting compounds have a half-life of 12–24 hours, may have residual effects in the first half of the day. Rebound insomnia however is more common upon discontinuation of short-acting benzodiazepines. Daytime withdrawal symptoms are also a problem with prolonged usage of short-acting benzodiazepines, including daytime anxiety. Long-acting compounds have a half-life greater than 24 hours.[10][11] Strong sedative effects typically persist throughout the next day if long-acting preparations are used for insomnia. Accumulation of the compounds in the body may occur. The elimination half-life may greatly vary between individuals, especially the elderly. Shorter-acting compounds are usually best for their hypnotic effects, whereas longer-acting compounds are usually better for their anxiolytic effects. Benzodiazepines with shorter half-lives tend to be able to produce tolerance and addiction quicker, as the drug does not last in the system for as long, with resultant interdose withdrawal phenomenon and next-dose craving. Although short-acting drugs are more commonly prescribed for insomnia, there are exceptions to the rules, such as alprazolam being prescribed as an anxiolytic more than a hypnotic, despite possessing a short half-life.
Mechanism of action
Benzodiazepines produce a range of effects from depressing to stimulating the central nervous system via modulating the GABAA receptor, the most prevalent inhibitory receptor within the brain. The subset of GABAA receptors that also bind benzodiazepines are referred to as benzodiazepine receptors (BzR). The GABAA receptor is composed of five subunits, most commonly two α's, two β's, and one γ (α2β2γ). For each subunit, multiple subtypes exist (α1-6, β1-3, and γ1-3). GABAA receptors that are made up of different combinations of subunit subtypes have different properties, different distributions within the brain, and different activities relative to pharmacological and clinical effects.
Benzodiazepines bind at the interface of the α and γ subunits on the GABAA receptor. Benzodiazepine binding also requires that alpha subunits contain a histidine amino acid residue, (i.e., α1, α2, α3 and α5 containing GABAA receptors). For this reason, benzodiazepines show no affinity for GABAA receptors containing α4 and α6 subunits, which contain an arginine instead of a histidine residue. Other sites on the GABAA receptor also bind neurosteroids, barbiturates and certain anesthetics.[12]
Once bound to the BzR, the benzodiazepine ligand locks the BzR into a conformation in which it has a much higher affinity for the GABA neurotransmitter than otherwise. This increases the frequency of opening of the associated chloride ion channel and hyperpolarizes the membrane of the associated neuron. This potentiates the inhibitory effect of the available GABA, leading to sedatory and anxiolytic effects. As mentioned above, different benzodiazepines can have different affinities for BzRs made up of different collection of subunits. For instance, benzodiazepines with high activity at the α1 are associated with sedation, whereas those with higher affinity for GABAA receptors containing α2 and/or α3 subunits have good anti-anxiety activity.[13] Benzodiazepines also bind to glial cell membranes.[14]
Some benzodiazepines are full BzR agonists, producing anxiolytic and sedating properties. Compounds that, in the absence of agonist, have no apparent activity but that competitively inhibit the binding of agonists to the receptor are called BzR antagonists. Ligands that decrease GABA function are termed benzodiazepine receptor inverse agonists. Full inverse agonists have potent convulsant activities.
Some compounds lie somewhere between being full agonists and neutral antagonists, and are termed either partial agonists or partial antagonists. There has been interest in partial agonists for the BzR, with evidence that complete tolerance may not occur with chronic use, with partial agonists demonstrating continued anxiolytic properties with reduced sedation, dependence, and withdrawal problems.[15]
However the anticonvulsant properties of benzodiazepines may be in part or entirely due to binding to voltage-dependent sodium channels rather than benzodiazepine receptors. Sustained repetitive firing seems to be limited by benzodiazepines effect of slowing recovery of sodium channels from inactivation.[16]
Benzodiazepine receptors also appear in a number of non nervous-system tissues and are mainly of the peripheral benzodiazepine receptor (PBRs) type. These peripheral benzodiazepine receptors are not coupled (or "attached") to GABAA receptors. These are found in various tissues such as heart, liver, adrenal, and testis, as well as hemopoietic and lymphatic cells.[17] In lymphatic tissues, they modulate apoptosis of thymocytes via reduction of mitochondrial transmembrane potential.[18] PBRs have many other actions on immune cells including modulation of oxidative bursts by neutrophils and macrophages, and inhibition of macrophage secretion of cytokines inhibition of the proliferation of lymphoid cells and secretion of cytokines by macrophages.[19]
Benzodiazepines and their therapeutic uses
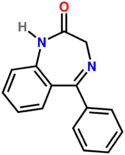
The core chemical structure of "classical" benzodiazepine drugs is a fusion between the benzene and diazepine ring systems. Many of these drugs contain the 5-phenyl-1,3-dihydro-1,4-benzodiazepin-2-one substructure (see figure to the above right). Benzodiazepines are molecularly similar to several groups of drugs, some of which share similar pharmacological properties, including the quinazolinones, hydantoines, succinimides, oxazolidinediones, barbiturates and glutarimides.[20][21] Most benzodiazepines are administered orally; however, administration can also occur intravenously, intramuscularly, sublingually or as a suppository. Benzodiazepines have a number of therapeutic uses, are well-tolerated, and are very safe and effective drugs in the short term for a wide range of conditions.
Anticonvulsants
- clobazam
- clonazepam
- clorazepate
- diazepam
- lorazepam
- midazolam
Benzodiazepines are potent anticonvulsants and have life-saving properties in the acute management of status epilepticus. The most commonly-used benzodiazepines for seizure control are lorazepam and diazepam. A meta-analysis of 11 clinical trials concluded that lorazepam was superior to diazepam in treating persistent seizures.[22] Although diazepam is much longer-acting than lorazepam, lorazepam has a more prolonged anticonvulsant effect. This is because diazepam is very lipid-soluble and highly protein-bound, and has a very large distribution of unbound drug, resulting in diazepam's having only a 20– to 30-minute duration of action against status epilepticus. Lorazepam, however, has a much smaller volume of distribution of unbound drug, which results in a more prolonged duration of action against status epilepticus. Lorazepam can therefore be considered superior to diazepam, at least in the initial stages of treatment of status epilepticus.[23]
Anxiolytics
- alprazolam
- bromazepam
- chlordiazepoxide
- clonazepam
- clorazepate
- diazepam
- lorazepam
- medazepam
- nordazepam
- oxazepam
- prazepam
Benzodiazepines possess anti-anxiety properties and can be useful for the short-term treatment of severe anxiety. Benzodiazepines are usually administered orally for the treatment of anxiety; however, occasionally lorazepam or diazepam may be given intravenously for the treatment of panic attacks.[24]
A panel of over 50 peer-nominated internationally recognized experts in the pharmacotherapy of anxiety and depression judged the benzodiazepines, especially combined with an antidepressant, as the mainstays of pharmacotherapy for anxiety disorders.[25][26][27][28]
Despite increasing focus on the use of antidepressants and other agents for the treatment of anxiety, benzodiazepines have remained a mainstay of anxiolytic pharmacotherapy due to their robust efficacy, rapid onset of therapeutic effect, and generally favorable side effect profile.[29] Treatment patterns for psychotropic drugs appear to have remained stable over the past decade, with benzodiazepines being the most commonly used medication for panic disorder.[30]
Insomnia
- brotizolam
- estazolam
- flunitrazepam
- flurazepam
- loprazolam
- lormetazepam
- midazolam
- nimetazepam
- nitrazepam
- temazepam
- triazolam
Hypnotic benzodiazepines have strong sedative effects, and certain benzodiazepines therefore are often prescribed for the management of insomnia. Longer-acting benzodiazepines, such as nitrazepam, have side-effects that may persist into the next day, whereas the more intermediate-acting benzodiazepines (for example, temazepam) may have less "hangover" effects the next day.[31] Benzodiazepine hypnotics should be reserved for short-term courses to treat acute conditions, as tolerance and dependence may occur if these benzodiazepines are taken regularly for more than a few weeks.
