Antihypertensive
Antihypertensives are a class of drugs that are used in medicine and pharmacology to treat hypertension (high blood pressure). There are many classes of antihypertensives, which—by varying means—act by lowering blood pressure. Evidence suggests that reduction of the blood pressure by 5-6 mmHg can decrease the risk of stroke by 40%, of coronary heart disease by 15-20%, and reduces the likelihood of dementia, heart failure, and mortality from cardiovascular disease.
Which type of medication to use initially for hypertension has been the subject of several large studies and resulting national guidelines.The fundamental goal of treatment should be the prevention of the important "endpoints" of hypertension such as heart attack, stroke and heart failure. Several classes of medications are effective in reducing blood pressure. However, these classes differ in side effect profiles, ability to prevent endpoints, and cost. The choice of more expensive agents, where cheaper ones would be equally effective, may have negative impacts on national healthcare budgets.[1]
In the United States, the JNC7 (The Seventh Report of the Joint National Committee on Prevention of Detection, Evaluation and Treatment of High Blood Pressure) recommends starting with a thiazide diuretic if single therapy is being initiated and another medication is not indicated.[2] This is based on a slightly better outcome for chlortalidone in the ALLHAT study versus other anti-hypertensives and because thiazide diuretics are relatively cheap.[3] A subsequent smaller study (ANBP2) published after the JNC7 did not show this small difference in outcome and actually showed a slightly better outcome for ACE-inhibitors in older male patients.[4]
Despite thiazides being cheap, effective, and recommended as the best first-line drug for hypertension by many experts, they are not prescribed as often as some newer drugs. Arguably, this is because they are off-patent and thus rarely promoted by the drug industry.[5]
In the United Kingdom, the June 2006 "Hypertension: management of hypertension in adults in primary care"[6] guideline of the National Institute for Health and Clinical Excellence, downgraded the role of beta-blockers due to their risk of provoking type 2 diabetes.[7]
Contents |
Available drugs
Diuretics
Diuretics help the kidneys eliminate excess salt and water from the body's tissues and blood.
- Loop diuretics:
- bumetanide
- ethacrynic acid
- furosemide
- torsemide
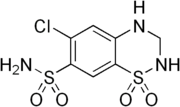
- Thiazide diuretics:
- chlortalidone
- epitizide
- hydrochlorothiazide and chlorothiazide
- bendroflumethiazide
- Thiazide-like diuretics:
- indapamide
- chlorthalidone
- metolazone
- Potassium-sparing diuretics:
- amiloride
- triamterene
- spironolactone
Only the thiazide and thiazide-like diuretics have good evidence of beneficial effects on important endpoints of hypertension, and hence, should usually be the 1st choice when selecting a diuretic to treat hypertension. The reason why thiazides-type diuretics are better than the others is (at least in part) thought to be because of their vasodilating properties.
Although the diuretic effect of thiazides may be apparent shortly after administration, it takes longer (weeks of treatment) for the full anti-hypertensive effect to develop.
Adrenergic receptor antagonists

- Beta blockers (no longer 1st line therapy in many countries - see Lancet 29 October 2005):
- atenolol
- metoprolol
- nadolol
- oxprenolol
- pindolol
- propranolol
- timolol
- Alpha blockers:
- doxazosin
- phentolamine
- indoramin
- phenoxybenzamine
- prazosin
- terazosin
- tolazoline
- Mixed Alpha + Beta blockers:
- bucindolol
- carvedilol
- labetalol
Although beta blockers lower blood pressure, they do not have as positive a benefit on endpoints as some other antihypertensives.[8] In particular, atenolol seems to be less useful in hypertension than several other agents.[9] However, beta blockers have an important role in the prevention of heart attack in people who have already had a heart attack.[10]
Despite lowering blood pressure, alpha blockers have significantly poorer endpoint outcomes than other antihypertensives, and are no longer recommended as a first-line choice in the treatment of hypertension.[11] However, they may be useful for some men with symptoms of prostate disease.
Adrenergic receptor agonist
- Alpha-2 agonists:
- clonidine
- methyldopa
- Guanfacine
Calcium channel blockers
Calcium channel blockers block the entry of calcium into muscle cells in artery walls.
- dihydropyridines:
- amlodipine
- felodipine
- isradipine
- lercanidipine
- nicardipine
- nifedipine
- nimodipine
- nitrendipine
- non-dihydropyridines:
- diltiazem
- verapamil
ACE inhibitors

ACE inhibitors inhibit the activity of Angiotensin-converting enzyme (ACE), an enzyme responsible for the conversion of angiotensin I into angiotensin II, a potent vasoconstrictor.
- captopril
- enalapril
- fosinopril
- lisinopril
- perindopril
- quinapril
- ramipril
- trandolapril
- benazepril
Angiotensin II receptor antagonists

