Paracetamol
 |
|
 |
|
|
Paracetamol
|
|
| Systematic (IUPAC) name | |
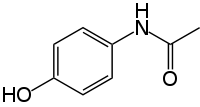
| N-(4-hydroxyphenyl)acetamide | |
| Identifiers | |
| CAS number | |
| ATC code | N02 |
| PubChem | |
| DrugBank | |
| ChemSpider | |
| Chemical data | |
| Formula | C8H9NO2 |
| Mol. mass | 151.169 g/mol |
| SMILES | & |
| Physical data | |
| Density | 1.263 g/cm³ |
| Melt. point | 169 °C (336 °F) |
| Solubility in water | 14 mg/mL @ 25C [1] mg/mL (20 °C) |
| Pharmacokinetic data | |
| Bioavailability | almost 100% |
| Metabolism | 90 to 95% Hepatic |
| Half life | 1–4 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral, rectal, intravenous |
Paracetamol (INN) (IPA: /ˌpærəˈsiːtəmɒl, -ˈsɛtə-/) or acetaminophen (USAN) is a widely-used analgesic and antipyretic medication. Derived from coal tar, it is the active metabolite of phenacetin, but unlike phenacetin, paracetamol has not been shown to be carcinogenic in any way. Paracetamol generally is well tolerated, lacks many of the side-effects of aspirin, and is available over-the-counter. It is commonly used for the relief of fever, headaches, and other minor aches and pains. In combination with non-steroidal anti-inflammatory drugs (NSAIDs) or opioid analgesics, paracetamol is used also in the management of more severe pain.[2] Paracetamol is a major ingredient in numerous cold and flu remedies.
While generally safe for human use at recommended doses, acute overdoses of paracetamol can cause potentially fatal liver damage and, in rare individuals, a normal dose can do the same. Paracetamol toxicity is the foremost cause of acute liver failure in the Western world, and accounts for most drug overdoses in the United States, the United Kingdom, Australia and New Zealand.[3][4][5][6] This risk is heightened by alcoholism. A 2008 study indicates that Paracetamol given to infants may also be linked to an increased risk of developing asthma in children.[7][8][9]
The words acetaminophen and paracetamol come from the chemical names for the compound: para-acetylaminophenol and para-acetylaminophenol. The brand name Tylenol also derives from this name: para-acetylaminophenol. In some contexts, it is shortened to APAP, for N-acetyl-para-aminophenol.
Contents |
History
In ancient and medieval times, known antipyretic agents were compounds contained in white willow bark (a family of chemicals known as salicins, which led to the development of aspirin), and compounds contained in cinchona bark.[10] Cinchona bark was also used for the extraction of the anti-malaria drug quinine. Quinine itself also has antipyretic effects. Efforts to refine and isolate salicin and salicylic acid took place throughout the middle- and late-19th century, and was accomplished by Bayer chemist Felix Hoffmann (this was also done by French chemist Charles Frédéric Gerhardt 40 years earlier, but he abandoned the work after deciding it was impractical).[11]
When the cinchona tree became scarce in the 1880s, people began to look for alternatives. Two alternative antipyretic agents were developed in the 1880s: acetanilide in 1886 and phenacetin in 1887. Harmon Northrop Morse first synthesized paracetamol via the reduction of p-nitrophenol with tin in glacial acetic acid in 1878;[12] however, paracetamol was not used in medical treatment for another 15 years. In 1893, paracetamol was discovered in the urine of individuals who had taken phenacetin, and was concentrated into a white, crystalline compound with a bitter taste. In 1899, paracetamol was found to be a metabolite of acetanilide. This discovery was largely ignored at the time.

