Addiction
The term "addiction" is used in many contexts to describe an obsession, compulsion, or excessive physical dependence or psychological dependence, such as: drug addiction, crime, alcoholism, compulsive overeating, problem gambling, computer addiction, pornography, etc.
In medical terminology, an addiction is a state in which the body relies on a substance for normal functioning and develops physical dependence, as in drug addiction. When the drug or substance on which someone is dependent is suddenly removed, it will cause withdrawal, a characteristic set of signs and symptoms. Addiction is generally associated with increased drug tolerance. In physiological terms, addiction is not necessarily associated with substance abuse since this form of addiction can result from using medication as prescribed by a doctor.
However, common usage of the term addiction has spread to include psychological dependence. In this context, the term is used in drug addiction and substance abuse problems, but also refers to behaviors that are not generally recognized by the medical community as problems of addiction, such as compulsive overeating.
The term addiction is also sometimes applied to compulsions that are not substance-related, such as problem gambling and computer addiction. In these kinds of common usages, the term addiction is used to describe a recurring compulsion by an individual to engage in some specific activity, despite harmful consequences to the individual's health, mental state or social life.
Contents |
History of addiction models
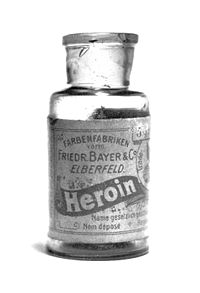
The term 'addiction' appeared as far back as at least 1599, when Shakespeare used it in the first scene of Henry V; however it wasn't until 1906, in reference to opium, that it began to be used regularly. There is also an isolated usage, recorded from 1779, referring to tobacco. The first use of the adjective 'addict' (with the meaning of 'delivered, devoted') was in 1529 and comes from the Latin addictus, pp. of addicere ('deliver, yield, devote,' from ad-, 'to' + dicere, 'say, declare').[1]
Prior to the latter half of the 20th Century, addiction was primarily a pharmacological term that referred to the process of developing drug tolerance so that more of a drug was required, more frequently, for the same effect to occur. However, with the founding of Alcoholics Anonymous in 1935, the allergy concept eventually morphed into the disease-model of addiction was proposed, based on the work of Dr. William Duncan Silkworth, and began to gather support in the professional community, amongst medical and social services workers, and amongst addicts themselves. The disease-model concept led to a definition of addiction based on the continued use of alcohol or drugs despite negative consequences for the user. This latter definition is now thought of as a disease state by the medical community. Morse and Flavin summarise the disease-model definition of addiction commonly utilized by treatment centers and substance abuse counselors:
Addiction is a primary, progressive, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over use of the substance, preoccupation with the substance, use of the substance despite adverse consequences, and distortions in thinking.[2]
In the latter half of the 20th Century, the twelve-step program began to be applied to a wide range of problem behaviours, many never previously identified as addictions. For example, during this process the establishment of Overeaters Anonymous in 1960 led to the identification of an associated concept of food addiction[3] [4]and the establishment of Sex and Love Addicts Anonymous in 1977 led to the identification of the concept of sexual addiction.[5][6] However, although these terms are widely used in the recovery movement, and by commentators on that movement, neither of them are widely accepted by members of the professional communities working in the fields of addiction.
In the 21st Century, attempts have been made to model addiction using the tools of Economics, for instance, by calculating the elasticity of addictive goods and determining to what extent present income and consumption has on future consumption.[7] In general, most modern economists identify 3 models of addiction when analyzing patterns for policy research. These are:
-Myopic/Naive: This model essentially stipulates that addicts are characterized by near-sighted behavior and are wholly incapable of ascertaining the potential implications of their behavior. Therefore, under this model, demand for whatever the addict is addicted to would be totally inelastic, implying that the addict is unable to even slightly reduce comsumption regardless of cost.
-Rational time-consistent: Under this model, the addict is assumed to be perfectly aware of future consequences of their behavior and is assumed to have fully considered all benefits and costs of their actions. Under this model, the elasticity of demand would be very high (at or nearing 1), implying that the addict will almost certainly change their behavior in response to price, since a high price may outweigh potential benefits.
-Time-inconsistent (as well as imperfectly rational): Under this model, the addict is assumed to be capable of some level of analysis of the benefits and costs of their behavior, but may not be able to act on the conclusions of this analysis due to physical dependencies and/or insufficient "willpower". The essence of this model is an an attempt to classify typical behavior by which most addicts wish they could quit, indicating rationality and proper benefit/cost analysis, but are still unable to. Under this model, there is a moderate level of elasticity indicating some but not prefect responsiveness to price.
