Aspirin
 |
|
 |
|
|
Aspirin
|
|
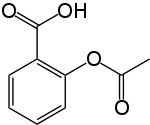
| Systematic (IUPAC) name | |
| 2-(acetyloxy)benzoic acid | |
| Identifiers | |
| CAS number | |
| ATC code | A01 B01, N02 |
| PubChem | |
| DrugBank | |
| ChemSpider | |
| Chemical data | |
| Formula | C9H8O4 |
| Mol. mass | 180.157 g/mol |
| SMILES | & |
| Synonyms | 2-acetyloxybenzoic acid acetylsalicylate acetylsalicylic acid O-acetylsalicylic acid |
| Physical data | |
| Density | 1.40 g/cm³ |
| Melt. point | 135 °C (275 °F) |
| Boiling point | 140 °C (284 °F) (decomposes) |
| Solubility in water | 10 mg/mL (20 °C) |
| Pharmacokinetic data | |
| Bioavailability | Rapidly and completely absorbed |
| Protein binding | 99.6% |
| Metabolism | Hepatic |
| Half life | 300–650 mg dose: 3.1–3.2hrs 1 g dose: 5 hours 2 g dose: 9 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status | |
| Routes | Most commonly oral, also rectal. Lysine acetylsalicylate may be given IV or IM |
Aspirin (USAN), also known as acetylsalicylic acid (pronounced /əˌsɛtɨlsælɨˌsɪlɨk ˈæsɨd/, abbreviated ASA), is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication.
Aspirin also has an antiplatelet, or "anti-clotting", effect and is used in long-term, low doses to prevent heart attacks, strokes and blood clot formation in people at high risk for developing blood clots.[1] It has also been established that low doses of aspirin may be given immediately after a heart attack to reduce the risk of another heart attack or of the death of cardiac tissue.[2][3]
The main undesirable side effects of aspirin are gastrointestinal ulcers, stomach bleeding and tinnitus, especially in higher doses. In children and adolescents, aspirin is no longer used to control flu-like symptoms or the symptoms of chickenpox or other viral illnesses, due to the risk of Reye's syndrome.[4]
Aspirin was the first-discovered member of the class of drugs known as non-steroidal anti-inflammatory drugs (NSAIDs), not all of which are salicylates, although they all have similar effects and most have inhibition of the enzyme cyclooxygenase as their mechanism of action. Today, aspirin is one of the most widely used medications in the world, with an estimated 40,000 metric tons of it being consumed each year.[5] In countries where Aspirin is a registered trademark owned by Bayer, the generic term is acetylsalicylic acid (ASA).[6][7]
Contents |
History
Medicines containing derivatives of salicylic acid, structurally similar to aspirin, have been in medical use since ancient times. Salicylate-rich willow bark extract became recognized for its specific effects on fever, pain and inflammation in the mid-eighteenth century. By the nineteenth century pharmacists were experimenting with and prescribing a variety of chemicals related to salicylic acid, the active component of willow extract.
A French chemist, Charles Frederic Gerhardt, was the first to prepare acetylsalicylic acid (named aspirin in 1899) in 1853. In the course of his work on the synthesis and properties of various acid anhydrides, he mixed acetyl chloride with a sodium salt of salicylic acid (sodium salicylate). A vigorous reaction ensued, and the resulting melt soon solidified.[8] Since no structural theory existed at that time, Gerhardt called the compound he obtained "salicylic-acetic anhydride" (wasserfreie Salicylsäure-Essigsäure). This preparation of aspirin ("salicylic-acetic anhydride") was one of the many reactions Gerhardt conducted for his paper on anhydrides, but he did not pursue it further.

Six years later, in 1859, von Gilm obtained analytically pure acetylsalicylic acid (which he called "acetylierte Salicylsäure", acetylated salicylic acid) by a reaction of salicylic acid and acetyl chloride.[9] In 1869 Schröder, Prinzhorn and Kraut repeated both Gerhardt's (from sodium salicylate) and von Gilm's (from salicylic acid) syntheses and concluded that both reactions gave the same compound—acetylsalicylic acid. They were first to assign to it the correct structure with the acetyl group connected to the phenolic oxygen.[10]
In 1897, scientists at the drug and dye firm Bayer began investigating acetylsalicylic acid as a less-irritating replacement for standard common salicylate medicines. By 1899, Bayer had dubbed this drug Aspirin and was selling it around the world.[11]The name Aspirin is derived from A = Acetyl and "Spirsäure" = an old (German) name for salicylic acid.[12] Aspirin's popularity grew over the first half of the twentieth century, spurred by its effectiveness in the wake of Spanish flu pandemic of 1918, and aspirin's profitability led to fierce competition and the proliferation of aspirin brands and products, especially after the American patent held by Bayer expired in 1917.[13][14]
Aspirin's popularity declined after the market releases of paracetamol (acetaminophen) in 1956 and ibuprofen in 1969.[15] In the 1960s and 1970s, John Vane and others discovered the basic mechanism of aspirin's effects, while clinical trials and other studies from the 1960s to the 1980s established aspirin's efficacy as an anti-clotting agent that reduces the risk of clotting diseases.[16] Aspirin sales revived considerably in the last decades of the twentieth century, and remain strong in the twenty-first, thanks to widespread use as a preventive treatment for heart attacks and strokes.[17]
Trademark in most countries
As part of war reparations specified in the 1919 Treaty of Versailles following Germany's surrender after World War I, Aspirin (along with Heroin) lost its status as a registered trademark in France, Russia, the United Kingdom, and the United States, where it became a generic name and can be spelled in lower case.[18][19][20] Today, "aspirin" is a generic word in Australia, Argentina, Britain, France, India, Ireland, Japan, New Zealand, Pakistan, the Philippines, South Africa and the United States.[21] Aspirin remains a registered trademark of Bayer in Germany, Canada, Mexico, and in over 80 other countries, where the first letter of its name should be capitalized and used only in reference to and on ASA products manufactured and marketed by Bayer.[22][23]
Therapeutic uses
Aspirin is one of the most frequently used drugs in the treatment of mild to moderate pain, including that of migraines and fever.[24][25] It is often combined with other non-steroidal anti-inflammatory drugs and opioid analgesics in the treatment of moderate to severe pain.[26]
In high doses, aspirin and other salicylates are used in the treatment of rheumatic fever, rheumatic arthritis, and other inflammatory joint conditions. In lower doses, aspirin also inhibits platelet aggregation, and has been shown to reduce the incidence of transient ischemic attacks and unstable angina in men, and can be used prophylactically. It is also used in the treatment of pericarditis, coronary artery disease, and acute myocardial infarction.[27][28] Low doses of aspirin are also recommended for the prevention of stroke, and myocardial infarction in patients with diagnosed cardiovascular disease. It is of no value in people without proven heart disease.[29]
Pediatric
Aspirin is no longer used in children and adolescents due to the risk of Reye's syndrome (see Adverse effects); paracetamol (known as acetaminophen in the United States) or non-salicylate NSAIDs, such as ibuprofen, are now used instead. Kawasaki disease remains one of the few indications for aspirin use in children, although even this use has been questioned by some authors.[30] In the United Kingdom, the only indications for aspirin use in children and adolescents under 16 are Kawasaki disease and prevention of blood clot formation.