In 1946, the Institute for the Study of Analgesic and Sedative Drugs awarded a grant to the New York City Department of Health to study the problems associated with analgesic agents. Bernard Brodie and Julius Axelrod were assigned to investigate why non-aspirin agents were associated with the development of methemoglobinemia, a condition that decreases the oxygen-carrying capacity of blood and is potentially lethal. In 1948, Brodie and Axelrod linked the use of acetanilide with methemoglobinemia and determined that the analgesic effect of acetanilide was due to its active metabolite paracetamol. They advocated the direct use of paracetamol, since it did not have the toxic effects of acetanilide.[13]
The product was first sold in 1955 by McNeil Laboratories as a pain and fever reliever for children, under the brand name Tylenol Children's Elixir.[14]
In 1956, 500 mg tablets of paracetamol went on sale in the United Kingdom under the trade name Panadol, produced by Frederick Stearns & Co, a subsidiary of Sterling Drug Inc. Panadol was originally available only by prescription, for the relief of pain and fever, and was advertised as being "gentle to the stomach," since other analgesic agents of the time contained aspirin, a known stomach irritant. In June 1958, a children's formulation, Panadol Elixir, was released.
In 1963, paracetamol was added to the British Pharmacopoeia, and has gained popularity since then as an analgesic agent with few side-effects and little interaction with other pharmaceutical agents.
The U.S. patent on paracetamol has long expired, and generic versions of the drug are widely available under the Drug Price Competition and Patent Term Restoration Act of 1984, although certain Tylenol preparations were protected until 2007. U.S. patent 6,126,967 filed September 3, 1998 was granted for "Extended release acetaminophen particles".
Chemistry
Structure and reactivity


Paracetamol consists of a benzene ring core, substituted by one hydroxyl group and the nitrogen atom of an amide group in the para (1,4) pattern. The amide group is acetamide (ethanamide). It is an extensively conjugated system, as the lone pair on the hydroxyl oxygen, the benzene pi cloud, the nitrogen lone pair, the p orbital on the carbonyl carbon, and the lone pair on the carbonyl oxygen are all conjugated. The presence of two activating groups also make the benzene ring highly reactive toward electrophilic aromatic substitution. As the substituents are ortho,para-directing and para with respect to each other, all positions on the ring are more or less equally activated. The conjugation also greatly reduces the basicity of the oxygens and the nitrogen, while making the hydroxyl acidic through delocalisation of charge developed on the phenoxide anion.
Synthesis
From the starting material phenol, paracetamol can be made in the following manner:
- Phenol is nitrated using sulfuric acid and sodium nitrate (as phenol is highly activated, its nitration requires very mild conditions compared to the oleum-fuming nitric acid mixture required to nitrate benzene).
- The para isomer is separated from the ortho isomer by fractional distillation (there will be little of meta, as OH is o-p directing).
- The 4-nitrophenol is reduced to 4-aminophenol using a reducing agent such as sodium borohydride in basic medium.
- 4-aminophenol is reacted with acetic anhydride to give paracetamol.
Note that the synthesis of paracetamol lacks one very significant difficulty inherent in almost all drug syntheses: Lack of stereocenters means there is no need to design a stereo-selective synthesis. More efficient, industrial syntheses are also available.
Available forms


Panadol, which is marketed in Europe, Africa, Asia, Central America, and Australasia, is the most widely available brand, sold in over 80 countries. In North America, paracetamol is sold in generic form (usually labeled as acetaminophen) or under a number of trade names, for instance, Tylenol (McNeil-PPC, Inc.), Anacin-3, Tempra, and Datril. While there is brand named paracetamol available in the UK (e.g. Panadol), unbranded or generic paracetamol is more commonly sold.
In some formulations, paracetamol is combined with the opioid codeine, sometimes referred to as co-codamol (BAN). In the United States and Canada, this is marketed under the name of Tylenol #1/2/3/4, which contain approximately 1/8 grain, approximately 1/4 grain, approximately 1/2 grain, and approximately 1 grain of codeine, respectively. A US grain is 64.78971 milligrams—this is usually rounded in manufacture down to a multiple of 5 mg (so that a #3 contains 30 mg, and a #4 contains 60 mg, while a #1 may be 8 mg or 10 mg depending on manufacturer). In the U.S., this combination is available only by prescription, while the lowest-strength preparation is over-the-counter in Canada, and, in other countries, other strengths may be available over the counter. There are generics as well. In the UK and in many other countries, this combination is marketed under the names of Tylex CD and Panadeine. Other names include Captin, Disprol, Dymadon, Fensum, Hedex, Mexalen, Nofedol, Paralen, Pediapirin, Perfalgan, and Solpadeine. Paracetamol is also combined with other opioids such as dihydrocodeine, referred to as co-dydramol (BAN), oxycodone or hydrocodone, marketed in the U.S. as Percocet and Vicodin, respectively. Another very commonly used analgesic combination includes paracetamol in combination with propoxyphene napsylate, sold under the brand name Darvocet. A combination of paracetamol, codeine, and the calmative doxylamine succinate is marketed as Syndol or Mersyndol.