Premedication before procedures
Benzodiazepines can be very beneficial as premedication before surgery, especially in those that are anxious. Usually administered a couple of hours before surgery, benzodiazepines will bring about anxiety relief and also produce amnesia. Amnesia can be useful in this situation, as patients will not be able to remember any unpleasantness from surgery.[32] Diazepam or temazepam can be utilized in patients who are particularly anxious about dental procedures.[32] Alternatively nitrous oxide can be administered in dental phobia due to its sedative and dissociative effects, its fast onset of action, and its extremely short duration of action.
Intensive care
Benzodiazepines can be very useful in intensive care to sedate patients receiving mechanical ventilation, or those in extreme distress or severe pain. Caution should be exercised in this situation due to the occasional scenario of respiratory depression, and benzodiazepine overdose treatment facilities should be available.[32]
The following are some of the criteria for Intensive care unit monitoring[33]
- Age greater than 40 with concomitant medical illness e.g. cardiac disease with failure, ischemia or angina, recent infarction
- Severe electrolyte imbalances especially with ECG changes, severe acid base disturbances
- Hemodynamic instability
- Respiratory insufficiency, hypoxemia and/or hypercapnia
- Potentially serious infections, including sepsis
- GI pathology including pancreatitis, GI bleeding, fulminant hepatic failure, peritonitis
- Persistent hyperthermia (Tmax > 39°C or 103°F)
- Rhabdomyolysis
- Renal failure
- Prior history of severe Delirium Tremens
- Need for IV benzodiazepines or other IV drips to control withdrawal
Alcohol dependence
Benzodiazepines have been shown to be safe and effective, particularly for preventing or treating seizures and delirium, and are the preferred agents for treating the symptoms of alcohol withdrawal syndrome.[34] The choice of agent is based on pharmacokinetics. The most commonly used benzodiazepines in the management of alcohol withdrawal are diazepam (Valium) and chlordiazepoxide (Librium), two long-acting agents, and lorazepam (Ativan) and oxazepam (Serax), two intermediate-acting agents. The long half-life of diazepam and chlordiazepoxide make withdrawal smoother, and rebound withdrawal symptoms are less likely to occur. The two intermediate-acting agents have excellent records of efficacy. Chlordiazepoxide is the benzodiazepine of choice in uncomplicated alcohol withdrawal.[35] Oxazepam is the most commonly used benzodiazepine in managing alcohol withdrawal symptoms. It is the benzodiazepine of choice in treating severe alcohol withdrawal symptoms, and it is often used in patients that metabolize medications less effectively, particularly the elderly and those with cirrhosis. Lorazepam is the only benzodiazepine with predictable intramuscular absorption (if intramuscular administration is necessary) and it is the most effective in preventing and controlling seizures. Phenazepam is another benzodiazepine that has been used to treat alcohol withdrawal with excellent efficacy. In Russia, it is preferred over diazepam in the management of alcohol withdrawal.
Muscular disorders
Benzodiazepines are well known for their strong muscle-relaxing properties, and can be useful in the treatment of muscle spasms, for example, Tetanus or spastic disorders[36] and Restless legs syndrome. Clonazepam has been used with efficacy in the treatment of some forms of Tourette's syndrome (with symptoms more on the side of motor tics, as opposed to vocal tics, although almost any tic can be preceded by, and intensify with stress; therapy for Tourette's syndrome is highly individualized.) Many people experiencing tremors may be helped with benzodiazepines.
Acute mania
Mania, a mood disorder, is a state of extreme mood elevation and is a diagnosable serious psychiatric disorder. Benzodiazepines can be very useful in the short-term treatment of acute mania, until the effects of lithium or neuroleptics take effect. Benzodiazepines bring about rapid tranquillisation and sedation of the manic individual, therefore benzodiazepines are a very important tool in the management of mania. Both clonazepam and lorazepam are used for the treatment, with some evidence that clonazepam may be superior in the treatment of acute mania.[37][38]
Veterinary practice
As in humans, benzodiazepines have a wide range of uses in veterinary practice in the treatment of various disorders and scenarios involving animals.
Midazolam and diazepam are utilized for their anesthetic properties in veterinary practice in combination with other general anesthetic drugs such as ketamine.[39][40]
Midazolam or diazepam can also be used as a sedative anxiolytic to quell anxiety and agitation experienced by animals in veterinary practice, for example, during transport. [41][42] Diazepam has also been found to have tranquillising effects on various animals tested with the following properties; myorelaxation, stress reduction and aggression inhibition.[43]
Benzodiazepines are also commonly used for the control of muscular conditions in animals. Diazepam has been prescribed for the effective treatment and control of tremors by veterinarians in animals. Corticosteroids and or Diazepam have been found to be effective for the control of tremors in veterinarian practice.[44][45] Diazepam has also been used in to control muscle spasms that were the result of tetanus in cats.[46]
Benzodiazepines, such as diazepam, are used in the treatment of various forms of epilepsy in dogs.[47] Benzodiazepines have potent anticonvulsant properties and are very effective in the short term in managing seizure disorders in animals. However, with prolonged usage, benzodiazepines tend to lose their anticonvulsant properties. Partial benzodiazepine receptor agonists have shown some promise, with continued efficacy being demonstrated with benzodiazepine receptor partial agonists and also displaying mild withdrawal symptoms upon discontinuation, which may make them superior to benzodiazepines in the long-term management of epilepsy in animals.[48] Phenobarbital is the drug of choice and potassium bromide is the drug of second choice in the treatment of epilepsy in dogs and diazepam is recommended for the treatment at home of cluster seizures.[49]
Lorazepam has been found to be an effective premedication before general anesthesia in bringing about adequate muscular relaxation for veterinary surgery.[50]
Midazolam can also be used along with other drugs in the sedation and capture of wild animals.[51]
Side-effects
The following list summarizes the side effects which may occur from use of benzodiazepines.[52]
- Drowsiness
- Dizziness
- Upset stomach
- Blurred vision
- Headache
- Confusion
- Depression
- Impaired coordination
- Changes in heart rate
- Trembling
- Weakness
- Amnesia
- Hangover effect (grogginess)
- Dreaming or nightmares
- Chest pain
- Vision changes
- Jaundice
- Paradoxical reactions[53]
Paradoxical reactions
Severe behavioral changes resulting from benzodiazepines have been reported including mania, schizophrenia, anger, impulsivity, and hypomania.[54] Individuals with borderline personality disorder appear to have a greater risk of experiencing severe behavioral or psychiatric disturbances from benzodiazepines. Aggression and violent outbursts can also occur with benzodiazepines, particularly when they are combined with alcohol. Recreational abusers and patients on high-dosage regimes may be at an even greater risk of experiencing paradoxical reactions to benzodiazepines.[55] Paradoxical reactions may occur in any individual on commencement of therapy and initial monitoring should take into account the risk of increase in anxiety or suicidal thoughts.[53]
When benzodiazepines are used as an adjunct in the treatment of seizures, an increase in dosage of the primary agent may be required. The concomitant administration of benzodiazepines and anti-convulsants may precipitate an increase in certain seizure activity, specifically tonic-clonic seizures.
