Anemia
| Anemia Classification and external resources |
|
 |
|
|---|---|
| ICD-10 | D50.-D64. |
| ICD-9 | 280-285 |
| DiseasesDB | 663 |
| MedlinePlus | 000560 |
| eMedicine | med/132 emerg/808 emerg/734 |
| MeSH | D000740 |
Anemia (AmE) or anæmia/anaemia (BrE) (from the Ancient Greek Ἀναιμία anaîmia, meaning “without blood”) is defined as a qualitative or quantitative deficiency of hemoglobin, a molecule found inside red blood cells (RBCs). Since hemoglobin normally carries oxygen from the lungs to the tissues, anemia leads to hypoxia (lack of oxygen) in organs. Since all human cells depend on oxygen for survival, varying degrees of anemia can have a wide range of clinical consequences. Anemia is also caused by a lack of iron in the body.
The three main classes of anemia include excessive blood loss (acutely such as a hemorrhage or chronically through low-volume loss), excessive blood cell destruction (hemolysis) or deficient red blood cell production (ineffective hematopoiesis).
Anemia is the most common disorder of the blood. There are several kinds of anemia, produced by a variety of underlying causes. Anemia can be classified in a variety of ways, based on the morphology of RBCs, underlying etiologic mechanisms, and discernible clinical spectra, to mention a few.
There are two major approaches of classifying anemias, the "kinetic" approach which involves evaluating production, destruction and loss[1], and the "morphologic" approach which groups anemia by red blood cell size. The morphologic approach uses a quickly available and cheap lab test as its starting point (the MCV). On the other hand, focusing early on the question of production may allow the clinician more rapidly to expose cases where multiple causes of anemia coexist.
Contents |
Signs and symptoms
Anemia goes undetected in many people, and symptoms can be small and vague. Most commonly, people with anemia report a feeling of weakness or fatigue in general or during exercise, general malaise and sometimes poor concentration. People with more severe anemia often report dyspnea (shortness of breath) on exertion. Very severe anemia prompts the body to compensate by increasing cardiac output, leading to palpitations and sweatiness, and to heart failure.
Pallor (pale skin, mucosal linings and nail beds) is often a useful diagnostic sign in moderate or severe anemia, but it is not always apparent. Other useful signs are cheilosis and koilonychia.
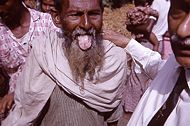
Pica, the consumption of non-food based items such as dirt, paper, wax, grass, ice, and hair, may be a symptom of iron deficiency, although it occurs often in those who have normal levels of hemoglobin.
Chronic anemia may result in behavioral disturbances in children as a direct result of impaired neurological development in infants, and reduced scholastic performance in children of school age.
Diagnosis
Generally, clinicians request complete blood counts in the first batch of blood tests in the diagnosis of an anemia. Apart from reporting the number of red blood cells and the hemoglobin level, the automatic counters also measure the size of the red blood cells by flow cytometry, which is an important tool in distinguishing between the causes of anemia. Examination of a stained blood smear using a microscope can also be helpful, and is sometimes a necessity in regions of the world where automated analysis is less accessible.
In modern counters, four parameters (RBC count, hemoglobin concentration, MCV and RDW) are measured, allowing others (hematocrit, MCH and MCHC) to be calculated, and compared to values adjusted for age and sex. Some counters estimate hematocrit from direct measurements. For adult men, a hemoglobin level less than 13.0 g/dl (grams per deciliter) is diagnostic of anemia, and for adult women, the diagnostic threshold is below 12.0 g/dl.
Reticulocyte counts, and the "kinetic" approach to anemia, have become more common than in the past in the large medical centers of the United States and some other wealthy nations, in part because some automatic counters now have the capacity to include reticulocyte counts. A reticulocyte count is a quantitative measure of the bone marrow's production of new red blood cells. The reticulocyte production index is a calculation of the ratio between the level of anemia and the extent to which the reticulocyte count has risen in response. If the degree of anemia is significant, even a "normal" reticulocyte count actually may reflect an inadequate response.
If an automated count is not available, a reticulocyte count can be done manually following special staining of the blood film. In manual examination, activity of the bone marrow can also be gauged qualitatively by subtle changes in the numbers and the morphology of young RBCs by examination under a microscope. Newly formed RBCs are usually slightly larger than older RBCs and show polychromasia. Even where the source of blood loss is obvious, evaluation of erythropoiesis can help assess whether the bone marrow will be able to compensate for the loss, and at what rate.