Paracetamol is commonly used in multi-ingredient preparations for migraine headache, typically including butalbital and paracetamol with or without caffeine, and sometimes containing codeine.
It is commonly administered in tablet, liquid suspension, suppository, intravenous, or intramuscular form. The common adult dose is 500 mg to 1000 mg. The recommended maximum daily dose, for adults, is 4 grams. In recommended doses, paracetamol generally is safe for children and infants, as well as for adults.
| Brand Names[15] |
|---|
| Aceta, Actimin, Anacin-3, Apacet, Aspirin Free Anacin, Atasol, Banesin, Crocin, Dapa, Datril Extra-Strength, Feverall, Few Drops, Fibi, Fibi plus, Genapap, Genebs, Lekadol, Liquiprin, Neopap, Oraphen-PD, Panadol, Paralen, Phenaphen, Redutemp, Snaplets-FR, Suppap, Tapanol, Tylenol, Valorin, Xcel. |
Mechanism of action
The mechanism by which paracetamol reduces fever and pain is still a source of debate.[16] The reason for this confusion has largely been due to the fact that paracetamol reduces the production of prostaglandins (pro-inflammatory chemicals). Aspirin also inhibits the production of prostaglandins, but, unlike aspirin, paracetamol has little anti-inflammatory action. Likewise, whereas aspirin inhibits the production of the pro-clotting chemicals thromboxanes, paracetamol does not. Aspirin is known to inhibit the cyclooxygenase (COX) family of enzymes, and, because of paracetamol's partial similarity of aspirin's action, much research has focused on whether paracetamol also inhibits COX. It is now clear, however, that paracetamol acts via (at least) two pathways.[17][18][19][20]
The COX family of enzymes are responsible for the metabolism of arachidonic acid to prostaglandin H2, an unstable molecule, which is, in turn, converted to numerous other pro-inflammatory compounds. Classical anti-inflammatories, such as the NSAIDs, block this step. Only when appropriately oxidized is the COX enzyme highly active.[21][22] It has been shown that paracetamol reduces the oxidized form of the COX enzyme, preventing it from forming pro-inflammatory chemicals.[18][23]
Further research has shown that paracetamol also modulates the endogenous cannabinoid system.[24] Paracetamol is metabolized to AM404, a compound with several actions; most important, it inhibits the uptake of the endogenous cannabinoid/vanilloid anandamide by neurons. Anandamide uptake would result in the activation of the main pain receptor (nociceptor) of the body, the TRPV1 (older name: vanilloid receptor). Furthermore, AM404 inhibits sodium channels, similarly to the anesthetics lidocaine and procaine.[25] Either of these actions by themselves has been shown to reduce pain, and are a possible mechanism for paracetamol, though it has been demonstrated that, after blocking cannabinoid receptors and hence making any action of cannabinoid reuptake irrelevant, paracetamol no longer has any analgesic effect, suggesting its pain-relieving action is indeed mediated by the endogenous cannabinoid system.[26]
One theory holds that paracetamol works by inhibiting the COX-3 isoform of the cyclooxygenase family of enzymes. This enzyme, when expressed in dogs, shares a strong similarity to the other COX enzymes, produces pro-inflammatory chemicals, and is selectively inhibited by paracetamol.[27] However, some research has suggested that in humans and mice, the COX-3 enzyme is without inflammatory action.[17] Another possibility is that paracetamol is able to block cycloxygenase as in aspirin, but that in an inflammatory environment, where the concentration of peroxides is high, the oxidation state of paracetamol is high which prevents its actions. This would mean that paracetamol has no direct effect at the site of inflammation but instead acts in the CNS to reduce temperature etc where the environment is not oxidative.[27] The exact mechanism by which paracetamol is believed to affect COX-3 is still disputed by some research.