Definition
Not all doctors agree on the exact nature of addiction or dependency.[8] Traditionally, addiction has been defined with regard solely to psychoactive substances (for example alcohol, tobacco and other drugs) which cross the blood-brain barrier once ingested, temporarily altering the chemical milieu of the brain. However, "studies on phenomenology, family history, and response to treatment suggest that intermittent explosive disorder, kleptomania, pathological gambling, pyromania, and trichotillomania may be related to mood disorders, alcohol and psychoactive substance abuse, and anxiety disorders (especially obsessive-compulsive disorder)."[9] However, such disorders are classified by the American Psychological Association as impulse control disorders and therefore not as addictions.
Many people, both psychology professionals and laypersons, now feel that there should be accommodation made to include psychological dependency on such things as gambling, food, sex, pornography, computers, work, exercise, cutting, shopping, and religion so these behaviors count as diseases as well and cause guilt, shame, fear, hopelessness, failure, rejection, anxiety, or humiliation symptoms associated with, among other medical conditions, depression,epilepsy, and hyperreligiosity.[10][11][12][13] In depression related to religious addiction "The religious addict seeks to avoid pain and overcome shame by becoming involved in a belief system which offers security through its rigidity and its absolute values."[14] While religion and spirituality may play a key role in psychotherapeutic support and recovery, it can also be a source of pain, guilt and exclusion, and religious themes may also play a negative role in psychopathology.[15] Although, the above mentioned are things or tasks which, when used or performed, do not fit into the traditional view of addiction and may be better defined as an obsessive-compulsive disorder,withdrawal symptoms may occur with abatement of such behaviors. It is said by those who adhere to a traditionalist view that these withdrawal-like symptoms are not strictly reflective of an addiction, but rather of a behavioral disorder. However, understanding of neural science, the brain, the nervous system, human behavior, and affective disorders has revealed "the impact of molecular biology in the mechanisms underlying developmental processes and in the pathogenesis of disease".[16] The use of thyroid hormones as an effective adjunct treatment for affective disorders has been studied over the past three decades and has been confirmed repeatedly.[17] In spite of traditionalist protests and warnings that overextension of definitions may cause the wrong treatment to be used (thus failing the person with the behavioral problem), popular media, and some members of the field, do represent the aforementioned behavioral examples as addictions.
Varied forms of addiction
In the United States, physical dependence, abuse of, and withdrawal from drugs and other substances is outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV TR). It does not use the word 'addiction' at all. It has instead a section about Substance dependence:
"Substance dependence When an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed. Compulsive and repetitive use may result in tolerance to the effect of the drug and withdrawal symptoms when use is reduced or stopped. This, along with Substance Abuse are considered Substance Use Disorders..."[18]
Terminology has become quite complicated in the field. Pharmacologists continue to speak of addiction from a physiologic standpoint (some call this a physical dependence); psychiatrists refer to the disease state as psychological dependence; most other physicians refer to the disease as addiction. The field of psychiatry is now considering, as they move from DSM-IV to DSM-V, transitioning from "substance dependence" to "addiction" as terminology for the disease state.
The medical community now makes a careful theoretical distinction between physical dependence (characterized by symptoms of withdrawal) and psychological dependence (or simply addiction). Addiction is now narrowly defined as "uncontrolled, compulsive use"; if there is no harm being suffered by, or damage done to, the patient or another party, then clinically it may be considered compulsive, but to the definition of some it is not categorized as 'addiction'. In practice, the two kinds of addiction are not always easy to distinguish. Addictions often have both physical and psychological components.
There is also a lesser known situation called pseudo-addiction.[19] A patient will exhibit drug-seeking behavior reminiscent of psychological addiction, but they tend to have genuine pain or other symptoms that have been under-treated. Unlike true psychological addiction, these behaviors tend to stop when the pain is adequately treated. The obsolete term physical addiction is deprecated, because of its connotations. In modern pain management with opioids physical dependence is nearly universal. While opiates are essential in the treatment of acute pain, the benefit of this class of medication in chronic pain is not well proven. Clearly, there are those who would not function well without opiate treatment; on the other hand, many states are noting significant increases in non-intentional deaths related to opiate use. High-quality, long-term studies are needed to better delineate the risks and benefits of chronic opiate use.