In a letter to the British Medical Journal, it was reported that a high proportion of parents referred for actual or threatened child abuse were taking drugs at the time, often a combination of benzodiazepines and tricyclic antidepressants. Many mothers described that instead of feeling less anxious or depressed, they became more hostile and openly aggressive towards the child as well as to other family members while consuming tranquilizers. The author warned that environmental or social stresses such as difficulty coping with a crying baby combined with the effects of tranquilizers may precipitate a child abuse event.[56]
Paradoxical rage reactions from benzodiazepines are thought to be due to partial deterioration from consciousness, generating automatic behaviors, fixation amnesia, and aggressiveness from disinhibition with a possible serotonergic mechanism playing a role.[57]
Physical dependence and withdrawal
Long-term benzodiazepine usage, in general, leads to some form of tolerance and/or drug dependence with the appearance of a benzodiazepine withdrawal syndrome when the benzodiazepines are stopped or the dose is reduced. However, it is important to distinguish between addiction to and normal physical dependence on benzodiazepines. Benzodiazepines are usually a secondary drug of abuse—used mainly to augment the high received from another drug or to offset the adverse effects of other drugs.[58]
Withdrawal management
Benzodiazepine withdrawal symptoms occur when benzodiazepine dosage is reduced in people who are physically dependent on benzodiazepines. Abrupt or over-rapid dosage reduction can produce severe withdrawal symptoms. Withdrawal symptoms can even occur during a very gradual and slow dosage reduction.
Benzodiazepine withdrawal is best managed by transferring the physically-dependent patient to an equivalent dose of diazepam because it has the longest half-life of all of the benzodiazepines and is available in low-potency, 2-mg tablets, which can be quartered for small dose reductions.[59] The speed of benzodiazepine reduction regimes varies from person to person, but is usually 10% every 2–4 weeks. A slow withdrawal, preferably under medical supervision by a physician that is knowledgeable about the benzodiazepine withdrawal syndrome, with the patient in control of dosage reductions coupled with reassurance that withdrawal symptoms are temporary, have been found to produce the highest success rates. The withdrawal syndrome can usually be avoided or minimized by use of a long half-life benzodiazepine such as diazepam (Valium) or chlordiazepoxide (Librium) and a very gradually tapering off the drug over a period of months, or even up to a year or more, depending on the dosage and degree of dependency of the individual. A slower withdrawal rate significantly reduces the symptoms. In fact, some people feel better and more clear-headed as the dose gradually gets lower, so withdrawal from benzodiazepines is not necessarily an unpleasant event. People that report severe experiences from benzodiazepine withdrawal have almost invariably withdrawn or been withdrawn too quickly.[60]
Benzodiazepine drug misuse
Benzodiazepines are used/abused recreationally and activate the dopaminergic reward pathways in the central nervous system.[61] Misusers of benzodiazepines develop a high degree of tolerance, coupled with dosage escalation, often increasing their dosage to very high levels. Long-term use of benzodiazepines has the potential to cause both physical and psychological dependence, and are at risk of severe withdrawal symptoms. Tolerance and dependence to benzodiazepines develop rapidly with users of benzodiazepines, demonstrating benzodiazepine withdrawal syndrome after as little as 3 weeks of continuous use. Benzodiazepines, and in particular temazepam, are sometimes used intravenously, which done incorrectly or done in an unsterile matter can lead to medical complications including abscesses, cellulitis, thrombophlebitis, arterial puncture, deep vein thrombosis, hepatitis B and C, HIV or AIDS, overdose and gangrene.
Benzodiazepine use is widespread among amphetamine users, and those that have used amphetamines and benzodiazepines have greater levels of mental health problems, social deterioration, and poorer general health. Benzodiazepine injectors are almost four times more likely to inject using a shared needle than non-benzodiazepine-using injectors. It has been concluded in various studies that benzodiazepine use causes greater levels of risk and psycho-social dysfunction among drug users.[62] Those who use stimulants and depressant drugs are more likely to report adverse reactions from stimulant use, more likely to be injecting stimulants, and more likely to have been treated for a drug problem than those using stimulants but not depressant drugs.[63]
Once benzodiazepine dependence has been established a clinician should first establish the average daily consumption of benzodiazepines and then convert the patient to an equivalent dose of diazepam before beginning a gradual reduction program, starting initially with 2mg-size reductions. Additional drugs, such as antianxiety drugs like buspirone or β blockers, and carbamazepine, should not be added into the withdrawal program unless there is a specific indication for their use.[64]
A six-year study on 51 Vietnam veterans who were drug abusers of either mainly stimulants (11 people), mainly opiates (26 people), or mainly benzodiazepines (14 people) was carried out to assess psychiatric symptoms related to the specific drugs of abuse. After six years, opiate abusers had little change in psychiatric symptomatology; 5 of the stimulant users had developed psychosis, and 8 of the benzodiazepine users had developed depression. Therefore, long-term benzodiazepine abuse and dependence seems to carry a negative effect on mental health, with a significant risk of causing depression.[65]
Increased mortality was found in drug misusers that also used benzodiazepines against those that did not. Heavy alcohol misuse was also found to increase mortality among multiple-drug users.[66]
Crime
In a survey of police detainees carried out by the Australian Government, both legal and illegal users of benzodiazepines were found to be more likely to have lived on the streets, less likely to have been in full time work, and more likely to have used heroin or methamphetamines in the past 30 days from the date of taking part in the survey. Benzodiazepine users were also more likely to be receiving illegal incomes and more likely to have been arrested or imprisoned in the previous year. Benzodiazepines were sometimes reported to be abused alone, but most often formed part of a poly drug-using problem. Female users of benzodiazepines were more likely than men to be using heroin, whereas male users of benzodiazepines were more likely to report amphetamine use. Benzodiazepine users were more likely than non-users to claim government financial benefits, and benzodiazepine users who were also poly-drug users were the most likely to be claiming government financial benefits. Problem benzodiazepine use can be associated with crime. Those who reported using benzodiazepines alone were found to be in the mid range when compared to other drug using patterns in terms of property crimes and criminal breaches. Of the detainees reporting benzodiazepine use, one in five reported injection use, mostly of illicit temazepam, but some reported injecting prescribed temazepam or more rarely, other benzodiazepines. Injection was a concern in this survey due to increased health risks. The main problems highlighted in this survey were concerns of dependence, the potential for overdose of benzodiazepines in combination with opiates and the health problems associated with injection of benzodiazepines. The most consequential, and by far most commonly-abused benzodiazepine, was temazepam.[67] In the U.S. several jurisdictions have reported that benzodiazepine abuse by criminal detainees has surpassed that of opiates.[68]