Metabolism

Paracetamol is metabolised primarily in the liver, where its major metabolites include inactive sulfate and glucuronide conjugates, which are excreted by the kidneys. Only a small, yet significant amount is metabolised via the hepatic cytochrome P450 enzyme system (its CYP2E1 and CYP1A2 isoenzymes), which is responsible for the toxic effects of paracetamol due to a minor alkylating metabolite (N-acetyl-p-benzo-quinone imine, abbreviated as NAPQI).[28] There is a great deal of polymorphism in the P450 gene, and genetic polymorphisms in CYP2D6 have been studied extensively. The population can be divided into "extensive", "ultrarapid", and "poor metabolizers" depending on their levels of CYP2D6 expression. CYP2D6 may also contribute to the formation of NAPQI, albeit to a lesser extent than other P450 isozymes, and its activity may contribute to paracetamol toxicity, in particular, in extensive and ultrarapid metabolizers and when paracetamol is taken at very large doses.[29]
The metabolism of paracetamol is an excellent example of toxication, because the metabolite NAPQI is primarily responsible for toxicity rather than paracetamol itself. At usual doses in persons with a common phenotype, the toxic metabolite NAPQI is quickly detoxified by combining irreversibly with the sulfhydryl groups of glutathione to produce a non-toxic conjugate that is eventually excreted by the kidneys.[28] This route becomes saturated following overdose.
Comparison with NSAIDs
Paracetamol, unlike other common analgesics such as aspirin and ibuprofen, has relatively little anti-inflammatory activity, and so it is not considered to be a non-steroidal anti-inflammatory drug (NSAID).
Efficacy
Regarding comparative efficacy, studies show conflicting results when compared to NSAIDs. A randomized controlled trial of chronic pain from osteoarthritis in adults found similar benefit from paracetamol and ibuprofen.[30] However, a randomized controlled trial of acute musculoskeletal pain in children found that the standard OTC dose of ibuprofen gives greater relief of pain than the standard dose of paracetamol.[31]
Adverse effects
In recommended doses, paracetamol does not irritate the lining of the stomach, affect blood coagulation as much as NSAIDs, or affect function of the kidneys. However, some studies have shown that high dose-usage (greater than 2,000 mg per day) does increase the risk of upper gastrointestinal complications such as stomach bleeding.[32]
Paracetamol is safe in pregnancy, and does not affect the closure of the fetal ductus arteriosus as NSAIDs can. Unlike aspirin, it is safe in children, as paracetamol is not associated with a risk of Reye's syndrome in children with viral illnesses.
Like NSAIDs and unlike opioid analgesics, paracetamol has not been found to cause euphoria or alter mood in any way. While paracetamol and NSAIDs may damage the liver, they do not pose a large risk of addiction, dependence, tolerance, and withdrawal.
Paracetamol, particularly in combination with weak opioids, is more likely than NSAIDs to cause rebound headache (medication overuse headache), although less of a risk than ergotamine or triptans used for migraines.[33]
A 2008 preliminary case-control study based on a parent survey presented evidence that paracetamol following MMR vaccination is apparently associated with development of autism in children aged 1–5 years. The effect seemed to appear only in children who show some post-vaccination regression together with other post-vaccination sequelae such as fever, and it was not seen with other painkillers such as ibuprofen. The effect has not been independently confirmed.[34]
Toxicity
Excessive use of paracetamol can damage multiple organs, especially the liver and kidney. In both organs, toxicity from paracetamol is not from the drug itself but from one of its metabolites, N-acetyl-p-benzoquinoneimine (NAPQI). In the liver, the cytochrome P450 enzymes CYP2E1 and CYP3A4 are primarily responsible for the conversion of paracetamol to NAPQI. In the kidney, cyclooxygenases are the principal route by which paracetamol is converted to NAPQI.[35]
Paracetamol overdose leads to the accumulation of NAPQI, which undergoes conjugation with glutathione. Conjugation depletes glutathione, a natural antioxidant. This in combination with direct cellular injury by NAPQI, leads to cell damage and death. These injuries are known as paracetamol hepatotoxicity and analgesic nephropathy in the liver and kidney, respectively.