When the cause is not obvious, clinicians use other tests: ESR, ferritin, serum iron, transferrin, RBC folate level, serum vitamin B12, hemoglobin electrophoresis, renal function tests (e.g. serum creatinine).
When the diagnosis remains difficult, a bone marrow examination allows direct examination of the precursors to red cells.
Classification
Production vs. destruction or loss
The "kinetic" approach to anemia yields what many argue is the most clinically relevant classification of anemia. This classification depends on evaluation of several hematological parameters, particularly the blood reticulocyte (precursor of mature RBCs) count. This then yields the classification of defects by decreased RBC production versus increased RBC destruction and/or loss. Clinical signs of loss or destruction include abnormal peripheral blood smear with signs of hemolysis; elevated LDH suggesting cell destruction; or clinical signs of bleeding, such as guiaic-positive stool, radiographic findings, or frank bleeding.
Here is a simplified schematic of this approach:
|
|
|
|
|
|
|
|
|
Anemia |
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||
|
|
|
|
|
|
Reticulocyte production index shows inadequate production response to anemia. |
|
|
|
Reticulocyte production index shows appropriate response to anemia = ongoing hemolysis or blood loss without RBC production problem. |
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
|
No clinical findings consistent with hemolysis or blood loss: pure disorder of production. |
|
Clinical findings and abnormal MCV: hemolysis or loss and chronic disorder of production*. |
|
Clinical findings and normal MCV= acute hemolysis or loss without adequate time for bone marrow production to compensate**. |
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
| Macrocytic anemia (MCV>100) |
|
Normocytic anemia (80<MCV<100) |
|
|
Microcytic anemia (MCV<80) |
|
|
|
|
||||||||||||||||||||||||||
* For instance, sickle cell anemia with superimposed iron deficiency; chronic gastric bleeding with B12 and folate deficiency; and other instances of anemia with more than one cause. ** Confirm by repeating reticulocyte count: ongoing combination of low reticulocyte production index, normal MCV and hemolysis or loss may be seen in bone marrow failure or anemia of chronic disease, with superimposed or related hemolysis or blood loss.
Red blood cell size
In the morphological approach, anemia is classified by the size of red blood cells; this is either done automatically or on microscopic examination of a peripheral blood smear. The size is reflected in the mean corpuscular volume (MCV). If the cells are smaller than normal (under 80 fl), the anemia is said to be microcytic; if they are normal size (80-100 fl), normocytic; and if they are larger than normal (over 100 fl), the anemia is classified as macrocytic. This scheme quickly exposes some of the most common causes of anemia; for instance, a microcytic anemia is often the result of iron deficiency. In clinical workup, the MCV will be one of the first pieces of information available; so even among clinicians who consider the "kinetic" approach more useful philosophically, morphology will remain an important element of classification and diagnosis.
Here is a schematic representation of how to consider anemia with MCV as the starting point:
|
|
|
|
|
|
|
|
|
|
|
|
Anemia |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
Macrocytic anemia (MCV>100) |
|
|
|
|
|
Normocytic anemia (80<MCV<100) |
|
|
|
|
|
Microcytic anemia (MCV<80) | ||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
High reticulocyte count |
|
|
|
|
|
Low reticulocyte count |
|
|
|
|
||||||||||||||||||||||||||||
Other characteristics visible on the peripheral smear may provide valuable clues about a more specific diagnosis; for example, abnormal white blood cells may point to a cause in the bone marrow.
Microcytic anemia
Microcytic anemia is primarily a result of hemoglobin synthesis failure/insufficiency, which could be caused by several etiologies:
- Heme synthesis defect
- Iron deficiency anemia
- Anemia of chronic disease (more commonly presenting as normocytic anemia)
- Globin synthesis defect
- alpha-, and beta-thalassemia
- HbE syndrome
- HbC syndrome
- and various other unstable hemoglobin diseases
- Sideroblastic defect
- Hereditary sideroblastic anemia
- Acquired sideroblastic anemia, including lead toxicity
- Reversible sideroblastic anemia
Iron deficiency anemia is the most common type of anemia overall and it has many causes. RBCs often appear hypochromic (paler than usual) and microcytic (smaller than usual) when viewed with a microscope.
- Iron deficiency anemia is caused by insufficient dietary intake or absorption of iron to replace losses from menstruation or losses due to diseases.[2] Iron is an essential part of hemoglobin, and low iron levels result in decreased incorporation of hemoglobin into red blood cells. In the United States, 20% of all women of childbearing age have iron deficiency anemia, compared with only 2% of adult men. The principal cause of iron deficiency anemia in premenopausal women is blood lost during menses. Studies have shown that iron deficiency without anemia causes poor school performance and lower IQ in teenage girls. Iron deficiency is the most prevalent deficiency state on a worldwide basis. Iron deficiency is sometimes the cause of abnormal fissuring of the angular (corner) sections of the lips (angular stomatitis).