Physical dependency
Physical dependence on a substance is defined by the appearance of characteristic withdrawal symptoms when the substance is suddenly discontinued. Opiates, amphetamines, benzodiazepines, barbiturates, alcohol and nicotine induce physical dependence. On the other hand, some categories of substances share this property and are still not considered addictive: cortisone, beta blockers and most antidepressants are examples. So, while physical dependency can be a major factor in the psychology of addiction and most often becomes a primary motivator in the continuation of an addiction, the initial primary attribution of an addictive substance is usually its ability to induce pleasure, although with continued use the goal is not so much to induce pleasure as it is to relieve the anxiety caused by the absence of a given addictive substance, causing it to become used compulsively. An example of this is nicotine; A cigarette can be described as pleasurable, but is in fact fulfilling the physical addiction of the user, and therefore, is achieving pleasurable feelings relative to his/her previous state of physical withdrawal. Further, the physical dependency of the nicotine addict on the substance itself becomes an overwhelming factor in the continuation of use.
Some substances induce physical dependence or physiological tolerance - but not addiction - for example many laxatives, which are not psychoactive; nasal decongestants, which can cause rebound congestion if used for more than a few days in a row; and some antidepressants, most notably venlafaxine, paroxetine and sertraline, as they have quite short half-lives, so stopping them abruptly causes a more rapid change in the neurotransmitter balance in the brain than many other antidepressants. Many non-addictive prescription drugs should not be suddenly stopped, so a doctor should be consulted before abruptly discontinuing them.
The speed with which a given individual becomes addicted to various substances varies with the substance, the frequency of use, the means of ingestion, the intensity of pleasure or euphoria, and the individual's genetic and psychological susceptibility. Some people may exhibit alcoholic tendencies from the moment of first intoxication, while most people can drink socially without ever becoming addicted. Opioid dependent individuals have different responses to even low doses of opioids than the majority of people, although this may be due to a variety of other factors, as opioid use heavily stimulates pleasure-inducing neurotransmitters in the brain. Nonetheless, because of these variations, in addition to the adoption and twin studies that have been well replicated, much of the medical community is satisfied that addiction is in part genetically moderated. That is, one's genetic makeup may regulate how susceptible one is to a substance and how easily one may become psychologically attached to a pleasurable routine.
Eating disorders are complicated pathological mental illnesses and thus are not the same as addictions described in this article. Eating disorders, which some argue are not addictions at all, are driven by a multitude of factors, most of which are highly different than the factors behind addictions described in this article. It has been reported, however, that patients with eating disorders can successfully be treated with the same non-pharmacological protocols used in patients with chemical addiction disorders.[20] Gambling is another potentially addictive behavior with some biological overlap. Conversely gambling urges have emerged with the administration of Mirapex (pramipexole), a dopamine agonist.[21]
Psychological dependency
Psychological dependency is a dependency of the mind, and leads to psychological withdrawal symptoms (such as cravings, irritability, insomnia, depression, anorexia, etc). Addiction can in theory be derived from any rewarding behaviour, and is believed to be strongly associated with the dopaminergic system of the brain's reward system (as in the case of cocaine and amphetamines). Some claim that it is a habitual means to avoid undesired activity, but typically it is only so to a clinical level in individuals who have emotional, social, or psychological dysfunctions (psychological addiction is defined as such), replacing normal positive stimuli not otherwise attained (see Rat Park study).
A person who is physically dependent, but not psychologically dependent can have their dose slowly dropped until they are no longer dependent. However, if that person is psychologically dependent, they are still at serious risk for relapse into abuse and subsequent physical dependence.
Psychological dependence does not have to be limited only to substances; even activities and behavioral patterns can be considered addictions, if they become uncontrollable, e.g. problem gambling, Internet addiction, computer addiction, sexual addiction / pornography addiction, eating, self-injury, or work addiction.
Addiction and drug control legislation
Most countries have legislation which brings various drugs and drug-like substances under the control of licensing systems. Typically this legislation covers any or all of the opiates, amphetamines, cannabinoids, cocaine, barbiturates, hallucinogens (tryptamines, LSD, phencyclidine(PCP), psilocybin) and a variety of more modern synthetic drugs, and unlicensed production, supply or possession may be a criminal offense.
Usually, however, drug classification under such legislation is not related simply to addictiveness. The substances covered often have very different addictive properties. Some are highly prone to cause physical dependency, whilst others rarely cause any form of compulsive need whatsoever. Typically nicotine (in the form of tobacco) is regulated extremely loosely, if at all, although it is well-known as one of the most addictive substances ever discovered.