Signs and symptoms of phenacetin toxicity may initially be absent or vague. Untreated, overdose can lead to liver failure and death within days. Paracetamol hepatotoxicity is, by far, the most common cause of acute liver failure in both the United States and the United Kingdom.[6][36] Paracetamol overdose results in more calls to poison control centers in the US than overdose of any other pharmacological substance.[37]
Effects on animals
Paracetamol is extremely toxic to cats, and should not be given to them under any circumstances. Cats lack the necessary glucuronyl transferase enzymes to safely break paracetamol down, and minute portions of a tablet may prove fatal.[38] Initial symptoms include vomiting, salivation and discolouration of the tongue and gums. After around two days, liver damage is evident, typically giving rise to jaundice. Unlike an overdose in humans, liver damage is rarely the cause of death; instead, methaemoglobin formation and the production of Heinz bodies in red blood cells inhibit oxygen transport by the blood, causing asphyxiation. Effective treatment is occasionally possible for small doses, but must be extremely rapid.
In dogs, paracetamol is a useful anti-inflammatory with a good safety record, causing a lower incidence of gastric ulceration than NSAIDs. It should be administered only on veterinary advice. A paracetamol-codeine product (trade name Pardale-V)[39] licensed for use in dogs is available on veterinary prescription in the UK.[40]
Any cases of suspected ingestion in cats or overdose in dogs should be taken to a veterinarian immediately for detoxification.[41] The effects of toxicity can include liver damage, haemolytic anaemia, oxidative damage to the red blood cells and bleeding tendencies. There are no home remedies, and the amount of irreversible liver failure is dependent on how quickly veterinary intervention begins. Treatment of paracetamol overdose by a veterinarian may involve the use of supportive fluid therapy, acetylcysteine (trade name Mucomyst), methionine, or S-adenosyl-L-methionine (SAMe) to slow liver damage, and cimetidine (trade name Tagamet) to protect against gastric ulceration. Once liver damage has occurred, it cannot be reversed. [42] Vitamin C can be used to aid in the conversion of methemoglobine back to hemoglobine (6 x 30mg/kg every 6 hours).
Paracetamol is also lethal to snakes, and has been used in attempts to control the brown tree snake (Boiga irregularis) in Guam.[43]
See also
- List of paracetamol brand names
- Tylenol scare
- AM404
- NAPQI
- Acetaminophen toxicity
Notes and references
- ↑ [1]
- ↑ Control of Pain in Patients with Cancer Sign Guidelines 40Section 6 [2].
- ↑ Daly FF, Fountain JS, Murray L, Graudins A, Buckley NA (March 2008). "Guidelines for the management of paracetamol poisoning in Australia and New Zealand—explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres". Med. J. Aust. 188 (5): 296–301. PMID 18312195. http://www.mja.com.au/public/issues/188_05_030308/dal10916_fm.html.
- ↑ Khashab M, Tector AJ, Kwo PY (March 2007). "Epidemiology of acute liver failure". Curr Gastroenterol Rep 9 (1): 66–73. PMID 17335680.
- ↑ Hawkins LC, Edwards JN, Dargan PI (2007). "Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature". Drug Saf 30 (6): 465–79. PMID 17536874.
- ↑ 6.0 6.1 Larson AM, Polson J, Fontana RJ, et al (2005). "Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study". Hepatology 42 (6): 1364–72. doi:. PMID 16317692.
- ↑ Laurance, Jeremy (September 19, 2008). "Paracetamol given to babies is linked to global rise in asthma", The Independent. Retrieved on 2008-09-19.
- ↑ Beasley, Richard; Clayton, Tadd; Crane, Julian; von Mutius, Erika; Lai, Christopher; Montefort, Stephen; Stewart, Alistair (2008). "Association between paracetamol use in infancy and childhood, and risk of asthma, rhinoconjunctivitis, and eczema in children aged 6–7 years: analysis from Phase Three of the ISAAC programme.". The Lancet 372: 1039-1048. http://www.thelancet.com/journals/lancet/article/PIIS0140673608614452/abstract. Retrieved on 2008-09-19.
- ↑ "Baby paracetamol asthma concern", BBC News (2008-09-19). Retrieved on 2008-09-19.
- ↑ Gormley, James J. "White willow bark is a gentle, effective pain-reliever." Better Nutrition. March, 1996. Retrieved on August 17, 2007.