Experimental

Aspirin has been theorized to reduce cataract formation in diabetic patients, but one study showed it was ineffective for this purpose.[31] The role of aspirin in reducing the incidence of many forms of cancer has also been widely studied. In several studies, aspirin use did not reduce the incidence of prostate cancer.[32][33] Its effects on the incidence of pancreatic cancer are mixed; one study published in 2004 found a statistically significant increase in the risk of pancreatic cancer among women,[34] while a meta-analysis of several studies, published in 2006, found no evidence that aspirin or other NSAIDs are associated with an increased risk for the disease.[35] The drug may be effective in reduction of risk of various cancers, including those of the colon,[36][37][38][39] lung,[40][41] and possibly the upper GI tract, though some evidence of its effectiveness in preventing cancer of the upper GI tract has been inconclusive.[42][43][42] Its preventative effect against adenocarcinomas may be explained by its inhibition of COX-2 enzymes expressed in them.[44]
Veterinary uses
Aspirin has been used to treat pain and arthritis in veterinary medicine, primarily in cats and dogs, although it is often not recommended for this purpose, as there are newer medications available with fewer side effects in these animals. Dogs, for example, are particularly susceptible to the gastrointestinal side effects associated with salicylates.[45] Horses have also been given aspirin for pain relief, although it is not commonly used due to its relatively short-lived analgesic effects. Horses are also fairly sensitive to the gastrointestinal side effects. Nevertheless, it has shown promise in its use as an anticoagulant, mostly in cases of laminitis.[46] Aspirin should only be used in animals under the direct supervision of a veterinarian.
Mechanism of action

Discovering the mechanism
In 1971, British pharmacologist John Robert Vane, then employed by the Royal College of Surgeons in London, showed that aspirin suppressed the production of prostaglandins and thromboxanes.[47][48] For this discovery, he was awarded both a Nobel Prize in Physiology or Medicine in 1982 and a knighthood.
Suppression of prostaglandins and thromboxanes
Aspirin's ability to suppress the production of prostaglandins and thromboxanes is due to its irreversible inactivation of the cyclooxygenase (COX) enzyme. Cyclooxygenase is required for prostaglandin and thromboxane synthesis. Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the COX enzyme. This makes aspirin different from other NSAIDs (such as diclofenac and ibuprofen), which are reversible inhibitors.
Low-dose, long-term aspirin use irreversibly blocks the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation. This anticoagulant property makes aspirin useful for reducing the incidence of heart attacks.[49] 40 mg of aspirin a day is able to inhibit a large proportion of maximum thromboxane A2 release provoked acutely, with the prostaglandin I2 synthesis being little affected; however, higher doses of aspirin are required to attain further inhibition.[50]
Prostaglandins are local hormones produced in the body and have diverse effects in the body, including the transmission of pain information to the brain, modulation of the hypothalamic thermostat, and inflammation. Thromboxanes are responsible for the aggregation of platelets that form blood clots. Heart attacks are primarily caused by blood clots, and low doses of aspirin are seen as an effective medical intervention for acute myocardial infarction. The major side-effect of this is that because the ability of blood to clot is reduced, excessive bleeding may result from the use of aspirin.
COX-1 and COX-2 inhibition
There are at least two different types of cyclooxygenase: COX-1 and COX-2. Aspirin irreversibly inhibits COX-1 and modifies the enzymatic activity of COX-2. Normally COX-2 produces prostanoids, most of which are pro-inflammatory. Aspirin-modified COX-2 produces lipoxins, most of which are anti-inflammatory. Newer NSAID drugs called COX-2 selective inhibitors have been developed that inhibit only COX-2, with the intent to reduce the incidence of gastrointestinal side-effects.[5]
However, several of the new COX-2 selective inhibitors, such as Vioxx, have been withdrawn recently, after evidence emerged that COX-2 inhibitors increase the risk of heart attack. It is proposed that endothelial cells lining the microvasculature in the body express COX-2, and, by selectively inhibiting COX-2, prostaglandins (specifically PGI2; prostacyclin) are downregulated with respect to thromboxane levels, as COX-1 in platelets is unaffected. Thus, the protective anti-coagulative effect of PGI2 is decreased, increasing the risk of thrombus and associated heart attacks and other circulatory problems. Since platelets have no DNA, they are unable to synthesize new COX once aspirin has irreversibly inhibited the enzyme, an important difference with reversible inhibitors.
Additional mechanisms
Aspirin has been shown to have at least three additional modes of action. It uncouples oxidative phosphorylation in cartilaginous (and hepatic) mitochondria, by diffusing from the inner membrane space as a proton carrier back into the mitochondrial matrix, where it ionizes once again to release protons.[51] In short, aspirin buffers and transports the protons. When high doses of aspirin are given, aspirin may actually cause fever due to the heat released from the electron transport chain, as opposed to the antipyretic action of aspirin seen with lower doses. Additionally, aspirin induces the formation of NO-radicals in the body, which have been shown in mice to have an independent mechanism of reducing inflammation. This reduced leukocyte adhesion, which is an important step in immune response to infection; however, there is currently insufficient evidence to show that aspirin helps to fight infection.[52] More recent data also suggests that salicylic acid and its derivatives modulate signaling through NF-κB.[53] NF-κB is a transcription factor complex that plays a central role in many biological processes, including inflammation.