Also, although the legislation may be justifiable on moral grounds to some, it can make addiction or dependency a much more serious issue for the individual. Reliable supplies of a drug become difficult to secure as illegally produced substances may have contaminants. Withdrawal from the substances or associated contaminants can cause additional health issues and the individual becomes vulnerable to both criminal abuse and legal punishment. Criminal elements that can be involved in the profitable trade of such substances can also cause physical harm to users.
Methods of care
Early editions of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) described addiction as a physical dependency to a substance that resulted in withdrawal symptoms in its absence. Recent editions, including DSM-IV, have moved toward a diagnostic instrument that classifies such conditions as dependency, rather than addiction. The American Society of Addiction Medicine recommends treatment for people with chemical dependency based on patient placement criteria (currently listed in PPC-2), which attempt to match levels of care according to clinical assessments in six areas, including:
- Acute intoxication and/or withdrawal potential
- Biomedical conditions or complications
- Emotional/behavioral conditions or complications
- Treatment acceptance/resistance
- Relapse potential
- Recovery environment
Some medical systems, including those of at least 15 states of the United States, refer to an Addiction Severity Index to assess the severity of problems related to substance use. The index assesses problems in six areas: medical, employment/support, alcohol and other drug use, legal, family/social, and psychiatric.
While addiction or dependency is related to seemingly uncontrollable urges, and arguably could have roots in genetic predispositions, treatment of dependency is conducted by a wide range of medical and allied professionals, including Addiction Medicine specialists, psychiatrists, and appropriately trained nurses, social workers, and counselors. Early treatment of acute withdrawal often includes medical detoxification, which can include doses of anxiolytics or narcotics to reduce symptoms of withdrawal. An experimental drug, ibogaine,[22] is also proposed to treat withdrawal and craving. Alternatives to medical detoxification include acupuncture detoxification. In chronic opiate addiction, a surrogate drug such as methadone is sometimes offered as a form of opiate replacement therapy. But treatment approaches universal focus on the individual's ultimate choice to pursue an alternate course of action.
Therapists often classify patients with chemical dependencies as either interested or not interested in changing. Treatments usually involve planning for specific ways to avoid the addictive stimulus, and therapeutic interventions intended to help a client learn healthier ways to find satisfaction. Clinical leaders in recent years have attempted to tailor intervention approaches to specific influences that affect addictive behavior, using therapeutic interviews in an effort to discover factors that led a person to embrace unhealthy, addictive sources of pleasure or relief from pain.
| Treatment Modality Matrix | ||
|---|---|---|
| Behavioral Pattern | Intervention | Goals |
| Low self-esteem, anxiety, verbal hostility | Relationship therapy, client centered approach | Increase self esteem, reduce hostility and anxiety |
| Defective personal constructs, ignorance of interpersonal means | Cognitive restructuring including directive and group therapies | Insight |
| Focal anxiety such as fear of crowds | Desensitization | Change response to same cue |
| Undesirable behaviors, lacking appropriate behaviors | Aversive conditioning, operant conditioning, counter conditioning | Eliminate or replace behavior |
| Lack of information | Provide information | Have client act on information |
| Difficult social circumstances | Organizational intervention, environmental manipulation, family counseling | Remove cause of social difficulty |
| Poor social performance, rigid interpersonal behavior | Sensitivity training, communication training, group therapy | Increase interpersonal repertoire, desensitization to group functioning |
| Grossly bizarre behavior | Medical referral | Protect from society, prepare for further treatment |
| Adapted from: Essentials of Clinical Dependency Counseling, Aspen Publishers | ||
From the applied behavior analysis literature and the behavioral psychology literature several evidenced based intervention programs have emerged (1) behavioral maritial therapy (2) community reinforcement approach (3) cue exposure therapy and (4) contingency management strategies.[23][24] In addition, the same author suggest that Social skills training adjunctive to inpatient treatment of alcohol dependence is probably efficacious.
Diverse explanations
Several explanations (or "models") have been presented to explain addiction. These divide, more or less, into the models which stress biological or genetic causes for addiction, and those which stress social or purely psychological causes. Of course there are also many models which attempt to see addiction as both a physiological and a psycho-social phenomenon.