- ↑ "The Aspirin story". Did You Know?.
- ↑ H. N. Morse (1878). "Ueber eine neue Darstellungsmethode der Acetylamidophenole". Berichte der deutschen chemischen Gesellschaft 11 (1): 232–233. doi:.
- ↑ Brodie BB, Axelrod J (1948). "The fate of acetanilide in man" (PDF). J Pharmacol Exp Ther 94 (1): 29–38. http://profiles.nlm.nih.gov/HH/A/A/A/D/_/hhaaad.pdf.
- ↑ "A Festival of Analgesics." Chemical Heritage Foundation. 2001. Retrieved on August 17, 2007.
- ↑ Reader's Digest Guide to Drugs and Supplements. Pleasantville, New York; Montreal: Reader's Digest Association, Inc.. 2002. ISBN 0-7621-0366-3.
- ↑ Rossi, S. (ed.) (2008). Australian Medicines Handbook 2008. Adelaide: Australian Medicines Handbook. ISBN 0-9757919-6-7. http://www.amh.net.au.
- ↑ 17.0 17.1 Kis B, Snipes JA, Busija DW (2005). "Acetaminophen and the cyclooxygenase-3 puzzle: sorting out facts, fictions, and uncertainties". J. Pharmacol. Exp. Ther. 315 (1): 1–7. doi:. PMID 15879007.
- ↑ 18.0 18.1 Aronoff DM, Oates JA, Boutaud O (2006). "New insights into the mechanism of action of acetaminophen: Its clinical pharmacologic characteristics reflect its inhibition of the two prostaglandin H2 synthases". Clin. Pharmacol. Ther. 79 (1): 9–19. doi:. PMID 16413237.
- ↑ Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S (2006). "Paracetamol: new vistas of an old drug". CNS drug reviews 12 (3–4): 250–75. doi:. PMID 17227290.
- ↑ Graham GG, Scott KF (2005). "Mechanism of action of paracetamol". American journal of therapeutics 12 (1): 46–55. doi:. PMID 15662292.
- ↑ Ohki S, Ogino N, Yamamoto S, Hayaishi O (1979). "Prostaglandin hydroperoxidase, an integral part of prostaglandin endoperoxide synthetase from bovine vesicular gland microsomes". J. Biol. Chem. 254 (3): 829–36. PMID 104998.
- ↑ Harvison PJ, Egan RW, Gale PH, Nelson SD (1986). "Acetaminophen as a cosubstrate and inhibitor of prostaglandin H synthase". Adv. Exp. Med. Biol. 197: 739–47. PMID 3094341.
- ↑ Roberts, L.J II. & Marrow, J.D. "Analgesic-antipyretic and Antiinflammatory Agents and Drugs Employed in the Treatment of Gout" in, "Goodman & Gilman's The Pharmacological Basis of Therapeutics 10th Edition" by Hardman, J.G. & Limbird, L.E. Published by McGraw Hill, 2001, p.687–731.
- ↑ Högestätt ED, Jönsson BA, Ermund A, et al (2005). "Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system". J. Biol. Chem. 280 (36): 31405–12. doi:. PMID 15987694.
- ↑ Köfalvi A (2008). Chapter 9: Alternative interacting sites and novel receptors for cannabinoid ligands. In: 'Cannabinoids and the Brain' Springer-Verlag. pp. 131–160. doi:.
- ↑ Ottani A, Leone S, Sandrini M, Ferrari A, Bertolini A (2006). "The analgesic activity of paracetamol is prevented by the blockade of cannabinoid CB1 receptors". Eur. J. Pharmacol. 531 (1–3): 280–1. doi:. PMID 16438952.
- ↑ 27.0 27.1 Chandrasekharan NV, Dai H, Roos KL, et al (2002). "COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression". Proc. Natl. Acad. Sci. U.S.A. 99 (21): 13926–31. doi:. PMID 12242329.
- ↑ 28.0 28.1 Borne, Ronald F. "Nonsteroidal Anti-inflammatory Drugs" in Principles of Medicinal Chemistry, Fourth Edition. Eds. Foye, William O.; Lemke, Thomas L.; Williams, David A. Published by Williams & Wilkins, 1995. p. 544–545.