Chemistry
Aspirin is an acetyl derivative of salicylic acid that is a white, crystalline, weakly acidic substance, with melting point 135°C. Acetylsalicylic acid decomposes rapidly in solutions of ammonium acetate or of the acetates, carbonates, citrates or hydroxides of the alkali metals. Acetylsalicylic acid is stable in dry air, but gradually hydrolyses in contact with moisture to acetic and salicylic acids. In solution with alkalis, the hydrolysis proceeds rapidly and the clear solutions formed may consist entirely of acetate and salicylate.[54]
Synthesis
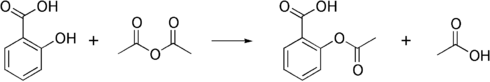
The synthesis of aspirin is classified as an esterification reaction. Salicylic acid is treated with acetic anhydride, an acid derivative, causing a chemical reaction that turns salicylic acid's phenol group into an acetyl group, (R-OH --> R-OCOCH3). This process yields aspirin and acetic acid, which is considered a byproduct of this reaction. Small amounts of sulfuric acid (and occasionally phosphoric acid) are almost always used as a catalyst. This method is commonly employed in undergraduate teaching labs.[55]
Formulations containing high concentrations of aspirin often smell like vinegar.[56] This is because aspirin can decompose through hydrolysis in moist conditions, yielding salicylic acid and acetic acid.[57]
The acid dissociation constant (pKa) for acetylsalicylic acid is 3.5 at 25 °C.[58]
Polymorphism
Polymorphism, or the ability of a substance to form more than one crystal structure, is important in the development of pharmaceutical ingredients. Many drugs are receiving regulatory approval for only a single crystal form or polymorph. For a long time, only one crystal structure for aspirin was known, although there had been indications that aspirin might have a second crystalline form since the 1960s. The elusive second polymorph was first discovered by Vishweshwar and coworkers in 2005,[59] and fine structural details were given by Bond et al.[60] A new crystal type was found after attempted co-crystallization of aspirin and levetiracetam from hot acetonitrile. The form II is only stable at 100 K and reverts back to form I at ambient temperature. In the (unambiguous) form I, two salicylic molecules form centrosymmetric dimers through the acetyl groups with the (acidic) methyl proton to carbonyl hydrogen bonds, and in the newly claimed form II, each salicylic molecule forms the same hydrogen bonds with two neighboring molecules instead of one. With respect to the hydrogen bonds formed by the carboxylic acid groups both polymorphs form identical dimer structures.
Pharmacokinetics
Salicylic acid is a weak acid, and very little of it is ionized in the stomach after oral administration. Acetylsalicylic acid is poorly soluble in the acidic conditions of the stomach, which can delay absorption of high doses for 8 to 24 hours. In addition to the increased pH of the small intestine, aspirin is rapidly absorbed there due to the increased surface area, which in turn allows more of the salicylate to dissolve. Due to the issue of solubility, however, aspirin is absorbed much more slowly during overdose, and plasma concentrations can continue to rise for up to 24 hours after ingestion.[61][62][63]
About 50–80% of salicylate in the blood is bound by protein while the rest remains in the active, ionized state; protein binding is concentration-dependent. Saturation of binding sites leads to more free salicylate and increased toxicity. The volume of distribution is 0.1–0.2 l/kg. Acidosis increases the volume of distribution because of enhancement of tissue penetration of salicylates.[63]
As much as 80% of therapeutic doses of salicylic acid is metabolized in the liver. Conjugation with glycine forms salicyluric acid and with glucuronic acid forms salicyl acyl and phenolic glucuronide. These metabolic pathways have only a limited capacity. Small amounts of salicylic acid are also hydroxylated to gentisic acid. With large salicylate doses, the kinetics switch from first order to zero order, as metabolic pathways become saturated and renal excretion becomes increasingly important.[63]
Salicylates are excreted mainly by the kidneys as salicyluric acid (75%), free salicylic acid (10%), salicylic phenol (10%) and acyl (5%) glucuronides, and gentisic acid (< 1%). When small doses (less than 250 mg in an adult) are ingested, all pathways proceed by first order kinetics, with an elimination half-life of about 2 to 4.5 hours.[64][65] When higher doses of salicylate are ingested (more than 4 g), the half-life becomes much longer (15–30 hours)[66] because the biotransformation pathways concerned with the formation of salicyluric acid and salicyl phenolic glucuronide become saturated.[67] Renal excretion of salicylic acid becomes increasingly important as the metabolic pathways become saturated, because it is extremely sensitive to changes in urinary pH. There is a 10 to 20 fold increase in renal clearance when urine pH is increased from 5 to 8. The use of urinary alkalinization exploits this particular aspect of salicylate elimination.[68]
Contraindications and resistance
Aspirin should not be taken by people who are allergic to ibuprofen or naproxen,[69][70] or to have salicylate intolerance[71][72] or a more generalized drug intolerance to NSAIDs, and caution should be exercised in those with asthma or NSAID-precipitated bronchospasm. Due to its effect on the stomach lining, manufacturers recommend that people with kidney disease, peptic ulcers, mild diabetes, gout or gastritis seek medical advice before using aspirin.[69][73] Even if none of these conditions are present, there is still an increased risk of stomach bleeding when aspirin is taken with alcohol or warfarin.[69][70] Patients with hemophilia or other bleeding tendencies should not take aspirin or other salicylates.[69][73] Aspirin is known to cause hemolytic anemia in people who have the genetic disease glucose-6-phosphate dehydrogenase deficiency (G6PD), particularly in large doses and depending on the severity of the disease.[74][75] Aspirin should not be given to children or adolescents to control cold or influenza symptoms as this has been linked with Reye's syndrome.[4] Use of aspirin during Dengue Fever is not recommended due to increased bleeding tendency.[76]
For some people, aspirin does not have as strong an effect on platelets as for others, an effect known as aspirin resistance or insensitivity. One study has suggested that women are more likely to be resistant than men[77] and a different, aggregate study of 2,930 patients found 28% to be resistant.[78] A study in 100 Italian patients found that of the apparent 31% aspirin resistant subjects, only 5% were truly resistant, and the others were non-compliant.[79]