Benzodiazepines have also been used as a tool of murder by serial killers, murderers, and as a murder weapon by those with the condition Munchausen syndrome by proxy.[69][70][71] Benzodiazepines have also been used to facilitate rape or robbery crimes, and benzodiazepine dependence has been linked to shoplifting due to the fugue state induced by the chronic use of the drug.[72][73] When benzodiazepines are used for criminal purposes against a victim they are often mixed with food or drink.[74] Flunitrazepam, temazepam, and midazolam are the most common benzodiazepines used to facilitate date rape.[75] Alprazolam has been abused for the purpose of carrying out acts of incest and for the corruption of adolescent girls.[76] However, alcohol remains the most common drug involved in cases of drug rape.[77] Although benzodiazepines and ethanol are the most frequent drugs used in sexual assaults, GHB is another potential date rape drug which has received increased media focus.[78] Some benzodiazepines are more associated with crime than others especially when abused or taken in combination with alcohol. The potent benzodiazepine flunitrazepam (Rohypnol), which has strong amnesia producing effects can cause abusers to become ruthless and also cause feelings of being invincible. This has led to some acts of extreme violence to others, often leaving abusers with no recollection of what they have done in their drug-induced state. It has been proposed that criminal and violent acts brought on by benzodiazepine abuse may be related to lowered serotonin levels via enhanced GABAergic effects.[79] Flunitrazepam has been implicated as the cause of one serial killers violent rampage, triggering off extreme aggression with anterograde amnesia.[80] A study on forensic psychiatric patients who had abused flunitrazepam at the time of their crimes found that the patients displayed extreme violence, lacked the ability to think clearly and experienced a loss of empathy for their victims while under the influence of flunitrazepam, and it was found that the abuse of alcohol or other drugs in combination with Flunitrazepam compounded the problem. Their behaviour under the influence of flunitrazepam was in contrast to their normal psychological state.[81]
Patients reporting to two emergency rooms in Canada with violence-related injuries were most often found to be intoxicated with alcohol and were significantly more likely to test positive for benzodiazepines (most commonly temazepam) than other groups of individuals, whereas other drugs were found to be insignificant in relation to violent injuries.[82]
Overdose
Benzodiazepines taken alone rarely cause severe complications in overdose,[83] and deaths after hospital admission are rare.[84] However, combinations of these drugs with alcohol or opiates is particularly dangerous, and may lead to coma and death.[85][86] The various benzodiazepines differ in their toxicity since they produce varying levels of sedation in overdose, with oxazepam being least toxic and least sedative and temazepam most toxic and most sedative in overdose. Temazepam is more frequently involved in drug-related deaths causing more deaths per million than other benzodiazepines.[87]
The antidote for all benzodiazepines is flumazenil (Anexate), a benzodiazepine antagonist, which is occasionally used empirically in patients presenting with unexplained loss of consciousness in an emergency room setting. As with all overdose situations, the care provider must be aware of the possibility that multiple substances were utilized by the patient. Supportive measures should be put in place prior to administration of any benzodiazepine antagonist in order to protect the patient from both the withdrawal effects and possible complications arising from simultaneous utilization of chemically-unrelated pharmaceutical compounds. A determination of possible deliberate overdose should be considered with appropriate scrutiny, and precautions taken to prevent any attempt by patient to commit further bodily harm.[88][89]
Flumazenil should be administered only by physicians that are familiar and suitably trained in the use of flumazenil in benzodiazepine overdose. Treating benzodiazepine overdose with flumazenil may reduce the chance of the patient being admitted to intensive care; however, caution should be exercised in the administration of flumazenil. The treating physician should bear in mind the possibility of mixed overdoses, especially mixed overdoses of other drugs or substances, as cocktails of drugs are often taken in overdose situations with their own overdose risks.
Pregnancy
In the United States the FDA has categorised benzodiazepines into either category D or category X benzodiazepines.[90] International statistics show that 3.5% of women consume psychotropic drugs during pregnancy and of that 3.5% up to 85% report using benzodiazepines during pregnancy making benzodiazepines the most commonly prescribed psychotropic drug consumed during pregnancy. Approximately 0.4% of all pregnancies are to women who have used benzodiazepines chronically throughout their pregnancy.[91] Neurodevelopmental and clinical symptoms are commonly found in babies exposed to benzodiazepines in utero. Benzodiazepine exposed babies have a low birth weight but catch up to normal babies at an early age but smaller head circumferences found in benzo babies persists. Other adverse effects of benzodiazepines taken during pregnancy are deviating neurodevelopmental and clinical symptoms including craniofacial anomalies, delayed development of pincer grasp, deviations in muscle tone and pattern of movements. Motor impairments in the babies are impeded for up to 1 year after birth. Gross motor development impairments takes 18 months to return to normal but fine motor function impairments persist.[92] In addition to the smaller head circumference found in benzodiazepine exposed babies mental retardation and lower intelligence occurs.[93]
Elderly
A large cohort study found that benzodiazepine use is associated with a significantly higher incidence of hip fracture. Benzodiazepines of a short half-life are as likely to be associated with hip fracture as long-acting benzodiazepines. Because hip fractures are a frequent cause of disability and death in the elderly, efforts have been underway to reduce benzodiazepine prescribing in the elderly.[94] Still, a law introduced in New York State reducing benzodiazepine use by 60% did not result in a measurable decrease in hip fractures.[95]
Elderly people are more sensitive to benzodiazepines and are at an increased risk of dependence. Up to 10% of hospital admissions of the elderly are because of benzodiazepines. The elderly are more sensitive to the intellectual and cognitive impairing effects of benzodiazepines including amnesia, diminished short-term recall, and increased forgetfulness. Chronic use of benzodiazepines and benzodiazepine dependence in the elderly can resemble dementia, depression or anxiety syndromes, which worsens with longer-term use of benzodiazepines. The success of gradual-tapering benzodiazepines is as great in the elderly as in younger people. Benzodiazepines should be prescribed to the elderly only with caution and only for a short period at low doses.[96]
Legal status
All benzodiazepines are Schedule IV in the USA under the Federal Controlled Substances Act, even when not on the market (for example, nitrazepam and bromazepam). In Canada benzodiazepines are also Schedule IV.[97]
Elsewhere in the world, however, benzodiazepines which are often subject to heavy abuse and addiction are often more strictly regulated or controlled. Temazepam, nimetazepam, and flunitrazepam are the world's most heavily regulated benzodiazepines.
Flunitrazepam (Rohypnol), Nimetazepam (Erimin), and Temazepam (Restoril; Normison) are treated more severely under International law than other benzodiazepines. For example, in the United States, despite being Schedule IV like any other benzodiazepine, flunitrazepam is not commercially available. It also carries tougher Federal penalties for trafficking and possession than other Schedule IV drugs. With the exception of cases involving 5 grams or more of cocaine or morphine, flunitrazepam is the only controlled substance whose first-offense simple possession is a federal felony. Temazepam is the only benzodiazepine which may require specially-coded prescriptions in some states.
Throughout Europe, including the United Kingdom, temazepam and flunitrazepam also carry tougher penalties for trafficking and possession.[98] In Ireland, temazepam and flunitrazepam are both Schedule 3 drugs under the Misuse of Drugs Act, while all other benzodiazepines are Schedule 4. As a result of continued abuse, illegal diversion, distrubtion, and clandestine manufacture in the Netherlands and Eastern Europe, Germany is currently in the process of possibly taking temazepam off of Anlage 3 (equivalent to Schedule 3 or Class C) of the BtMG (or Betäubungsmittelgesetz, which means Narcotics Act) and placing it under Anlage 2 (equivalent to Schedule 2 or Class B).