- The disease model of addiction holds that addiction is a disease, coming about as a result of either the impairment of neurochemical or behavioral processes, or of some combination of the two. Within this model, addictive disease is treated by specialists in Addiction Medicine. Within the field of medicine, the American Medical Association, National Association of Social Workers, and American Psychological Association all have policies which are predicated on the theory that addictive processes represent a disease state. Most treatment approaches, as well, are based on the idea that dependencies are behavioral dysfunctions, and, therefore, contain, at least to some extent, elements of physical or mental disease. Organizations such as the American Society of Addiction Medicine believe the research-based evidence for addiction's status as a disease is overwhelming.
- The pleasure model proposed by professor Nils Bejerot. Addiction "is an emotional fixation (sentiment) acquired through learning, which intermittently or continually expresses itself in purposeful, stereotyped behavior with the character and force of a natural drive, aiming at a specific pleasure or the avoidance of a specific discomfort." "The pleasure mechanism may be stimulated in a number of ways and give rise to a strong fixation on repetitive behavior. Stimulation with drugs is only one of many ways, but one of the simplest, strongest,and often also the most destructive" "If the pleasure stimulation becomes so strong that it captivates an individual with the compulsion and force characteristic of natural drives, then there exists...an addiction" [25] The pleasure model is used as one of the reason for zero tolerance for use of illicit drugs
- The genetic model posits a genetic predisposition to certain behaviors. It is frequently noted that certain addictions "run in the family," and while researchers continue to explore the extent of genetic influence, many researchers argue that there is strong evidence that genetic predisposition is often a factor in dependency.
- The experiential model devised by Stanton Peele argues that addictions occur with regard to experiences generated by various involvements, whether drug-induced or not. This model is in opposition to the disease, genetic, and neurobiological approaches. Among other things, it proposes that addiction is both more temporary or situational than the disease model claims, and is often outgrown through natural processes.
- The opponent-process model generated by Richard Soloman states that for every psychological event A will be followed by its opposite psychological event B. For example, the pleasure one experiences from heroin is followed by an opponent process of withdrawal, or the terror of jumping out of an airplane is rewarded with intense pleasure when the parachute opens. This model is related to the opponent process color theory. If you look at the color red then quickly look at a gray area you will see green. There are many examples of opponent processes in the nervous system including taste, motor movement, touch, vision, and hearing. Opponent-processes occurring at the sensory level may translate "down-stream" into addictive or habit-forming behavior.
- The allostatic (stability through change) model generated by George Koob and Michel LeMoal is a modification of the opponent process theory where continued use of a drug leads to a spiralling of uncontrolled use, negative emotional states and withdrawal and a shift into use to new allostatic set point which is lower than that maintained before use of the drug.[26]
- The cultural model recognizes that the influence of culture is a strong determinant of whether or not individuals fall prey to certain addictions. For example, alcoholism is rare among Saudi Arabians, where obtaining alcohol is difficult and using alcohol is prohibited. In North America, on the other hand, the incidence of gambling addictions soared in the last two decades of the 20th century, mirroring the growth of the gaming industry. Half of all patients diagnosed as alcoholic are born into families where alcohol is used heavily, suggesting that familiar influence, genetic factors, or more likely both, play a role in the development of addiction. What also needs to be noted is that when people don't gain a sense of moderation through their development they can be just as likely, if not more, to abuse substances than people born into alcoholic families.
- The moral model states that addictions are the result of human weakness, and are defects of character. Those who advance this model do not accept that there is any biological basis for addiction. They often have scant sympathy for people with serious addictions, believing either that a person with greater moral strength could have the force of will to break an addiction, or that the addict demonstrated a great moral failure in the first place by starting the addiction. The moral model is widely applied to dependency on illegal substances, perhaps purely for social or political reasons, but is no longer widely considered to have any therapeutic value. Elements of the moral model, especially a focus on individual choices, have found enduring roles in other approaches to the treatment of dependencies.
- The habit model or "life-process model" proposed by Thomas Szasz questions the very concept of "addiction." He argues that addiction is a metaphor, and that the only reason to make the distinction between habit and addiction "is to persecute somebody." [27] However, the nature of this metaphor is unclear, and the list of groups that rejects Szasz's opinion that mental illness is a myth includes the American Psychiatric Association (APA) and the National Institute of Mental Health (NIMH).
- Finally, the blended model attempts to consider elements of all other models in developing a therapeutic approach to dependency. It holds that the mechanism of dependency is different for different individuals, and that each case must be considered on its own merits.