- ↑ Dong H, Haining RL, Thummel KE, Rettie AE, Nelson SD (2000). "Involvement of human cytochrome P450 2D6 in the bioactivation of acetaminophen". Drug Metab Dispos 28 (12): 1397–400. PMID 11095574. Free full text
- ↑ Bradley JD, Brandt KD, Katz BP, Kalasinski LA, Ryan SI (1991). "Comparison of an antiinflammatory dose of ibuprofen, an analgesic dose of ibuprofen, and acetaminophen in the treatment of patients with osteoarthritis of the knee". N. Engl. J. Med. 325 (2): 87–91. PMID 2052056.
- ↑ Clark E, Plint AC, Correll R, Gaboury I, Passi B (2007). "A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma". Pediatrics 119 (3): 460–7. doi:. PMID 17332198.
- ↑ García Rodríguez LA, Hernández-Díaz S (December 15, 2000). "The risk of upper gastrointestinal complications associated with nonsteroidal anti-inflammatory drugs, glucocorticoids, acetaminophen, and combinations of these agents". Arthritis Research and Therapy 3: 98. doi:. PMID 11178116.
- ↑ Colás Chacartegui R, Temprano González R, Gómez Arruza C, Muñoz Cacho P, Pascual Gómez J (2005). "[Abuse pattern of analgesics in chronic daily headache: a study in the general population]". Rev Clin Esp 205 (12): 583–87. PMID 16527179.
- ↑ Schultz ST, Klonoff-Cohen HS, Wingard DL, Akshoomoff NA, Macera CA, Ji M (2008). "Acetaminophen (paracetamol) use, measles-mumps-rubella vaccination, and autistic disorder: the results of a parent survey". Autism 12 (3): 293–307. doi:. PMID 18445737.
- ↑ Mohandas J, Duggin GG, Horvath JS, Tiller DJ (November 1981). "Metabolic oxidation of acetaminophen (paracetamol) mediated by cytochrome P-450 mixed-function oxidase and prostaglandin endoperoxide synthetase in rabbit kidney". Toxicol. Appl. Pharmacol. 61 (2): 252–9. PMID 6798713. http://linkinghub.elsevier.com/retrieve/pii/0041-008X(81)90415-4.
- ↑ Ryder SD, Beckingham IJ (2001). "ABC of diseases of liver, pancreas, and biliary system. Other causes of parenchymal liver disease". BMJ 322 (7281): 290–92. doi:. PMID 11157536. [11157536 Free full text]
- ↑ Lee WM (July 2004). "Acetaminophen and the U.S. Acute Liver Failure Study Group: lowering the risks of hepatic failure". Hepatology 40 (1): 6–9. doi:. PMID 15239078. http://www3.interscience.wiley.com/cgi-bin/fulltext/109086434/PDFSTART.
- ↑ Allen AL (2003). "The diagnosis of acetaminophen toxicosis in a cat". Can Vet J 44 (6): 509–10. PMID 12839249.
- ↑ "Pardale-V Tablets: Presentation". UK National Office of Animal Health Compendium of Animal Medicines (September 28, 2006).
- ↑ "Pardale-V Tablets: Legal Category". UK National Office of Animal Health Compendium of Animal Medicines (November 15, 2005).
- ↑ Villar D, Buck WB, Gonzalez JM (1998). "Ibuprofen, aspirin and acetaminophen toxicosis and treatment in dogs and cats". Vet Hum Toxicol 40 (3): 156–62. PMID 9610496.
- ↑ Manning AM. "Acetaminophen Toxicity in Dogs". PetPlace.com.
- ↑ Johnston J, Savarie P, Primus T, Eisemann J, Hurley J, Kohler D (2002). "Risk assessment of an acetaminophen baiting program for chemical control of brown tree snakes on Guam: evaluation of baits, snake residues, and potential primary and secondary hazards". Environ Sci Technol 36 (17): 3827–33. doi:. PMID 12322757.
External links
- List of Paracetamol synonyms
- Paracetamol Information Centre
- U.S. Patent 6,126,967
- The Julius Axelrod Papers
|
|||||||||||||||||||||||||||||||||||||||||||||