Adverse effects
Gastrointestinal
Aspirin use has been shown to increase the risk of gastrointestinal bleeding.[80] Although some enteric coated formulations of aspirin are advertised as being "gentle to the stomach", in one study enteric coating did not seem to reduce this risk.[80] Combining aspirin with other NSAIDs has also been shown to further increase this risk.[80] Using aspirin in combination with clopidogrel or warfarin also increases the risk of upper GI bleeding.[81]
Central effects
Large doses of salicylate, a metabolite of aspirin, have been proposed to cause tinnitus, based on the experiments in rats, via the action on arachidonic acid and NMDA receptors cascade.[82]
Reye's syndrome
Reye's syndrome, a severe illness characterized by acute encephalopathy and fatty liver, can occur when children or adolescents are given aspirin for a fever or other illnesses or infections. From 1981 through 1997, 1207 cases of Reye's syndrome in under-18 patients were reported to the U.S. Centers for Disease Control and Prevention. Of these, 93% reported being ill in the three weeks preceding onset of Reye's syndrome, most commonly with a respiratory infection, chickenpox, or diarrhea. Salicylates were detectable in 81.9% of children for whom test results were reported.[83] After the association between Reye's syndrome and aspirin was reported and safety measures to prevent it (including a Surgeon General's warning and changes to the labeling of aspirin-containing drugs) were implemented, the number of reported cases of Reye's syndrome declined considerably in the United States, as did the use of aspirin in children; a similar decline was found in the United Kingdom after warnings against pediatric aspirin use were issued.[83] The U.S. Food and Drug Administration now recommends that aspirin (or aspirin-containing products) should not be given to anyone under the age of 19 who has a fever.[4]
Other effects
Aspirin can cause prolonged bleeding after operations for up to 10 days. In one study, thirty patients were observed after their various surgeries. Twenty of the thirty patients had to have an additional unplanned operation because of postoperative bleeding.[84] This diffuse bleeding was associated with aspirin alone or in combination with another NSAID in 19 out of the 20 who had to have another operation due to bleeding after their operation. The average recovery time for the second operation was 11 days.
Aspirin can induce angioedema in some people. In one study, angioedema appeared 1–6 hours after ingesting aspirin in some of the patients participating in the study. However, when the aspirin was taken alone it did not cause angioedema in these patients; the aspirin was either taken in combination with another NSAID-induced drug when angioedema appeared.[85]
Interactions
Aspirin is known to interact with other drugs. For example, acetazolamide and ammonium chloride have been known to enhance the intoxicating effect of salicyclates, and alcohol also enhances the gastrointestinal bleeding associated with these types of drugs as well.[69][70] Aspirin is known to displace a number of drugs from protein binding sites in the blood, including the anti-diabetic drugs tolbutamide and chlorpropamide, the immunosuppressant methotrexate, phenytoin, probenecid, valproic acid (as well as interfering with beta oxidation, an important part of valproate metabolism) and any nonsteroidal anti-inflammatory drug. Corticosteroids may also reduce the concentration of aspirin. The pharmacological activity of spironolactone may be reduced by taking aspirin, and aspirin is known to compete with Penicillin G for renal tubular secretion.[86] Aspirin may also inhibit the absorption of vitamin C.[87][88][89]
Dosage

For adults doses are generally taken four times a day for fever or arthritis,[90] with doses near the maximal daily dose used historically for the treatment of rheumatic fever.[91] For the prevention of myocardial infarction in someone with documented or suspected coronary artery disease, much lower doses are taken once daily.[90]
In children with Kawasaki disease, aspirin is taken at dosages based on body weight, initially four times a day for up to two weeks and then at a lower dose once daily for a further six to eight weeks.[92]
Overdose
Aspirin overdose can be acute or chronic. In acute poisoning, a single large dose is taken; in chronic poisoning, supratherapeutic doses are taken over a period of time. Acute overdose has a mortality rate of 2%. Chronic overdose is more commonly lethal with a mortality rate of 25%; chronic overdose may be especially severe in children.[93]
Symptoms
Aspirin overdose has potentially serious consequences, sometimes leading to significant morbidity and death. Patients with mild intoxication frequently have nausea and vomiting, abdominal pain, lethargy, tinnitus, and dizziness. More significant symptoms occur in more severe poisonings and include hyperthermia, tachypnea, respiratory alkalosis, metabolic acidosis, hyperkalemia, hypoglycemia, hallucinations, confusion, seizure, cerebral edema, and coma. The most common cause of death following an aspirin overdose is cardiopulmonary arrest usually due to pulmonary edema.[94]
Toxicity
The acutely toxic dose of aspirin is generally considered greater than 150 mg per kg of body mass.[66] Moderate toxicity occurs at doses up to 300 mg/kg, severe toxicity occurs between 300 to 500 mg/kg, and a potentially lethal dose is greater than 500 mg/kg.[95] Chronic toxicity may occur following doses of 100 mg/kg per day for two or more days.[95]
Treatment
All overdosed patients should be conveyed to a hospital for assessment immediately. Initial treatment of an acute overdose includes gastric decontamination by administering activated charcoal, which adsorbs the aspirin in the gastrointestinal tract. Stomach pumping is no longer routinely used in the treatment of poisonings but is sometimes considered if the patient has ingested a potentially lethal amount less than one hour before presentation.[96] Inducing vomitting with syrup of ipecac is not recommended.[66] Repeated doses of charcoal have been proposed to be beneficial in cases of aspirin overdosing,[97] although one study found that they might not be of significant value.[98] Regardless, most clinical toxicologists will administer additional charcoal if serum salicylate levels are increasing.