Neurobiological basis
The development of addiction is thought to involve a simultaneous process of 1) increased focus on and engagement in a particular behavior and 2) the attenuation or "shutting down" of other behaviors. For example, under certain experimental circumstances such as social deprivation and boredom, animals allowed the unlimited ability to self-administer certain psychoactive drugs will show such a strong preference that they will forgo food, sleep, and sex for continued access. The neuro-anatomical correlate of this is that the brain regions involved in driving goal-directed behavior grow increasingly selective for particular motivating stimuli and rewards, to the point that the brain regions involved in the inhibition of behavior can no longer effectively send "stop" signals. A good analogy is to imagine flooring the gas pedal in a car with very bad brakes. In this case, the limbic system is thought to be the major "driving force" and the orbitofrontal cortex is the substrate of the top-down inhibition.
A specific portion of the limbic circuit known as the mesolimbic dopaminergic system is hypothesized to play an important role in translation of motivation to motor behavior- and reward-related learning in particular. It is typically defined as the ventral tegmental area (VTA), the nucleus accumbens, and the bundle of dopamine-containing fibers that are connecting them. This system is commonly implicated in the seeking out and consumption of rewarding stimuli or events, such as sweet-tasting foods or sexual interaction. However, its importance to addiction research goes beyond its role in "natural" motivation: while the specific site or mechanism of action may differ, all known drugs of abuse have the common effect in that they elevate the level of dopamine in the nucleus accumbens. This may happen directly, such as through blockade of the dopamine re-uptake mechanism (see cocaine). It may also happen indirectly, such as through stimulation of the dopamine-containing neurons of the VTA that synapse onto neurons in the accumbens (see opiates). The euphoric effects of drugs of abuse are thought to be a direct result of the acute increase in accumbal dopamine.[28]
The human body has a natural tendency to maintain homeostasis, and the central nervous system is no exception. Chronic elevation of dopamine will result in a decrease in the number of dopamine receptors available in a process known as downregulation. The decreased number of receptors changes the permeability of the cell membrane located post-synaptically, such that the post-synaptic neuron is less excitable- i.e.: less able to respond to chemical signaling with an electrical impulse, or action potential. It is hypothesized that this dulling of the responsiveness of the brain's reward pathways contributes to the inability to feel pleasure, known as anhedonia, often observed in addicts. The increased requirement for dopamine to maintain the same electrical activity is the basis of both physiological tolerance and withdrawal associated with addiction.
Downregulation can be classically conditioned. If a behavior consistently occurs in the same environment or contingently with a particular cue, the brain will adjust to the presence of the conditioned cues by decreasing the number of available receptors in the absence of the behavior. It is thought that many drug overdoses are not the result of a user taking a higher dose than is typical, but rather that the user is administering the same dose in a new environment.
In cases of physical dependency on depressants of the central nervous system such as opioids, barbiturates, or alcohol, the absence of the substance can lead to symptoms of severe physical discomfort. Withdrawal from alcohol or sedatives such as barbiturates or benzodiazepines (valium-family) can result in seizures and even death. By contrast, withdrawal from opioids, which can be extremely uncomfortable, is rarely if ever life-threatening. In cases of dependence and withdrawal, the body has become so dependent on high concentrations of the particular chemical that it has stopped producing its own natural versions (endogenous ligands) and instead produces opposing chemicals. When the addictive substance is withdrawn, the effects of the opposing chemicals can become overwhelming. For example, chronic use of sedatives (alcohol, barbiturates, or benzodiazepines) results in higher chronic levels of stimulating neurotransmitters such as glutamate. Very high levels of glutamate kill nerve cells, a phenomenon called excitatory neurotoxicity.
Criticism
A strong form of criticism comes from Thomas Szasz, who denies that addiction is a psychiatric problem. In many of his works, he argues that addiction is a choice, and that a drug addict is one who simply prefers a socially taboo substance rather than, say, a low risk lifestyle. In Our Right to Drugs, Szasz cites the biography of Malcolm X to corroborate his economic views towards addiction: Malcolm claimed that quitting cigarettes was harder than shaking his heroin addiction. Szasz postulates that humans always have a choice, and it is foolish to call someone an 'addict' just because they prefer a drug induced euphoria to a more popular and socially welcome lifestyle.
Szasz is not alone in questioning the standard view of addiction. Professor John Booth Davies at the University of Strathclyde has argued in his book The Myth of Addiction that 'people take drugs because they want to and because it makes sense for them to do so given the choices available' as opposed to the view that 'they are compelled to by the pharmacology of the drugs they take'.[29] He uses an adaptation of attribution theory (what he calls the theory of functional attributions) to argue that the statement 'I am addicted to drugs' is functional, rather than veridical. Stanton Peele has put forward similar views.