In the Netherlands, since October 1993, benzodiazepines are all placed on List 2 of the Opium Law, with the exception of any 20mg temazepam formulations, which are List 1. A prescription is needed for possession of all benzodiazepines.
In Australia, flunitrazepam and temazepam are restricted as Schedule 8 controlled drugs. As Schedule 8 controlled substances, it is illegal to possess either without an authority prescription from a registered doctor. In New Zealand, temazepam and flunitrazepam are completely illegal to possess and/or traffic. All other benzodiazepines are not illegal to possess for personal use, but distribution/traffic of any benzodiazepine is punishable by law.
In East Asia and Southeast Asia, temazepam and nimetazepam are often heavily controlled and restricted. In certain countries, triazolam, flunitrazepam, flutoprazepam, and midazolam are also restricted or controlled to certain degrees. In Hong Kong for example, temazepam and nimetazepam are regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. Triazolam, flunitrazepam, flutoprazepam, and midazolam are regulated under Schedule 2 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. Other benzodiazepines are not scheduled or controlled substances.
In Singapore, the Misuse of Drugs Act lists both temazepam and nimetazepam as Class A/Schedule I controlled drugs. Flutoprazepam, flunitrazepam, and triazolam are listed as Class C/Schedule II controlled drugs. Furthermore, a number of other benzodiazepines are regulated. Regulation of certain benzodiazepines under Schedule III was based on the relative ease by which they may be used to manufacture controlled benzodiazepines. They are as follows: camazepam, clonazepam, diazepam, estazolam, lorazepam, lormetazepam, nitrazepam, oxazepam, and prazepam. These benzodiazepines are regulated under Schedule III as controlled equipment, materials or substances useful for manufacturing controlled drugs. Restriction of these benzodiazepines is a measure against any clandestine manufacture of anyone of the controlled benzodiazepines, as seen with the growing illicit manufacture and distribution of temazepam in other regions of the world. Other benzodiazepines are not controlled drugs, but are available only by prescription and if used to manufacture any of the controlled benzodiazepines, automatically become Schedule III substances or material.
Internationally, temazepam, nimetazepam, and flunitrazepam are Schedule III drugs under the Convention on Psychotropic Substances.[99][100][101] As such, penalties for their possession and/or trafficking are more severe than all other benzodiazepine drugs, which are are classified as Schedule IV. Temazepam and nimetazepam continue to be the most widely abused benzodiazepines worldwide.[102] [103] Seizures of the two drugs by authorities are far higher in number than seizures of all the other benzodiazepines combined, including flunitrazepam. Worldwide, seizures of temazepam and nimetazepam may be comparable in number to seizures of the hypnotic, methaqualone. [104][105][106]
Various other countries limit the availability of benzodiazepines legally. Even though it is a commonly-prescribed class of drugs, the Medicare Prescription Drug, Improvement, and Modernization Act specifically states that insurance companies that provide Medicare Part D plans are not allowed to cover benzodiazepines.
See also
- Benzodiazepine withdrawal syndrome
- Benzodiazepine equivalence
- Nonbenzodiazepine
- Z drugs
- Barbiturate
References
- ↑ McKernan RM; Rosahl TW, Reynolds DS, Sur C, Wafford KA, Atack JR, Farrar S, Myers J, Cook G, Ferris P, Garrett L, Bristow L, Marshall G, Macaulay A, Brown N, Howell O, Moore KW, Carling RW, Street LJ, Castro JL, Ragan CI, Dawson GR, Whiting PJ. (June 2000). "Sedative but not anxiolytic properties of benzodiazepines are mediated by the GABA(A) receptor alpha1 subtype". Nature neuroscience. 3 (6): 587–92. doi:. PMID 10816315.
- ↑ Bulach R, Myles PS, Russnak M (2004). "Double-blind randomized controlled trial to determine extent of amnesia with midazolam given immediately before general anaesthesia" (PDF). Br J Anaesth 94 (3): 300–305. doi:. PMID 15567810. http://bja.oxfordjournals.org/cgi/reprint/94/3/300.pdf.
- ↑ Leikin JB, Krantz AJ, Zell-Kanter M, Barkin RL, Hryhorczuk DO (1989). "Clinical features and management of intoxication due to hallucinogenic drugs". Med Toxicol Adverse Drug Exp 4 (5): 324–50. PMID 2682130.
- ↑ Cooper, Jack R; Floyd E. Bloom, Robert H. Roth (January 15, 1996) (in Eng). The Complete Story of the Benzodiazepines (seventh ed.). USA: Oxford University Press. ISBN 0195103998. OCLC 223003583. http://www.etfrc.com/benzos1.htm. Retrieved on 07.
- ↑ Help For Mental Ills (Reports on Tests of Synthetic Drug Say The Results are Positive), New York Times, February 28, 1960, Page E9.
- ↑ Makers Worried On Tranquilizers, New York Times, August 28, 1960, Page F1.
- ↑ Warning Is Issued On Tranquilizers, New York Times, December 30, 1963, Page 23.
- ↑ Sternbach LH (1972). "The discovery of librium". Agents Actions 2 (4): 193–6. doi:. PMID 4557348.
- ↑ Lemmer B (2007). "The sleep-wake cycle and sleeping pills". Physiol. Behav. 90 (2-3): 285–93. doi:. PMID 17049955.
- ↑ Greenblatt DJ, Shader RI, Divoll M, Harmatz JS (1981). "Benzodiazepines: a summary of pharmacokinetic properties". Br J Clin Pharmacol 11 Suppl 1: 11S–16S. PMID 6133528.
- ↑ Summers RS, Schutte A, Summers B (December 1990). "Benzodiazepine use in a small community hospital. Appropriate prescribing or not?". S. Afr. Med. J. 78 (12): 721–5. PMID 2251629.
- ↑ Pym LJ, Cook SM, Rosahl T, McKernan RM, Atack JR (2005). "Selective labelling of diazepam-insensitive GABAA receptors in vivo using [3H]Ro 15-4513". Br. J. Pharmacol. 146 (6): 817–25. doi:. PMID 16184188.
- ↑ Hevers W, Lüddens H (1998). "The diversity of GABAA receptors. Pharmacological and electrophysiological properties of GABAA channel subtypes". Mol. Neurobiol. 18 (1): 35–86. doi:. PMID 9824848.
- ↑ Tardy M; Costa MF, Rolland B, Fages C, Gonnard P (April 1981). "Benzodiazepine receptors on primary cultures of mouse astrocytes". J Neurochem 36 (4): 1587–9. doi:. PMID 6267195.
- ↑ Atack JR (2003). "Anxioselective compounds acting at the GABAA receptor benzodiazepine binding site". Current drug targets. CNS and neurological disorders 2 (4): 213–32. doi:. PMID 12871032.
- ↑ McLean MJ; Macdonald RL. (February 1988). "Benzodiazepines, but not beta carbolines, limit high-frequency repetitive firing of action potentials of spinal cord neurons in cell culture". J Pharmacol Exp Ther. 244 (2): 789–95. PMID 2450203.