Angiotensin II receptor antagonists work by antagonizing the activation of angiotensin receptors.
- candesartan
- eprosartan
- irbesartan
- losartan
- olmesartan
- telmisartan
- valsartan
Aldosterone antagonists
Aldosterone receptor antagonists:
- eplerenone
- spironolactone
Aldosterone antagonists are not recommended as first-line agents for blood pressure,[2] but spironolactone and eplerenone are both used in the treatment of heart failure.
Vasodilators
Vasodilators act directly on arteries to relax their walls so blood can move more easily through them; they are only used in medical emergencies.
- sodium nitroprusside
Centrally acting adrenergic drugs
Central alpha agonists lower blood pressure by stimulating alpha-receptors in the brain which open peripheral arteries easing blood flow. Central alpha agonists, such as clonidine, are usually prescribed when all other anti-hypertensive medications have failed. For treating hypertension, these drugs are usually administered in combination with a diuretic.
- Clonidine
- Guanabenz
- Methyldopa
- Moxonidine
Adverse effects of this class of drugs include sedation, drying of the nasal mucosa and rebound hypertension.
Some adrenergic neuron blockers are used for the most resistant forms of hypertension:
- Guanethidine
- Reserpine
Future treatment options
Blood pressure vaccine
Blood pressure vaccinations are being trialed and may become a treatment option for high blood pressure in the future. Research on the vaccine CYT006-AngQb published in The Lancet on the 8 March 2008 titled, “Vaccination against high blood pressure: a new strategy” showed patients experienced a drop in systolic and diastolic blood pressure after taking the vaccine. Effective blood pressure vaccines would assist those people who forget to take their medication. It would also help those who stop taking their medication due to side effects or falsely believing they don't need them anymore once their blood pressure is lowered.[12]
Choice
The choice between the drugs is to a large degree determined by the characteristics of the patient being prescribed for, the drugs' side-effects, and cost. For example, asthmatics have been reported to have worsening symptoms when using beta blockers. Most drugs have other uses; sometimes the presence of other symptoms can warrant the use of one particular antihypertensive (such as beta blockers in case of tremor and nervousness, and alpha blockers in case of benign prostatic hyperplasia). The JNC 7 report outlines compelling reasons to choose one drug over the others for certain individual patients.[2]
See also
- Blood pressure
- Hypertension
- Prehypertension
- Pulse pressure
References
- ↑ Nelson MR, McNeil JJ, Peeters A et al (Jun 4 2001). "PBS/RPBS cost implications of trends and guideline recommendations in the pharmacological management of hypertension in Australia, 1994-1998". Med J Aust 174 (11): 565–8. PMID 11453328.
- ↑ 2.0 2.1 2.2 Chobanian AV et al (2003). "The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report". JAMA 289: 2560–72. doi:. PMID 12748199. http://jama.ama-assn.org/cgi/content/full/289.19.2560v1.
- ↑ ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (Dec 18 2002). "Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)". JAMA 288 (23): 2981–97. doi:. PMID 12479763. http://jama.ama-assn.org/cgi/content/full/288/23/2981.
- ↑ Wing LM, Reid CM, Ryan P et al (Feb 13 2003). "A comparison of outcomes with angiotensin-converting--enzyme inhibitors and diuretics for hypertension in the elderly". NEJM 348 (7): 583–92. doi:. PMID 12584366.
- ↑ Wang TJ, Ausiello JC, Stafford RS (1999). "Trends in Antihypertensive Drug Advertising, 1985–1996". Circulation 99: 2055–2057. PMID 10209012. http://circ.ahajournals.org/cgi/content/full/99/15/2055.
- ↑ "Hypertension: management of hypertension in adults in primary care" (PDF). National Institute for Health and Clinical Excellence. Retrieved on 2006-09-30.
- ↑ Sheetal Ladva (2006-06-28). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Retrieved on 2006-09-30.
- ↑ Lindholm LH, Carlberg B, Samuelsson O (Oct 29-Nov 4 2005). "Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis". Lancet 366 (9496): 1545–53. doi:. PMID 16257341.
- ↑ Carlberg B, Samuelsson O, Lindholm LH (Nov 6-12 2004). "Atenolol in hypertension: is it a wise choice?". Lancet 364 (9446): 1684–9. doi:. PMID 15530629.
- ↑ Freemantle N, Cleland J, Young P et al (Jun 26 1999). "Beta Blockade after myocardial infarction: systematic review and meta regression analysis". BMJ 318 (7200): 1730–7. PMID 10381708. http://bmj.bmjjournals.com/cgi/content/full/318/7200/1730.
- ↑ ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (September 2003). "Diuretic Versus alpha-Blocker as First-Step Antihypertensive Therapy". Hypertension 42 (3): 239–46. doi:. PMID 12925554. http://hyper.ahajournals.org/cgi/content/full/42/3/239.
- ↑ http://www.my-blood-pressure.com/vaccine-study.html Blood pressure vaccine study promising
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||