- Iron deficiency anemia can also be due to bleeding lesions of the gastrointestinal tract. Fecal occult blood testing, upper endoscopy and lower endoscopy should be performed to identify bleeding lesions. In men and post-menopausal women the chances are higher that bleeding from the gastrointestinal tract could be due to colon polyp or colorectal cancer.
- Worldwide, the most common cause of iron deficiency anemia is parasitic infestation (hookworm, amebiasis, schistosomiasis and whipworm).[3]
Macrocytic anemia
- Megaloblastic anemia, the most common cause of macrocytic anemia, is due to a deficiency of either vitamin B12, folic acid (or both). Deficiency in folate and/or vitamin B12 can be due either to inadequate intake or insufficient absorption. Folate deficiency normally does not produce neurological symptoms, while B12 deficiency does.
- Pernicious anemia is caused by a lack of intrinsic factor. Intrinsic factor is required to absorb vitamin B12 from food. A lack of intrinsic factor may arise from an autoimmune condition targeting the parietal cells (atrophic gastritis) that produce intrinsic factor or against intrinsic factor itself. These lead to poor absorption of vitamin B12.
- Macrocytic anemia can also be caused by removal of the functional portion of the stomach, such as during gastric bypass surgery, leading to reduced vit B12/folate absorption. Therefore one must always be aware of anemia following this procedure.
- Hypothyroidism
- Alcoholism commonly causes a macrocytosis, although not specifically anemia. Other types of Liver Disease can also cause macrocytosis.
- Methotrexate, zidovudine, and other drugs that inhibit DNA replication.
Macrocytic anemia can be further divided into "megaloblastic anemia" or "non-megaloblastic macrocytic anemia". The cause of megaloblastic anemia is primarily a failure of DNA synthesis with preserved RNA synthesis, which result in restricted cell division of the progenitor cells. The megaloblastic anemias often present with neutrophil hypersegmentation (6-10 lobes). The non-megaloblastic macrocytic anemias have different etiologies (i.e. there is unimpaired DNA globin synthesis,) which occur, for example in alcoholism.
In addition to the non-specific symptoms of anemia, specific features of vitamin B12 deficiency include peripheral neuropathy and subacute combined degeneration of the cord with resulting balance difficulties from posterior column spinal cord pathology.[4] Other features may include a smooth, red tongue and glossitis.
The treatment for vitamin B12-deficient anemia was first devised by William Murphy who bled dogs to make them anemic and then fed them various substances to see what (if anything) would make them healthy again. He discovered that ingesting large amounts of liver seemed to cure the disease. George Minot and George Whipple then set about to chemically isolate the curative substance and ultimately were able to isolate the vitamin B12 from the liver. All three shared the 1934 Nobel Prize in Medicine.[5]
Normocytic anemia
Normocytic anaemia occurs when the overall hemoglobin levels are always decreased, but the red blood cell size (Mean corpuscular volume) remains normal. Causes include:
- Acute blood loss
- Anemia of chronic disease
- Aplastic anemia (bone marrow failure)
- Hemolytic anemia
Dimorphic anemia
When two causes of anemia act simultaneously, e.g., macrocytic hypochromic, due to hookworm infestation leading to deficiency of both iron and vitamin B12 or folic acid [6] or following a blood transfusion more than one abnormality of red cell indices may be seen. Evidence for multiple causes appears with an elevated RBC distribution width (RDW), which suggests a wider-than-normal range of red cell sizes.
Heinz body anemia
Heinz bodies are an abnormality that form on the cells in this condition. This form of anemia may be brought on by taking certain medications; it is also triggered in cats by eating onions[7] or acetaminophen (Tylenol). It can be triggered in dogs by ingesting onions or zinc, and in horses by ingesting dry red maple leaves.
Specific anemias
- Anemia of prematurity occurs in premature infants at 2 to 6 weeks of age and results from diminished erythropoietin response to declining hematocrit levels.
- Aplastic anemia is a condition generally unresponsive to anti-anemia therapies where bone marrow fails to produce enough red blood cells.
- Fanconi anemia is an hereditary disorder or defect featuring aplastic anemia and various other abnormalities.
- Hemolytic anemia causes a separate constellation of symptoms (also featuring jaundice and elevated LDH levels) with numerous potential causes. It can be autoimmune, immune, hereditary or mechanical (e.g. heart surgery). It can result (because of cell fragmentation) in a microcytic anemia, a normochromic anemia, or (because of premature release of immature red blood cells from the bone marrow), a macrocytic anemia.