- ↑ Woods MG, Williams DC (1996). Multiple forms and locations for the peripheral-type benzodiazepine receptor. 52. 1805–1814. doi:.
- ↑ Tanimoto Yutaka; Onishi, Yoshiaki (1999). "Benzodiazepine Receptor Agonists Modulate Thymocyte Apoptosis Through Reduction of the Mitochondrial Transmembrane Potential". Jpn J Pharmacol. 79: 177–183. doi:. PMID 10202853.
- ↑ (reference 2 of Yutaka article)
- ↑ Danneberg P, Weber KH (1983). "Chemical structure and biological activity of the diazepines". Br J Clin Pharmacol 16 (Suppl 2): 231S–244S. PMID 6140944.
- ↑ Earley JV, Fryer RI, Ning RY (July 1979). "Quinazolines and 1,4-benzodiazepines. LXXXIX: Haptens useful in benzodiazepine immunoassay development". J Pharm Sci 68 (7): 845–50. doi:. PMID 458601.
- ↑ Prasad K; Krishnan PR, Al-Roomi K, Sequeira R. (June 2007). "Anticonvulsant therapy for status epilepticus". British journal of clinical pharmacology. 63 (6): 640–7. doi:. PMID 17439538.
- ↑ Treiman DM. (1989). "Pharmacokinetics and clinical use of benzodiazepines in the management of status epilepticus". Epilepsia. 30 (2): 4–10. doi:. PMID 2670537.
- ↑ Enabling Cookies: BNF.org
- ↑ Uhlenhuth EH, Balter MB, Ban TA, Yang K (1999). "International study of expert judgment on therapeutic use of benzodiazepines and other psychotherapeutic medications: VI. Trends in recommendations for the pharmacotherapy of anxiety disorders, 1992-1997". Depress Anxiety 9 (3): 107–16. doi:. PMID 10356648.
- ↑ Uhlenhuth EH, Balter MB, Ban TA, Yang K (December 1995). "International study of expert judgement on therapeutic use of benzodiazepines and other psychotherapeutic medications: II. Pharmacotherapy of anxiety disorders". J Affect Disord 35 (4): 153–62. doi:. PMID 8749980.
- ↑ Uhlenhuth EH, Balter MB, Ban TA, Yang K (December 1999). "Trends in recommendations for the pharmacotherapy of anxiety disorders by an international expert panel, 1992-1997". Eur Neuropsychopharmacol 9 Suppl 6: S393–8. doi:. PMID 10622685.
- ↑ Uhlenhuth EH, Balter MB, Ban TA, Yang K (December 1999). "International study of expert judgment on therapeutic use of benzodiazepines and other psychotherapeutic medications: IV. Therapeutic dose dependence and abuse liability of benzodiazepines in the long-term treatment of anxiety disorders". J Clin Psychopharmacol 19 (6 Suppl 2): 23S–29S. doi:. PMID 10587281. http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0271-0749&volume=19&issue=6&spage=23S.
- ↑ Stevens JC, Pollack MH (2005). "Benzodiazepines in clinical practice: consideration of their long-term use and alternative agents". J Clin Psychiatry 66 Suppl 2: 21–7. PMID 15762816. http://article.psychiatrist.com/?ContentType=START&ID=10001225.
- ↑ Bruce SE, Vasile RG, Goisman RM, Salzman C, Spencer M, Machan JT, Keller MB (August 2003). "Are benzodiazepines still the medication of choice for patients with panic disorder with or without agoraphobia?". Am J Psychiatry 160 (8): 1432–8. doi:. PMID 12900305.
- ↑ Enabling Cookies: BNF.org
- ↑ 32.0 32.1 32.2 Enabling Cookies: BNF.org
- ↑ Chabria SB (2008). "Inpatient management of alcohol withdrawal: a practical approach". Signa Vitae 3 (1): 24–29. http://signavitae.com/index.php?option=com_content&task=view&id=67&Itemid=67.
- ↑ Wilson A, Vulcano B (1984). "A double-blind, placebo-controlled trial of magnesium sulfate in the ethanol withdrawal syndrome". Alcohol. Clin. Exp. Res. 8 (6): 542–5. doi:. PMID 6393805.
- ↑ Raistrick, D, Heather N, Godfrey C. "Review of the Effectiveness of Treatment for Alcohol Problems" (PDF). National Treatment Agency for Substance Misuse, London. Retrieved on 2008-06-19.
- ↑ Enabling Cookies: BNF.org
- ↑ Bottaï T; Hüe B, Hillaire-Buys D, Barbe A, Alric R, Pouget R, Petit P. (December 1995). "Clonazepam in acute mania: time-blind evaluation of clinical response and concentrations in plasma". Journal of affective disorders. 36 (1-2): 21–7. doi:. PMID 8988261.
- ↑ Curtin F; Schulz P. (March 2004). "Clonazepam and lorazepam in acute mania: a Bayesian meta-analysis". Journal of affective disorders. 78 (3): 201–8. doi:. PMID 15013244.
- ↑ Yamashita K; Wijayathilaka TP, Kushiro T, Umar MA, Taguchi K, Muir WW. (January 2007). "Anesthetic and cardiopulmonary effects of total intravenous anesthesia using a midazolam, ketamine and medetomidine drug combination in horses". The Journal of veterinary medical science / the Japanese Society of Veterinary Science. 69 (1): 7–13. PMID 17283393.
- ↑ Woolfson MW; Foran JA, Freedman HM, Moore PA, Shulman LB, Schnitman PA. (October 1980). "Immobilization of baboons (Papio anubis) using ketamine and diazepam". Laboratory animal science. 30 (5): 902–4. PMID 7431875.
- ↑ Pulley AC; Roberts JA, Lerche NW. (December 2004). "Four preanesthetic oral sedation protocols for rhesus macaques (Macaca mulatta)". Journal of zoo and wildlife medicine : official publication of the American Association of Zoo Veterinarians. 35 (4): 497–502. PMID 15732590.
- ↑ Sanhouri AA; Jones RS, Dobson H. (Jul-Aug 1991). "Preliminary results on the effects of diazepam on physiological responses to transport in male goats". The British veterinary journal. 147 (4): 388–9. PMID 1913136.
- ↑ Dilov P; Dimitrov S, Nikolov A, Chaleva E, Panchev I. (1984). "[Pharmacological and clinico-pharmacological studies of diazepam powder in suspensions]". Veterinarno-meditsinski nauki. 21 (3): 96–103. doi:. PMID 6740928.
- ↑ Yamaya Y; Iwakami E, Goto M, Koie H, Watari T, Tanaka S, Takeuchi A, Tokuriki M. (September 2004). "A case of shaker dog disease in a miniature dachshund". The Journal of veterinary medical science / the Japanese Society of Veterinary Science. 66 (9): 1159–60. PMID 15472486. http://www.jstage.jst.go.jp/article/jvms/66/9/1159/_pdf.
- ↑ Wagner SO; Podell M, Fenner WR. (September 15, 1997). "Generalized tremors in dogs: 24 cases (1984-1995)". Journal of the American Veterinary Medical Association. 211 (6): 731–5. PMID 9301744.
- ↑ Polizopoulou ZS; Kazakos G, Georgiadis G, Soubasis N, Koutinas Ch, Koutinas AF. (December 2002). "Presumed localized tetanus in two cats". Journal of feline medicine and surgery. 4 (4): 209–12. doi:. PMID 12468315.