Patients are monitored until their peak salicylate blood level has been determined.[68] Blood levels are usually assessed four hours after ingestion and then every two hours after that to determine the maximum level. Maximum levels can be used as a guide to toxic effects expected.[99]
There is no antidote to salicylate poisoning. Monitoring of biochemical parameters such as electrolytes, liver and kidney function, urinalysis, and complete blood count is undertaken along with frequent checking of salicylate and blood sugar levels. Arterial blood gas assessments are performed to test for respiratory alkalosis and metabolic acidosis. Patients are monitored and often treated according to their individual symptoms. Patients may be given intravenous potassium chloride to counteract hypokalemia, glucose to restore blood sugar levels, benzodiazepines for any seizure activity, fluids for dehydration, and importantly sodium bicarbonate to restore the blood's sensitive pH balance. Sodium bicarbonate also has the effect of increasing the pH of urine, which in turn increases the elimination of salicylate. Additionally, hemodialysis can be implemented to enhance the removal of salicylate from the blood. Hemodialysis is usually used in severely poisoned patients; for example, patients with significantly high salicylate blood levels, significant neurotoxicity (agitation, coma, convulsions), renal failure, pulmonary edema, or cardiovascular instability are hemodialyzed.[68] Hemodialysis also has the advantage of restoring electrolyte and acid-base abnormalities while removing salicylate;[68] hemodialysis is often life-saving in severely ill patients.
Epidemiology
During the latter part of the 20th century, the number of poisonings from salicylates declined, mainly because of the increased popularity of other over-the-counter analgesics such as paracetamol (acetaminophen). Fifty-two deaths involving single-ingredient aspirin were reported in the United States in 2000; however, in all but three of these cases, the reason for the ingestion of lethal doses was intentional; predominantly suicidal.[100]
See also
- Aspergum
- Copper aspirinate
- Non-steroidal anti-inflammatory drug
- History of aspirin
- Salicylic acid
References
- ↑ Lewis, H D; J W Davis, D G Archibald, W E Steinke, T C Smitherman, J E Doherty, H W Schnaper, M M LeWinter, E Linares, J M Pouget, S C Sabharwal, E Chesler, H DeMots (1983-08-18). "Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study". The New England journal of medicine 309 (7): 396–403. ISSN 00284793.
- ↑ Julian, D G; D A Chamberlain, S J Pocock (1996-09-24). "A comparison of aspirin and anticoagulation following thrombolysis for myocardial infarction (the AFTER study): a multicentre unblinded randomised clinical trial". BMJ (British Medical Journal) 313 (7070): 1429–1431. PMID 8973228. http://www.bmj.com/cgi/content/full/313/7070/1429. Retrieved on 2007-10-04.
- ↑ Krumholz, Harlan M.; Martha J. Radford, Edward F. Ellerbeck, John Hennen, Thomas P. Meehan, Marcia Petrillo, Yun Wang, Timothy F. Kresowik, Stephen F. Jencks (1995-11-15). "Aspirin in the Treatment of Acute Myocardial Infarction in Elderly Medicare Beneficiaries : Patterns of Use and Outcomes". Circulation 92 (10): 2841–2847. PMID 7586250. http://circ.ahajournals.org/cgi/content/abstract/92/10/2841. Retrieved on 2008-05-15.
- ↑ 4.0 4.1 4.2 Macdonald S (2002). "Aspirin use to be banned in under 16 year olds". BMJ 325 (7371): 988. doi:. PMID 12411346.
- ↑ 5.0 5.1 "Cyclooxygenase-3 (COX-3): filling in the gaps toward a COX continuum?". Proc Natl Acad Sci U S a 99 (21): 13371–3. 2002-10-15. doi:. PMID 12374850. http://www.pnas.org/cgi/content/extract/99/21/13371. Retrieved on 2008-05-08.
- ↑ http://www.wordconstructions.com/articles/health/aspirin.html
- ↑ http://www.inta.org/index.php?option=com_content&task=view&id=202&Itemid=126&getcontent=5
- ↑ (German) Gerhardt C (1853). "Untersuchungen über die wasserfreien organischen Säuren". Annalen der Chemie und Pharmacie 87: 149–179. doi:.
- ↑ (German) von Gilm H (1859). "Acetylderivate der Phloretin- und Salicylsäure". Annalen der Chemie und Pharmacie 112 (2): 180–185. doi:.
- ↑ (German) Schröder, Prinzhorn, Kraut K (1869). "Uber Salicylverbindungen". Annalen der Chemie und Pharmacie 150 (1): 1–20. doi:.
- ↑ Jeffreys, Diarmuid (August 11, 2005). Aspirin: The Remarkable Story of a Wonder Drug. Bloomsbury USA. pp. 73. ISBN 1582346003.
- ↑ Ueber Aspirin. Pflügers Archiv : European journal of physiology, Volume: 84, Issue: 11-12 (March 1, 1901), pp: 527-546.
- ↑ Jeffreys, Aspirin, pp. 136–142 and 151-152
- ↑ http://www.history.com/this-day-in-history.do?action=VideoArticle&id=52415
- ↑ Jeffreys, Aspirin, pp. 212–217
- ↑ Jeffreys, Aspirin, pp. 226–231
- ↑ Jeffreys, Aspirin, pp. 267–269
- ↑ "Treaty of Versailles, Part X, Section IV, Article 298" Annex, Paragraph 5 (1919-06-28). Retrieved on 2008-10-25.
- ↑ Mehta, Aalok (2005-06-20). "Aspirin". Chemical & Engineering News 83 (25). http://pubs.acs.org/cen/coverstory/83/8325/8325aspirin.html. Retrieved on 2008-10-23.
- ↑ http://www.ul.ie/~childsp/CinA/Issue59/TOC43_Aspirin.htm
- ↑ CBE Style Manual Committee; Huth, Edward J. (1994). Scientific Style and Format: The CBE Manual for Authors, Editors, and Publishers. Cambridge University Press. pp. 164.
- ↑ http://www.aspirin.com/faq_en.html
- ↑ Cheng, Tsung O. (15 Nov 2007). "The History of Aspirin". Texas Heart Institute Journal 34 (3): 392–393. PMID 17948100. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1995051. Retrieved on 2008-10-23.
- ↑ Aukerman G, Knutson D, Miser WF (2002). "Management of the acute migraine headache". Am Fam Phys 66 (11): 2123–30. PMID 12484694. http://www.aafp.org/afp/20021201/2123.html.