Experimentally, Bruce K. Alexander used the classic experiment of Rat Park to show that 'addicted' behaviour in rats only occurred when the rats had no other options. When other options and behavioural opportunities were put in place, the rats soon showed far more complex behaviours.
Casual addiction
The word addiction is also sometimes used colloquially to refer to something for which a person has a passion, such as books, chocolate, work, the web, running, postage stamp collecting, or eating.
See also
- Addiction recovery groups
- Addiction medicine
- Akrasia
- Alcoholism
- Alcohol withdrawal syndrome
- Benzodiazepine withdrawal syndrome
- Codependence
- Cold turkey
- Computer addiction
- Conditioned place preference
- Cue reactivity
- Disease model of addiction
- Drug addiction
- Drug Interventions Programme
- E. Morton Jellinek
- Higher order desire
- Junkie
- Life-process model of addiction
- Love addiction
- Physical dependence
- Problem gambling
- Sexual addiction
- Smoking
- Tanha
- Television addiction
- Treatment Improvement Protocols
- Twelve-step programs
Notes
- ↑ Harper, Douglas (2001). "Addiction" (HTML). Online Etymology Dictionary. Retrieved on 2008-03-24.
- ↑ Morse, RM; Flavin DK (1992). "The definition of alcoholism. The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine to Study the Definition and Criteria for the Diagnosis of Alcoholism". JAMA 268 (8): 1012–4. doi:. PMID 1501306. http://jama.ama-assn.org/. Retrieved on 2008-06-29.
- ↑ Sheppard, Kay (2000). From the First Bite. Health Communications, Inc.. pp. p.40. ISBN 978-1558747548. http://books.google.co.uk/books?id=qUtaGzDFtBgC&pg=PA40&dq=food+addiction+compulsive+overeating&lr=&client=firefox-a&sig=ACfU3U1HYi9Oyggrv9beGtiWMuwMbHKe9Q#PPA40,M1.
- ↑ Okasaka Y, Morita N, Nakatani Y, Fujisawa K (February 2008). "Correlation between addictive behaviors and mental health in university students". Psychiatry Clin. Neurosci. 62 (1): 84–92. doi:. PMID 18289145. http://www3.interscience.wiley.com/journal/119415087/abstract.
- ↑ *Earle, Ralph and Crow, Gregory Lonely All The Time: Recognizing, Understanding and Overcoming Sex Addiction, for Addicts and Co-Dependents New York, New York: Pocket Books 1989
- ↑ Bird MH (July 2006). "Sexual addiction and marriage and family therapy: facilitating individual and relationship healing through couple therapy". J Marital Fam Ther 32 (3): 297–311. doi:. PMID 16933435. http://www3.interscience.wiley.com/journal/118628074/abstract.
- ↑ Chaloupka, Frank; Taurus, J; Grossman, M.. "Economic Models of Addiction and Applications to Cigarette Smoking and Other Substance Abuse". University of Illinois at Chicago. Retrieved on 2006-09-01.
- ↑ Goodman A (November 1990). "Addiction: definition and implications". Br J Addict 85 (11): 1403–8. doi:. PMID 2285834. http://www3.interscience.wiley.com/journal/119381659/abstract.
- ↑ McElroy, S.L.; J.I. Hudson, Hg. Pope Jr, P.E. Keck Jr and H.G. Aizley (1992). "The DSM-III-R impulse control disorders not elsewhere classified: clinical characteristics and relationship to other psychiatric disorders". American Journal of Psychiatry (American Psychiatric Publishing Inc.) 149: 318–327. PMID 1536268. http://ajp.psychiatryonline.org/cgi/content/abstract/149/3/318. Retrieved on 2008-03-24.
- ↑ Taylor, C.Z. (March 2002). "Religious Addiction: Obsession with Spirituality". Pastoral Psychology (Springer Netherlands) 50 (4): 291–315. doi:. http://www.springerlink.com/content/9ner79ge7kntx3hp/. Retrieved on 2008-03-24.
- ↑ "Depression". The Columbia Electronic Encyclopedia. (2007). Columbia University Press. Retrieved on 2008-03-24.
- ↑ Nowack, W.J. (2006-08-29). "Psychiatric Disorders Associated With Epilepsy" (HTML). eMedicine Specialities. WebMD. Retrieved on 2008-03-24.
- ↑ Beck, D.A. (2007). "Psychiatric Disorders due to General Medical Conditions" (PDF). Department of Psychiatry, University of Missouri-Columbia. Retrieved on 2008-03-24.