- ↑ Bateman SW; Parent JM. (November 15, 1999). "Clinical findings, treatment, and outcome of dogs with status epilepticus or cluster seizures: 156 cases (1990-1995)". Journal of the American Veterinary Medical Association. 215 (10): 1463–8. PMID 10579043.
- ↑ Löscher W; Potschka H, Rieck S, Tipold A, Rundfeldt C. (October 2004). "Anticonvulsant efficacy of the low-affinity partial benzodiazepine receptor agonist ELB 138 in a dog seizure model and in epileptic dogs with spontaneously recurrent seizures". Epilepsia. 45 (10): 1228–39. doi:. PMID 15461677.
- ↑ Podell M. (July 1996). "Seizures in dogs". The Veterinary clinics of North America. Small animal practice. 26 (4): 779–809. PMID 8813750.
- ↑ Singh K; Sobti VK, Bansal PS, Rathore SS. (December 1989). "Studies on lorazepam as a premedicant for thiopental anaesthesia in the dog". Zentralblatt für Veterinärmedizin. Reihe A. 36 (10): 750–4. PMID 2515684.
- ↑ Nel PJ; Taylor A, Meltzer DG, Haupt MA. (March 2000). "Capture and immobilisation of aardvark (Orycteropus afer) using different drug combinations". Journal of the South African Veterinary Association. 71 (1): 58–63. PMID 10949520.
- ↑ medicinenet. "BENZODIAZEPINES - ORAL". medicinenet.com. Retrieved on 10 April 2008.
- ↑ 53.0 53.1 Paradoxical Reactions to Benzodiazepines
- ↑ Cole JO; Kando JC. (1993). "Adverse behavioral events reported in patients taking alprazolam and other benzodiazepines". The Journal of clinical psychiatry. 54 (49-61): 62–3. PMID 8262890.
- ↑ Drummer, OH (2002). "Benzodiazepines — Effects on Human Performance and Behavior" (PDF). Forensic Science Review.
- ↑ "Letter: Tranquilizers causing aggression". British medical journal. 1 (5952): 266. February 1, 1975. PMID 234269.
- ↑ Senninger JL; Laxenaire M. (1995). "[Violent paradoxal reactions secondary to the use of benzodiazepines]". Annales médico-psychologiques. 153 (4): 278–81. doi:. PMID 7618826.
- ↑ O'brien CP (2005). "Benzodiazepine use, abuse, and dependence". J Clin Psychiatry 66 (Suppl 2): 28–33. PMID 15762817.
- ↑ Dr JG McConnell (May 2007). "The Clinicopharmacotherapeutics of Benzodiazepine and Z drug dose Tapering Using Diazepam".
- ↑ Professor Heather Ashton (2002). "Benzodiazepines: How They Work and How To Withdraw".
- ↑ Söderpalm B; Svensson L, Hulthe P, Johannessen K, Engel JA. (1991). "Evidence for a role for dopamine in the diazepam locomotor stimulating effect". Psychopharmacology. 104 (1): 97–102. doi:. PMID 1679244.
- ↑ Darke S; Ross J, Cohen J. (1994). "The use of benzodiazepines among regular amphetamine users". Addiction (Abingdon, England). 89 (12): 1683–90. PMID 7866252.
- ↑ Williamson S; Gossop M, Powis B, Griffiths P, Fountain J, Strang J. (March 14, 1997). "Adverse effects of stimulant drugs in a community sample of drug users". Drug and alcohol dependence. 44 (2-3): 87–94. doi:. PMID 9088780.
- ↑ Gerada C; Ashworth M (1997). "ABC of mental health. Addiction and dependence--I: Illicit drugs". BMJ 315 (7103): 297–300. PMID 9274553.
- ↑ Woody GE; Mc Lellan AT O'Brien CP. (1979). "Development of psychiatric illness in drug abusers. Possible role of drug preference". The New England journal of medicine. 301 (24): 1310–4. PMID 41182.
- ↑ Gossop M; Stewart D, Treacy S, Marsden J. (2002). "A prospective study of mortality among drug misusers during a 4-year period after seeking treatment". Addiction (Abingdon, England). 97 (1): 39–47. doi:. PMID 11895269.
- ↑ Government, Australian (May 2007). "Benzodiazepine use and harms among police detainees in Australia" (PDF). Australian Institute of Criminology.
- ↑ Yacoubian GS. (January 2003). Correlates of benzodiazepine use among a sample of arrestees surveyed through the Arrestee Drug Abuse Monitoring (ADAM) Program. 38. Substance use & misuse.. pp. 127–39. PMID 12602810.
- ↑ Missliwetz J (Jul-Aug 1981). [Serial homicide in the Vienna-Lainz hospital]. 194. Archiv für Kriminologie.. pp. 1–7. PMID 7979864.
- ↑ Valentine JL; Schexnayder S, Jones JG, Sturner WQ. (September 1997). Clinical and toxicological findings in two young siblings and autopsy findings in one sibling with multiple hospital admissions resulting in death. Evidence suggesting Munchausen syndrome by proxy. 18. The American journal of forensic medicine and pathology : official publication of the National Association of Medical Examiners.. pp. 276–81. PMID 9290875.
- ↑ Saito T; Takeichi S, Nakajima Y, Yukawa N, Osawa M. (Nov-Dec 1997). A case of homicidal poisoning involving several drugs. 194. Journal of analytical toxicology.. pp. 1–7. PMID 9399131.
- ↑ Boussairi A; Dupeyron JP, Hernandez B, Delaitre D, Beugnet L, Espinoza P, Diamant-Berger O. (1996). Urine benzodiazepines screening of involuntarily drugged and robbed or raped patients. 34. Journal of toxicology. Clinical toxicology.. pp. 721–4. PMID 8941203.
- ↑ Tang CP; Pang AH, Ungvari GS. (July 1996). Shoplifting and robbery in a fugue state. 36. Medicine, science, and the law.. pp. 265–8. PMID 8918097.
- ↑ Ohshima T. (January 2006). A case of drug-facilitated sexual assault by the use of flunitrazepam. 13. Journal of clinical forensic medicine.. pp. 44–5. PMID 16087387.
- ↑ Negrusz A; Gaensslen RE. (August 2003). "Analytical developments in toxicological investigation of drug-facilitated sexual assault". Analytical and bioanalytical chemistry. 376 (8): 1192–7. doi:. PMID 12682705.
- ↑ Kintz P; Villain M, Chèze M, Pépin G. (October 29, 2005). Identification of alprazolam in hair in two cases of drug-facilitated incidents. 153. Forensic science international.. pp. 222–6. PMID 16139113.
- ↑ Weir E. (July 10, 2001). "Drug-facilitated date rape". journal de l'Association medicale canadienne. (CMAJ : Canadian Medical Association) 165 (1): 80. PMID 11468961. http://www.cmaj.ca/cgi/content/full/165/1/80.
- ↑ Saint-Martin P; Furet Y, O'Byrne P, Bouyssy M, Paintaud G, Autret-Leca E. (Mar-Apr 2006). [Chemical submission: a literature review]. 61. Thérapie.. pp. 145–50. doi:. PMID 16886708.