- ↑ Addy, D P (1983-04-09). "Cold comfort for hot children". British Medical Journal (Clinical research ed.) 286 (6372).
- ↑ Barkin, Robert (November/December 2001). "Acetaminophen, Aspirin, or Ibuprofen in Combination Analgesic Products". American Journal of Therapeutics 8 (6): 433–42. doi:. http://www.americantherapeutics.com/pt/re/ajt/abstract.00045391-200111000-00008.htm;jsessionid=LbQGQ3kCysg2DRjQQ5FhndrgfbXyp1vcpSqhhSP7prKz48H611H5!1379360954!181195629!8091!-1. Retrieved on 2008-05-02.
- ↑ Krumholz, HM; Radford MJ, Ellerbeck EF, Hennen J, Meehan TP, Petrillo M, Wang Y, Kresowik TF, Jencks SF. (1995-11-15). "Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes" ( – Scholar search). Circulation 92 (10): 2841–7. PMID 7586250. http://circ.ahajournals.org/cgi/content/full/92/10/284. Retrieved on 2008-05-02.
- ↑ ISIS-2 Collaborative group (1988). "Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2". Lancet (2): 349–60. PMID 2899772.
- ↑ Belch J, MacCuish A, Campbell I, et al. (2008). "The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease". Br Med J 337: a1840. doi:.
- ↑ Hsieh KS, Weng KP, Lin CC, Huang TC, Lee CL, Huang SM (December 2004). "Treatment of acute Kawasaki disease: aspirin's role in the febrile stage revisited". Pediatrics 114 (6): e689–93. doi:. PMID 15545617. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=15545617.
- ↑ Chew EY, Williams GA, Burton TC, Barton FB, Remaley NA, Ferris FL (1992). "Aspirin effects on the development of cataracts in patients with diabetes mellitus. Early treatment diabetic retinopathy study report 16". Arch Ophthalmol 110 (3): 339–42. PMID 1543449.
- ↑ Bosetti, et al. (2006). "Aspirin and the risk of prostate cancer". Eur J Cancer Prev 15 (1): 43–5. doi:. PMID 16374228.
- ↑ Menezes, et al. (2006). "Regular use of aspirin and prostate cancer risk (United States)". Cancer Causes & Control 17 (3): 251–6. doi:. PMID 16489532.
- ↑ Schernhammer, et al. (2004). "A Prospective Study of Aspirin Use and the Risk of Pancreatic Cancer in Women". J Natl Cancer Inst 96 (1): 22–28. doi:. PMID 14709735. http://jnci.oxfordjournals.org/cgi/content/full/96/1/22.
- ↑ Larsson SC, Giovannucci E, Bergkvist L, Wolk A (December 2006). "Aspirin and nonsteroidal anti-inflammatory drug use and risk of pancreatic cancer: a meta-analysis". Cancer Epidemiol. Biomarkers Prev. 15 (12): 2561–4. doi:. PMID 17164387. http://cebp.aacrjournals.org/cgi/content/full/15/12/2561.
- ↑ Thun MJ, Namboodiri MM, Heath CW (1991). "Aspirin use and reduced risk of fatal colon cancer". N Engl J Med 325 (23): 1593–6. PMID 1669840.
- ↑ Baron, et al. (2003). "A randomized trial of aspirin to prevent colorectal adenomas". N Engl J Med 348 (10): 891–9. doi:. PMID 12621133.
- ↑ Chan, et al. (2004). "A Prospective Study of Aspirin Use and the Risk for Colorectal Adenoma". Ann Intern Med 140 (3): 157–66. PMID 14757613.
- ↑ Chan, et al. (2005). "Long-term Use of Aspirin and Nonsteroidal Anti-inflammatory Drugs and Risk of Colorectal Cancer". JAMA 294 (8): 914–23. doi:. PMID 16118381.
- ↑ Akhmedkhanov, et al. (2002). "Aspirin and lung cancer in women". Br J cancer 87 (11): 1337–8. doi:. PMID 12085255.
- ↑ Moysich KB, Menezes RJ, Ronsani A, et al (2002). "Regular aspirin use and lung cancer risk". BMC Cancer 2: 31. doi:. PMID 12453317. Free full text
- ↑ 42.0 42.1 "Regular aspirin use and esophageal cancer risk". Int J Cancer 119 (1): 202–7. 2006-07-01. doi:. PMID 16450404.
- ↑ Bosetti, et al. (2003). "Aspirin use and cancers of the upper aerodigestive tract". Br J Cancer 88 (5): 672–74. doi:. PMID 12618872.
- ↑ Wolff, et al. (15 Nov 1998). "Expression of cyclooxygenase-2 in human lung carcinoma". Cancer Research 58 (22): 4997–5001. PMID 9823297. http://cancerres.aacrjournals.org/cgi/content/abstract/58/22/4997.
- ↑ Crosby, Janet Tobiassen (2006). "Veterinary Questions and Answers". About.com. Retrieved on 2007-09-05.
- ↑ Cambridge H, Lees P, Hooke RE, Russell CS (1991). "Antithrombotic actions of aspirin in the horse". Equine Vet J 23 (2): 123–7. PMID 1904347.
- ↑ John Robert Vane (1971). "Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs". Nature - New Biology 231 (25): 232–5. PMID 5284360.
- ↑ Vane JR, Botting RM (June 2003). "The mechanism of action of aspirin" (PDF). Thromb Res 110 (5-6): 255–8. doi:. PMID 14592543. http://www.eao.chups.jussieu.fr/polys/certifopt/saule_coxib/theme/1vane2003.pdf.
- ↑ "Aspirin in Heart Attack and Stroke Prevention". American Heart Association. Retrieved on 2008-05-08.
- ↑ Tohgi, H; S Konno, K Tamura, B Kimura and K Kawano (1992). "Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin". Stroke Vol 23: 1400–1403. PMID 1412574.
- ↑ Somasundaram, S. et al. (2000). "Uncoupling of intestinal mitochondrial oxidative phosphorylation and inhibition of cyclooxygenase are required for the development of NSAID-enteropathy in the rat". Aliment Pharmacol Ther 14: 639–650. doi:10.1046/j.1365-2036.2000.00723.x (inactive 2008-06-24). http://www.blackwell-synergy.com/doi/pdf/10.1046/j.1365-2036.2000.00723.x. Retrieved on 2008-05-28.