- ↑ Vanderheyden, P.A. (2004). "Religious Addiction: The Subtle Destruction of the Soul". Pastoral Psychology (Springer Netherlands) 47 (4): 293–302. doi:. http://www.springerlink.com/content/l23168155216kh58/. Retrieved on 2008-03-24.
- ↑ Keks, N.; R. deSouza (June 2003). "Spirituality and psychosis". Australasian Psychiatry (Blackwell Synergy) 11 (2): 170–171. doi:. http://www.blackwell-synergy.com/doi/abs/10.1046/j.1039-8562.2003.00510.x. Retrieved on 2008-03-24.
- ↑ Kandel, E.R.; J.H. Schwartz, T.M. Jessell (2000). Principles of Neural Science. Magraw-Hill Professional. ISBN 978-0071120005. http://books.google.com/books?hl=en&lr=&id=yzEFK7Xc87YC&oi=fnd&pg=PR35&dq=psychiatry+behavior+mood+disorders+addiction+hormones&ots=5yowgvrIK5&sig=fMAFWjZKzazKOIIh8yXzoWx_K3s#PPP1,M1.
- ↑ Bauer, M.; A. Heinz, P.C. Whybrow (2002). "Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain". Molecular Psychiatry (Nature) 7 (2): 140–156. doi:. http://www.nature.com/mp/journal/v7/n2/abs/4000963a.html. Retrieved on 2008-03-24.
- ↑ DSM-IV & DSM-IV-TR:Substance Dependence
- ↑ Weissman, D.E.; J.D. Haddox (1989). "Opioid pseudoaddiction--an iatrogenic syndrome". Pain (International Association for the Study of Pain) 36 (3): 363–366. PMID 2710565.
- ↑ AJ Giannini, M Keller, GC Colapietro, SM Melemis, N Leskovac, T Timcisko. Comparison of alternative treatment techniques in bulimia: The chemical dependency approach. Psychological Reports. 82(2):451-458, 1998.
- ↑ AJ Giannini. Drugs of Abuse--Second Edition. Los Angeles, Practice Management Information Corporation, 1997.
- ↑ Alper KR, Lotsof HS, Kaplan CD (January 2008). "The ibogaine medical subculture". J Ethnopharmacol 115 (1): 9–24. doi:. PMID 18029124.
- ↑ O'Donohue, W; K.E. Ferguson (2006). "Evidence-Based Practice in Psychology and Behavior Analysis" (– Scholar search). The Behavior Analyst Today (Joseph D. Cautilli) 7 (3): 335–350. http://www.behavior-analyst-today.com/VOL-7/BAT-7-3.PDF. Retrieved on 2008-03-24.
- ↑ Chambless et al, D.L. (1998). "[www.apa.org/divisions/div12/est/newrpt.pdf An update on empirically validated therapies]" (PDF). Clinical Psychology (American Psychological Association) 49: 5–14. www.apa.org/divisions/div12/est/newrpt.pdf. Retrieved on 2008-03-24.
- ↑ Nils Bejerot in Theories of Drug abuse, Selected contemporary perspectives, page 246-255, NIDA, 1980
- ↑ Koob GF, Le Moal M (February 2001). "Drug addiction, dysregulation of reward, and allostasis". Neuropsychopharmacology 24 (2): 97–129. doi:. PMID 11120394.
- ↑ Buckley, William F., Szasz, Professor Thomas Stephen. (1973). Drugs and Freedom [Partial transcript]. Hoover Institution Archives Firing Line Television Program Collection.
- ↑ Wise RA (April 1996). "Neurobiology of addiction". Curr. Opin. Neurobiol. 6 (2): 243–51. doi:. PMID 8725967. http://linkinghub.elsevier.com/retrieve/pii/S0959-4388(96)80079-1.
- ↑ Davies, John Booth (1998-01-18). The Myth of Addiction. Psychology Press Ltd (2nd rev edition). ISBN 978-9057022371. http://www.druglibrary.org/special/davies/mythprologue.htm.
Further reading
- Lende DH, Smith EO (April 2002). "Evolution meets biopsychosociality: an analysis of addictive behavior". Addiction 97 (4): 447–58. PMID 11964060. http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0965-2140&date=2002&volume=97&issue=4&spage=447.
- Ornstein, C., (2005-11-14). Quitting meth pays off. LA Times.
External links
- Addiction at the Open Directory Project
- Robert Wood Johnson Foundation - Addiction publications