- ↑ Dåderman A; Lidberg L. (March 3, 1999). [Rohypnol should be classified as a narcotic]. 96. Läkartidningen.. pp. 1005–7. doi:. PMID 10093441.
- ↑ Dåderman AM; Strindlund H, Wiklund N, Fredriksen SO, Lidberg L. (October 14, 2003). The importance of a urine sample in persons intoxicated with flunitrazepam--legal issues in a forensic psychiatric case study of a serial murderer. 137. Forensic science international.. pp. 21–7. PMID 14550609.
- ↑ Dåderman AM; Fredriksson B, Kristiansson M, Nilsson LH, Lidberg L. (2002). Violent behavior, impulsive decision-making, and anterograde amnesia while intoxicated with flunitrazepam and alcohol or other drugs: a case study in forensic psychiatric patients. 30. The journal of the American Academy of Psychiatry and the Law.. pp. 238–51. PMID 12108561.
- ↑ Macdonald S; Wells S, Giesbrecht N, Cherpitel CJ. (June 1, 1999). Demographic and substance use factors related to violent and accidental injuries: results from an emergency room study. 55. Drug and alcohol dependence.. pp. 53–61. PMID 10402149.
- ↑ Gaudreault P, Guay J, Thivierge RL, Verdy I (1991). "Benzodiazepine poisoning. Clinical and pharmacological considerations and treatment". Drug Saf 6 (4): 247–65. doi:. PMID 1888441.
- ↑ Höjer J, Baehrendtz S, Gustafsson L (August 1989). "Benzodiazepine poisoning: experience of 702 admissions to an intensive care unit during a 14-year period". J. Intern. Med. 226 (2): 117–22. PMID 2769176.
- ↑ Dietze P, Jolley D, Fry C, Bammer G (May 2005). "Transient changes in behaviour lead to heroin overdose: results from a case-crossover study of non-fatal overdose". Addiction 100 (5): 636–42. doi:. PMID 15847621.
- ↑ Hammersley R; Cassidy MT, Oliver J (July 1995). "Drugs associated with drug-related deaths in Edinburgh and Glasgow, November 1990 to October 1992". Addiction 90 (7): 959–65. doi:. PMID 7663317.
- ↑ Buckley NA, Dawson AH, Whyte IM, O'Connell DL (January 1995). "Relative toxicity of benzodiazepines in overdose". BMJ 310 (6974): 219–21. PMID 7866122. http://bmj.com/cgi/pmidlookup?view=long&pmid=7866122.
- ↑ Weinbroum AA, Flaishon R, Sorkine P, Szold O, Rudick V (September 1997). "A risk-benefit assessment of flumazenil in the management of benzodiazepine overdose". Drug Saf 17 (3): 181–96. doi:. PMID 9306053.
- ↑ Buckley NA, Dawson AH, Whyte IM, O'Connell DL (January 1995). "Relative toxicity of benzodiazepines in overdose". BMJ 310 (6974): 219–21. PMID 7866122. http://www.bmj.com/cgi/content/abstract/310/6974/219.
- ↑ BJC Behavioral Health. "Benzodiazepines". BJC. Retrieved on 18 April 2008.
- ↑ F, Marchetti; Romero M, Bonati M, Tognoni G (December 1993). "Use of psychotropic drugs during pregnancy" (pdf). European Journal of Clinical Pharmacology (Springer Berlin / Heidelberg) 45 (6): 495–501. doi:. ISSN 1432-1041. PMID 7908878. http://www.springerlink.com/content/x3033x8520251102/fulltext.pdf.
- ↑ L, Laegreid; Hagberg G, Lundberg A (April 1992). "Neurodevelopment in late infancy after prenatal exposure to benzodiazepines--a prospective study". Neuropediatrics 23 (2): 60–7. PMID 1351263.
- ↑ L, Laegreid (1990). "Clinical observations in children after prenatal benzodiazepine exposure". Dev Pharmacol Ther 15 (3-4): 186–8. PMID 1983095.
- ↑ Wagner AK, Zhang F, Soumerai SB, Walker AM, Gurwitz JH, Glynn RJ, Ross-Degnan D (July 2004). "Benzodiazepine use and hip fractures in the elderly: who is at greatest risk?". Arch. Intern. Med. 164 (14): 1567–72. doi:. PMID 15277291.
- ↑ Wagner AK, Ross-Degnan D, Gurwitz JH, Zhang F, Gilden DB, Cosler L, Soumerai SB (January 2007). "Effect of New York State regulatory action on benzodiazepine prescribing and hip fracture rates" (PDF). Ann. Intern. Med. 146 (2): 96–103. PMID 17227933. http://www.annals.org/cgi/reprint/146/2/96.pdf.
- ↑ http://psychservices.psychiatryonline.org/cgi/content/full/55/3/233 Practical Geriatrics: Use of Benzodiazepines Among Elderly Patients
- ↑ DEA, USA. "Benzodiazepines". Drug Enforcement Agency.
- ↑ UK, Gov (January 2006). "List of Drugs Currently Controlled Under The Misuse of Drugs Legislation". Misuse of Drugs Act UK. Retrieved on 10, 2007. Retrieved on 06 2007.
- ↑ Annual Estimates Of Requirements Of Narcotic Drugs, Manufacture Of Synthetic Drugs, Opium Production And Cultivation Of The
- ↑ http://www.cnb.gov.sg/ [Central Narcotics Bureau, Singapore]
- ↑ "Green List—List of psychotropic substances under international control" (PDF). International Narcotics Control Board (23rd edition, August 2003). Retrieved on 2007-11-25.
- ↑ http://www.cnb.gov.sg/ [Central Narcotics Bureau, Singapore]
- ↑ "Green List -- List of psychotropic substances under international control" (PDF). International Narcotics Control Board (23rd edition, August 2003). Retrieved on 2007-11-25.
- ↑ International Narcotics Control Board (INCB), 2006. Report of the International Narcotics Control Board for 2005. United Nations INCB, New York.
- ↑ Beare, M. “Structures, Strategies, and Tactics of Transnational Criminal Organizations: Critical Issues for Enforcement” Paper presented at the Australian Institute of Criminology, Australian Customs Service, and Australian Federal Police Transnational Crime Conference, Canberra
- ↑ Drugs and Crime Prevention Committee (DCPC), 2006. Inquiry into possible international epidemic of misuse/abuse of temazepam; Parliament of Victoria, Melbourne.
External links
- Ashton CH (2002-08-01). "Benzodiazepines How They Work & How to Withdraw". benzo.org.uk. Retrieved on 2008-06-19.
- Ashton CH (2007-04-01). "Benzodiazepine Equivalence Table". benzo.org.uk. Retrieved on 2008-06-19.
- Fruchtengarten L, (1998-04-01). "Benzodiazepines". PIM G008. International Programme on Chemical Safety (IPCS) INCHEM. Retrieved on 2008-06-19.
- Longo LP, Johnson B (2000-04-01). "Benzodiazepines Side Effects, Abuse Risk and Alternatives". Addiction: Part I. American Academy of Family Physicians. Retrieved on 2008-06-19.
- "An Overview of the History, Chemistry, and Pharmacodynamics of Benzodiazepines". The Eaton T. Fores Research Center (2002-01-01). Retrieved on 2008-06-19.
- "Benzodiazepines advanced consumer information". drugs.com (2005-02-24). Retrieved on 2008-06-19.
|
|||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||