- ↑ Mark J. Paul-Clark, Thong van Cao, Niloufar Moradi-Bidhendi, Dianne Cooper, and Derek W. Gilroy 15-epi-lipoxin A4–mediated Induction of Nitric Oxide Explains How Aspirin Inhibits Acute Inflammation J. Exp. Med. 200: 69-78; published online before print as 10.1084/jem.20040566
- ↑ McCarty, MF; KI Block (2006). "Preadministration of high-dose salicylates, suppressors of NF-kappaB activation, may increase the chemosensitivity of many cancers: an example of proapoptotic signal modulation therapy". Integr Cancer Ther. Vol 5 (3): 252–268. doi:. PMID 16880431.
- ↑ Reynolds EF (ed) (1982). Aspirin and similar analgesic and anti-inflammatory agents. Martindale, The Extra Pharmacopoeia 28 Ed, 234-82.
- ↑ Palleros, Daniel R. (2000). Experimental Organic Chemistry. New York: John Wiley & Sons. pp. 494. ISBN 0-471-28250-2.
- ↑ Barrans, Richard. "Aspirin Aging". Newton BBS. Retrieved on 2008-05-08.
- ↑ Carstensen, J.T.; F Attarchi and XP Hou (July 1985). "Decomposition of aspirin in the solid state in the presence of limited amounts of moisture". Journal of Pharmaceutical Sciences 77 (4): 318–21. doi:. PMID 4032246.
- ↑ "Acetylsalicylic acid". Jinno Laboratory, School of Materials Science, Toyohashi University of Technology (March 1, 1996). Retrieved on 2007-09-07.
- ↑ Peddy Vishweshwar, Jennifer A. McMahon, Mark Oliveira, Matthew L. Peterson, and Michael J. Zaworotko (2005). "The Predictably Elusive Form II of Aspirin". J. Am. Chem. Soc. 127 (48): 16802–16803. doi:.
- ↑ Andrew D. Bond, Roland Boese, Gautam R. Desiraju (2007). "On the Polymorphism of Aspirin: Crystalline Aspirin as Intergrowths of Two "Polymorphic" Domains". Angewandte Chemie International Edition 46 (4): 618–622. doi:.
- ↑ Ferguson, RK; Boutros, AR (1970-08-17). "Death following self-poisoning with aspirin". Journal of the American Medical Association. PMID 5468267.
- ↑ Kaufman, FL; Dubansky, AS (1970-04). "Darvon poisoning with delayed salicylism: a case report". Pediatrics 49 (4): 610–1. PMID 5013423.
- ↑ 63.0 63.1 63.2 Levy, G; Tsuchiya, T (1972-09-31). "Salicylate accumulation kinetics in man". New England Journal of Medicine 287 (9): 430–2. PMID 5044917.
- ↑ Hartwig, Otto H (1983-11-14). "Pharmacokinetic considerations of common analgesics and antipyretics". American Journal of Medicine 75 (5A): 30–7. doi:. PMID 6606362.
- ↑ Done, AK (1960-11). "Salicylate intoxication. Significance of measurements of salicylate in blood in cases of acute ingestion". Pediatrics: 800–7. PMID 13723722.
- ↑ 66.0 66.1 66.2 Chyka PA, Erdman AR, Christianson G, Wax PM, Booze LL, Manoguerra AS, Caravati EM, Nelson LS, Olson KR, Cobaugh DJ, Scharman EJ, Woolf AD, Troutman WG; Americal Association of Poison Control Centers; Healthcare Systems Bureau, Health Resources and Services Administration, Department of Health and Human Services. (2007). "Salicylate poisoning: an evidence-based consensus guideline for out-of-hospital management". Clin Toxicol (Phila) 45 (2): 95–131. doi:. PMID 17364628.
- ↑ Prescott LF, Balali-Mood M, Critchley JA, Johnstone AF, Proudfoot AT (November 1982). "Diuresis or urinary alkalinisation for salicylate poisoning?". Br Med J (Clin Res Ed) 285 (6352): 1383–6. PMID 6291695.
- ↑ 68.0 68.1 68.2 68.3 Dargan PI, Wallace CI, Jones AL. (2002). "An evidenced based flowchart to guide the management of acute salicylate (aspirin) overdose". Emerg Med J 19 (3): 206–9. doi:. PMID 11971828.
- ↑ 69.0 69.1 69.2 69.3 69.4 "Aspirin information from Drugs.com". Drugs.com. Retrieved on 2008-05-08.
- ↑ 70.0 70.1 70.2 "Oral Aspirin information". First DataBank. Retrieved on 2008-05-08.
- ↑ Raithel M, Baenkler HW, Naegel A, et al (September 2005). "Significance of salicylate intolerance in diseases of the lower gastrointestinal tract" (PDF). J. Physiol. Pharmacol. 56 Suppl 5: 89–102. PMID 16247191. http://www.jpp.krakow.pl/journal/archive/0905_s5/pdf/89_0905_s5_article.pdf.
- ↑ Senna GE, Andri G, Dama AR, Mezzelani P, Andri L (1995). "Tolerability of imidazole salycilate in aspirin-sensitive patients". Allergy Proc 16 (5): 251–4. doi:. PMID 8566739. http://openurl.ingenta.com/content/nlm?genre=article&issn=1088-5412&volume=16&issue=5&spage=251&aulast=Senna.
- ↑ 73.0 73.1 PDR Guide to Over the Counter (OTC) Drugs, http://www.mercksource.com/pp/us/cns/cns_hl_pdr.jspzQzpgzEzzSzppdocszSzuszSzcnszSzcontentzSzpdrotczSzotc_fullzSzdrugszSzfgotc036zPzhtm, retrieved on 2008-04-28.