- Hereditary spherocytosis is a hereditary defect that results in defects in the RBC cell membrane, causing the erythrocytes to be sequestered and destroyed by the spleen. This leads to a decrease in the number of circulating RBCs and, hence, anemia.
- Sickle-cell anemia, a hereditary disorder, is due to homozygous hemoglobin S genes.
- Warm autoimmune hemolytic anemia is an anemia caused by autoimmune attack against red blood cells, primarily by IgG.
- Cold agglutinin hemolytic anemia is primarily mediated by IgM.
- Pernicious anemia is a form of megaloblastic anaemia due to vitamin B12 deficiency dependent on impaired absorption of vitamin B12.
- Myelophthisic anemia or Myelophthisis is a severe type of anemia resulting from the replacement of bone marrow by other materials, such as malignant tumors or granulomas.
Possible complications
Anemia diminishes the capability of individuals who are affected to perform physical activities. This is a result of one's muscles being forced to depend on anaerobic metabolism. The lack of iron associated with anemia can cause many complications, including hypoxemia, brittle or rigid fingernails, cold intolerance, and possible behavioral disturbances in children. Hypoxemia resulting from anemia can worsen the cardio-pulmonary status of patients with pre-existing chronic pulmonary disease. Cold intolerance occurs in one in five patients with iron deficiency anemia, and becomes visible through numbness and tingling.
Anemia during pregnancy
Anemia affects 20% of all females of childbearing age in the United States. Because of the subtlety of the symptoms, women are often unaware that they have this disorder, as they attribute the symptoms to the stresses of their daily lives. Possible problems for the fetus include increased risk of growth retardation, prematurity, intrauterine death, rupture of the amnion and infection.
During pregnancy, women should be especially aware of the symptoms of anemia, as an adult female loses an average of two milligrams of iron daily. Therefore, she must intake a similar quantity of iron in order to make up for this loss. Additionally, a woman loses approximately 500 milligrams of iron with each pregnancy, compared to a loss of 4-100 milligrams of iron with each period. Possible consequences for the mother include cardiovascular symptoms, reduced physical and mental performance, reduced immune function, fatigue, reduced peripartal blood reserves and increased need for blood transfusion in the postpartum period.
Treatments for anemia
There are many different treatments for anemia and the treatment depends on severity and the cause.
Iron deficiency from nutritional causes is rare in non-menstruating adults (men and post-menopausal women). The diagnosis of iron deficiency mandates a search for potential sources of loss such as gastrointestinal bleeding from ulcers or colon cancer. Mild to moderate iron deficiency anemia is treated by iron supplementation with ferrous sulfate or ferrous gluconate. Vitamin C may aid in the body's ability to absorb iron.
Vitamin supplements given orally (folic acid) or subcutaneously (vitamin B-12) will replace specific deficiencies.
In anemia of chronic disease, anemia associated with chemotherapy, or anemia associated with renal disease, some clinicians prescribe recombinant erythropoietin, epoetin alfa, to stimulate red cell production.
In severe cases of anemia, or with ongoing blood loss, a blood transfusion may be necessary.
Blood transfusions for anemia
Doctors attempt to avoid blood transfusion in general, since multiple lines of evidence point to increased adverse patient clinical outcomes with more intensive transfusion strategies. The physiological principle that reduction of oxygen delivery associated with anemia leads to adverse clinical outcomes is balanced by the finding that transfusion does not necessarily mitigate these adverse clinical outcomes.
In severe, acute bleeding, transfusions of donated blood are often lifesaving. Improvements in battlefield casualty survival is attributable, at least in part, to the recent improvements in blood banking and transfusion techniques.
Transfusion of the stable but anemic hospitalized patient has been the subject of numerous clinical trials, and transfusion is emerging as a deleterious intervention.