- ↑ G6PD (Glucose-6-Phosphate Dehydrogenase) Deficiency, University of Virginia, http://www.healthsystem.virginia.edu/uvahealth/adult_blood/glucose.cfm, retrieved on 2008-05-07
- ↑ G6PD (Glucose-6-Phosphate Dehydrogenase) Deficiency, University of Texas Medical Branch, http://www.utmbhealthcare.org/Health/Content.asp?PageID=P00091, retrieved on 2008-05-07
- ↑ Dengue and Dengue Hemorrhagic Fever: Information for Health Care Practitioners, http://www.cdc.gov/NCIDOD/dvbid/dengue/dengue-hcp.htm, retrieved on 2008-04-28
- ↑ Dorsch MP, Lee JS, Lynch DR, Dunn SP, Rodgers JE, Schwartz T, Colby E, Montague D, Smyth SS (24 Apr 2007). "Aspirin Resistance in Patients with Stable Coronary Artery Disease with and without a History of Myocardial Infarction". Ann Pharmacother 41 (May): 737. doi:. PMID 17456544.
- ↑ Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (January 2008). "Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis". BMJ 336 (7637): 195–8. doi:. PMID 18202034. PMC: 2213873. http://bmj.com/cgi/pmidlookup?view=long&pmid=18202034.
- ↑ Pignatelli P, Di Santo S, Barillà F, Gaudio C, Violi F (October 2008). "Multiple anti-atherosclerotic treatments impair aspirin compliance: effects on aspirin resistance". J. Thromb. Haemost. 6 (10): 1832–4. doi:. PMID 18680540.
- ↑ 80.0 80.1 80.2 Sørensen HT, Mellemkjaer L, Blot WJ, et al (September 2000). "Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin". Am. J. Gastroenterol. 95 (9): 2218–24. doi:. PMID 11007221. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0002-9270&date=2000&volume=95&issue=9&spage=2218.
- ↑ Delaney JA, Opatrny L, Brophy JM & Suissa S (August 2007). "Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding". CMAJ 177 (4): 347–51. doi:. PMID 17698822.
- ↑ Guitton MJ, Caston J, Ruel J, Johnson RM, Pujol R, Puel JL (May 2003). "Salicylate induces tinnitus through activation of cochlear NMDA receptors". J. Neurosci. 23 (9): 3944–52. PMID 12736364. http://www.jneurosci.org/cgi/content/full/23/9/3944.
- ↑ 83.0 83.1 Belay ED, Bresee JS, Holman RC, Khan AS, Shahriari A, Schonberger LB (May 1999). "Reye's syndrome in the United States from 1981 through 1997". N. Engl. J. Med. 340 (18): 1377–82. PMID 10228187. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=10228187&promo=ONFLNS19.
- ↑ Scher, K.S. (January 1996). "Unplanned reoperation for bleeding". Am Surg 62 (1): 52–55. PMID 8540646.
- ↑ Berges-Gimeno MP & Stevenson DD (June 2004). "Nonsteroidal anti-inflammatory drug-induced reactions and desensitization". J Asthma 41 (4): 375–84. doi:. PMID 15281324.
- ↑ Katzung (1998), p. 584.
- ↑ Loh HS, Watters K & Wilson CW (01 Nov 1973). "The Effects of Aspirin on the Metabolic Availability of Ascorbic Acid in Human Beings". J Clin Pharmacol 13 (11): 480–6. PMID 4490672. http://jcp.sagepub.com/cgi/content/abstract/13/11/480.
- ↑ Basu TK (1982). "Vitamin C-aspirin interactions". Int J Vitam Nutr Res Suppl 23: 83–90. PMID 6811490.
- ↑ Ioannides C, Stone AN, Breacker PJ & Basu TK (December 1982). "Impairment of absorption of ascorbic acid following ingestion of aspirin in guinea pigs". Biochem Pharmacol 31 (24): 4035–8. doi:. PMID 6818974.
- ↑ 90.0 90.1 British National Formulary (45 ed.). British Medical Journal and Royal Pharmaceutical Society of Great Britain. March 2003.
- ↑ Aspirin monograph: dosages, etc
- ↑ British National Formulary for Children. British Medical Journal and Royal Pharmaceutical Society of Great Britain. 2006.
- ↑ Gaudreault P, Temple AR, Lovejoy FH Jr. (1982). "The relative severity of acute versus chronic salicylate poisoning in children: a clinical comparison". Pediatrics 70 (4): 566–9. PMID 7122154.
- ↑ Thisted B, Krantz T, Stroom J, Sorensen MB. (1987). "Acute salicylate self-poisoning in 177 consecutive patients treated in ICU". Acta Anaesthesiol Scand 31 (4): 312–6. PMID 3591255.
- ↑ 95.0 95.1 Temple AR. (1981). "Acute and chronic effects of aspirin toxicity and their treatment". Arch Intern Med 141 (3 Spec No): 364–9. doi:. PMID 7469627.
- ↑ Vale JA, Kulig K; American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. (2004). "Position paper: gastric lavage". J Toxicol Clin Toxicol 42 (7): 933–43. doi:. PMID 15641639.
- ↑ Hillman RJ, Prescott LF. (1985). "Treatment of salicylate poisoning with repeated oral charcoal". Br Med J (Clin Res Ed) 291 (6507): 1472. PMID 3933714.
- ↑ Kirshenbaum LA, Mathews SC, Sitar DS, Tenenbein M. (1990). "Does multiple-dose charcoal therapy enhance salicylate excretion?". Arch Intern Med 150 (6): 1281–3. doi:. PMID 2191636.
- ↑ Meredith TJ, Vale JA. (1986). "Non-narcotic analgesics. Problems of overdosage". Drugs 32 (Suppl 4): 117–205. doi:. PMID 3552583.
- ↑ Litovitz TL, Klein-Schwartz W, White S, Cobaugh DJ, Youniss J, Omslaer JC, Drab A, Benson BE (2001). "2000 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System". Am J Emerg Med 19 (5): 337–95. doi:. PMID 11555795.
External links
- NextBio Aspirin Entry
- Colour-enhanced scanning electron micrograph of aspirin crystals
- The History of Aspirin
- How Aspirin works
- The science behind aspirin
- Take two: Aspirin, New uses and new dangers are still being discovered as aspirin enters its second century. Shauna Roberts, American Chemical Society
- Ling, Greg (2005). "Aspirin". How Products are Made 1. Thomson Gale.
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||