Four randomized controlled clinical trials have been conducted to evaluate aggressive versus conservative transfusion strategies in critically ill patients. All four of these studies failed to find a benefit with more aggressive transfusion strategies.[8][9][10][11]
In addition, at least two retrospective studies have shown increases in adverse clinical outcomes with more aggressive transfusion strategies.[12][13]
Hyperbaric Oxygenation
Treatment of exceptional blood loss (anemia) is recognized as an indication for hyperbaric oxygen (HBO) by the Undersea and Hyperbaric Medical Society.[14][15] The use of HBO is indicated when oxygen delivery to tissue is not sufficient in patients who cannot be transfused for medical or religious reasons. HBO may be used for medical reasons when threat of blood product incompatibility or concern for transmissible disease are factors.[14] The beliefs of some religions (ex: Jehovah's Witnesses) may prohibit the receipt of transfused blood products.[14]
In 2002, Van Meter reviewed the publications surrounding the use of HBO in severe anemia and found that all publications report a positive result.[16]
References
- ↑ eMedicine - Anemia, Chronic : Article by Fredrick M Abrahamian, DO, FACEP
- ↑ Recommendations to Prevent and Control Iron Deficiency in the United States MMWR 1998;47 (No. RR-3) p. 5
- ↑ Iron Deficiency Anaemia: Assessment, Prevention, and Control: A guide for programme managers
- ↑ eMedicine - Vitamin B-12 Associated Neurological Diseases : Article by Niranjan N Singh, MD, DM, DNB July 18, 2006
- ↑ Physiology or Medicine 1934 - Presentation Speech
- ↑ Dorlands Medical Dictionary
- ↑ Onions are Toxic to Cats
- ↑ Hébert PC, Wells G, Blajchman MA, et al (1999). "A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group". N. Engl. J. Med. 340 (6): 409–17. PMID 9971864.
- ↑ Bush RL, Pevec WC, Holcroft JW (1997). "A prospective, randomized trial limiting perioperative red blood cell transfusions in vascular patients". Am. J. Surg. 174 (2): 143–8. doi:. PMID 9293831.
- ↑ Bracey AW, Radovancevic R, Riggs SA, et al (1999). "Lowering the hemoglobin threshold for transfusion in coronary artery bypass procedures: effect on patient outcome". Transfusion 39 (10): 1070–7. doi:. PMID 10532600.
- ↑ McIntyre LA, Fergusson DA, Hutchison JS, et al (2006). "Effect of a liberal versus restrictive transfusion strategy on mortality in patients with moderate to severe head injury". Neurocritical care 5 (1): 4–9. doi:. PMID 16960287.
- ↑ Corwin HL, Gettinger A, Pearl RG, et al (2004). "The CRIT Study: Anemia and blood transfusion in the critically ill--current clinical practice in the United States". Crit. Care Med. 32 (1): 39–52. doi:. PMID 14707558.
- ↑ Vincent JL, Baron JF, Reinhart K, et al (2002). "Anemia and blood transfusion in critically ill patients". JAMA 288 (12): 1499–507. doi:. PMID 12243637.
- ↑ 14.0 14.1 14.2 Undersea and Hyperbaric Medical Society. "Exceptional Blood Loss - Anemia". Retrieved on 2008-05-19.
- ↑ Hart GB, Lennon PA, Strauss MB. (1987). "Hyperbaric oxygen in exceptional acute blood-loss anemia". J. Hyperbaric Med 2 (4): 205–210. http://archive.rubicon-foundation.org/4352. Retrieved on 2008-05-19.
- ↑ Van Meter KW (2005). "A systematic review of the application of hyperbaric oxygen in the treatment of severe anemia: an evidence-based approach". Undersea Hyperb Med 32 (1): 61–83. PMID 15796315. http://archive.rubicon-foundation.org/4038. Retrieved on 2008-05-19.
Books
- Breymann, Christian. "Iron Deficiency and Anemia in Pregnancy: Modern Aspects of Diagnosis and Therapy." Blood Cells, Molecules, and Diseases. Nov/Dec: 2002.
- Conrad, Marcel E. "Iron Deficiency Anemia." EMedicine. 8 December 2004.
- Raymond, Tina. "Anemia: Diagnosis, Treatment and Prevention." Midwifery Today. 31 May 1999.
- Scrimshaw, Nevin. Iron deficiency. Scientific American Oct 1991 pp 46-52
- Schier, Stanley L. Approach to the adult patient with anemia. Up-to-Date (subscription required), accessed in Jan 2006, last changed June 2005.
- WHO Scientific Group on Nutritional Anaemias. "Nutritional anaemias : report of a WHO scientific group (meeting held in Geneva from 13 to 17 March 1967)". World Health Organization. Geneva, 1968.
- Ambulatory Management of Common Forms of Anemia - American Academy of Family Physicians
- Bruno de Benoist, Erin McLean, Ines Egli, Mary Cogswell (all Edit.): Worldwide prevalence of anaemia 1993–2005 : WHO global database on anaemia (PDF, 51p, 687kb), World Health Organization, 2008, ISBN 978-92-4-159665-7.
See also
- Hematology
- Human iron metabolism
- Heme
- Hemoglobin
External links
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||